Monday Poster Session
Category: IBD
P3342 - Comparing the Rate of Arthralgia Improvement in Patients With Active Inflammatory Bowel Disease Treated With Different Biologics: A Retrospective Multicenter Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bahar Saberzadeh-Ardestani, MD
Yale University School of Medicine
New Haven, CT
Presenting Author(s)
Bahar Saberzadeh-Ardestani, MD1, Noah Fanous, MD2, Barbara Mensah, MD2, Aditya Desai, MD2, Rumzah Paracha, MD1, Chandershekhar Shori, MS3, Sara Sheikh, BS4, Bhuvana Mukkamala, BS4, Linda A. Feagins, MD2, Jill K. J.. Gaidos, MD, FACG5
1Yale University School of Medicine, New Haven, CT; 2University of Texas at Austin Dell Medical School, Austin, TX; 3University of Central Florida College of Medicine, Orlando, FL; 4University of Texas, Austin, TX; 5Yale University, New Haven, CT
Introduction: Musculoskeletal symptoms represent the most common extraintestinal manifestation of IBD; however, there are no guidelines on optimal treatment of arthralgia. The aim of this study was to assess for improvement in joint pain with treatment of active IBD.
Methods: This multicenter retrospective cohort included consecutive patients with IBD seen between 1/1/2020 and 4/15/2023 at two academic centers with at least 12 months of follow up. Objective disease activity was defined as elevated fecal calprotectin ( >250 μg/g) or evidence of disease activity on endoscopy or imaging. The primary end point was improvement in joint pain after initiation of treatment for active IBD at 6 and 12 months after the initial visit. Relative risk was calculated for IBD type (Crohn’s disease (CD vs UC), type of therapy (anti-TNF, vedolizumab, IL12/23 inhibitor, JAK inhibitor), subclinical disease activity at enrollment (Based on HBAI or SSCAI) and GI symptoms resolution in association with rate of arthralgia improvement.
Results: Among the 736 enrolled IBD patients, 385 (52.3%) had objective disease activity at the initial visit. Of these 385 patients with active IBD, 123 (31.9%) reported joint pain. Among those with active IBD and joint pain, 62.5% had CD, 32.5% with UC and 4.9% with IBD-U. The median age was 32 years (IQR, 27-49), 60.2% were female with a median disease duration of 8 years (IQR, 2-16). At 6 months, 66 (56.8%) had resolution of joint pain. Resolution of joint pain was not significantly associated with GI symptom resolution at 6 months (p=0.97). At 12 months, 62 (54.8%) cases had resolution of joint pain. Patients with UC were more likely to have resolution of their pain compared to CD at follow up (RR: 0.59; 95% CI: 0.35-0.99, p: 0.039). Joint location, type of therapy, subclinical disease activity at enrollment and GI symptoms resolution were not significantly associated with improvement in joint pain (all p>0.05).
Discussion: Joint pain affects a notable proportion of IBD patients with active disease, yet our study found that resolution of GI symptom does not consistently lead to improvement in arthralgia symptoms. Neither the type of biologic therapy, joint location, nor subclinical disease activity at enrollment were significantly associated with joint pain improvement, suggesting that management of musculoskeletal symptoms in IBD requires approaches beyond controlling intestinal inflammation alone.
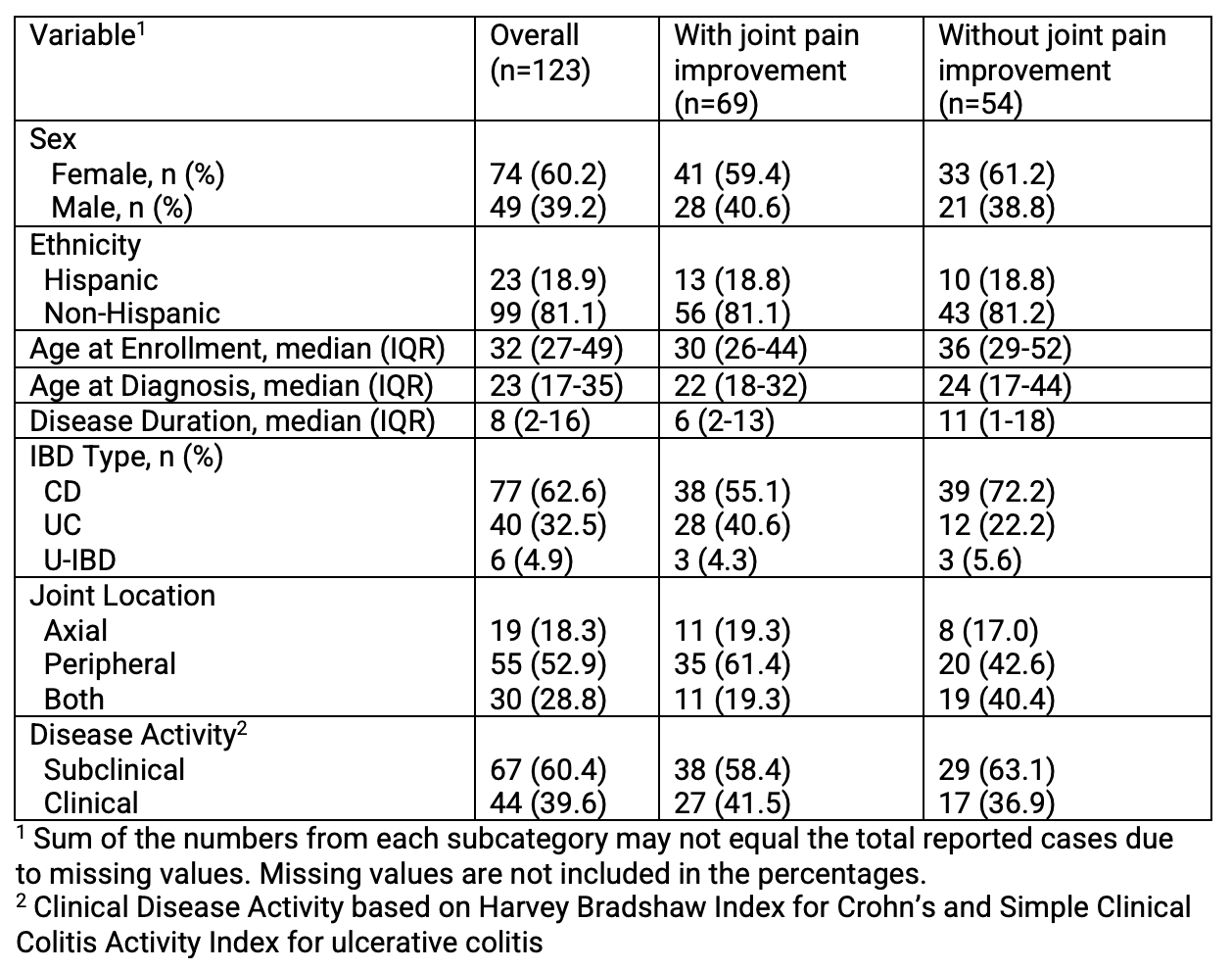
Figure: Table 1. Clinicopathologic Characteristics of Patients at Enrollment with Objective Disease Activity and Joint Pain
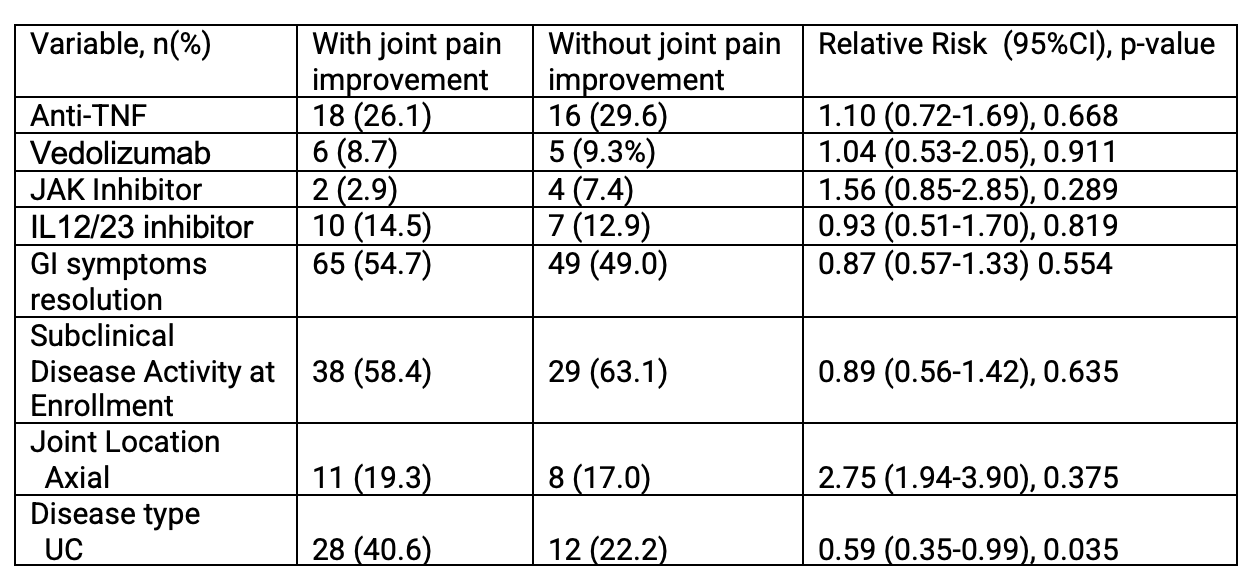
Figure: Table 2. Bivariable Analysis of Variables Associated with Joint Pain Resolution
Disclosures:
Bahar Saberzadeh-Ardestani indicated no relevant financial relationships.
Noah Fanous indicated no relevant financial relationships.
Barbara Mensah indicated no relevant financial relationships.
Aditya Desai indicated no relevant financial relationships.
Rumzah Paracha indicated no relevant financial relationships.
Chandershekhar Shori indicated no relevant financial relationships.
Sara Sheikh indicated no relevant financial relationships.
Bhuvana Mukkamala indicated no relevant financial relationships.
Linda Feagins: Corevitas – Clinical trial participation. Takeda – Clinical trial participation.
Jill Gaidos: Pfizer – Advisory Committee/Board Member.
Bahar Saberzadeh-Ardestani, MD1, Noah Fanous, MD2, Barbara Mensah, MD2, Aditya Desai, MD2, Rumzah Paracha, MD1, Chandershekhar Shori, MS3, Sara Sheikh, BS4, Bhuvana Mukkamala, BS4, Linda A. Feagins, MD2, Jill K. J.. Gaidos, MD, FACG5. P3342 - Comparing the Rate of Arthralgia Improvement in Patients With Active Inflammatory Bowel Disease Treated With Different Biologics: A Retrospective Multicenter Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale University School of Medicine, New Haven, CT; 2University of Texas at Austin Dell Medical School, Austin, TX; 3University of Central Florida College of Medicine, Orlando, FL; 4University of Texas, Austin, TX; 5Yale University, New Haven, CT
Introduction: Musculoskeletal symptoms represent the most common extraintestinal manifestation of IBD; however, there are no guidelines on optimal treatment of arthralgia. The aim of this study was to assess for improvement in joint pain with treatment of active IBD.
Methods: This multicenter retrospective cohort included consecutive patients with IBD seen between 1/1/2020 and 4/15/2023 at two academic centers with at least 12 months of follow up. Objective disease activity was defined as elevated fecal calprotectin ( >250 μg/g) or evidence of disease activity on endoscopy or imaging. The primary end point was improvement in joint pain after initiation of treatment for active IBD at 6 and 12 months after the initial visit. Relative risk was calculated for IBD type (Crohn’s disease (CD vs UC), type of therapy (anti-TNF, vedolizumab, IL12/23 inhibitor, JAK inhibitor), subclinical disease activity at enrollment (Based on HBAI or SSCAI) and GI symptoms resolution in association with rate of arthralgia improvement.
Results: Among the 736 enrolled IBD patients, 385 (52.3%) had objective disease activity at the initial visit. Of these 385 patients with active IBD, 123 (31.9%) reported joint pain. Among those with active IBD and joint pain, 62.5% had CD, 32.5% with UC and 4.9% with IBD-U. The median age was 32 years (IQR, 27-49), 60.2% were female with a median disease duration of 8 years (IQR, 2-16). At 6 months, 66 (56.8%) had resolution of joint pain. Resolution of joint pain was not significantly associated with GI symptom resolution at 6 months (p=0.97). At 12 months, 62 (54.8%) cases had resolution of joint pain. Patients with UC were more likely to have resolution of their pain compared to CD at follow up (RR: 0.59; 95% CI: 0.35-0.99, p: 0.039). Joint location, type of therapy, subclinical disease activity at enrollment and GI symptoms resolution were not significantly associated with improvement in joint pain (all p>0.05).
Discussion: Joint pain affects a notable proportion of IBD patients with active disease, yet our study found that resolution of GI symptom does not consistently lead to improvement in arthralgia symptoms. Neither the type of biologic therapy, joint location, nor subclinical disease activity at enrollment were significantly associated with joint pain improvement, suggesting that management of musculoskeletal symptoms in IBD requires approaches beyond controlling intestinal inflammation alone.
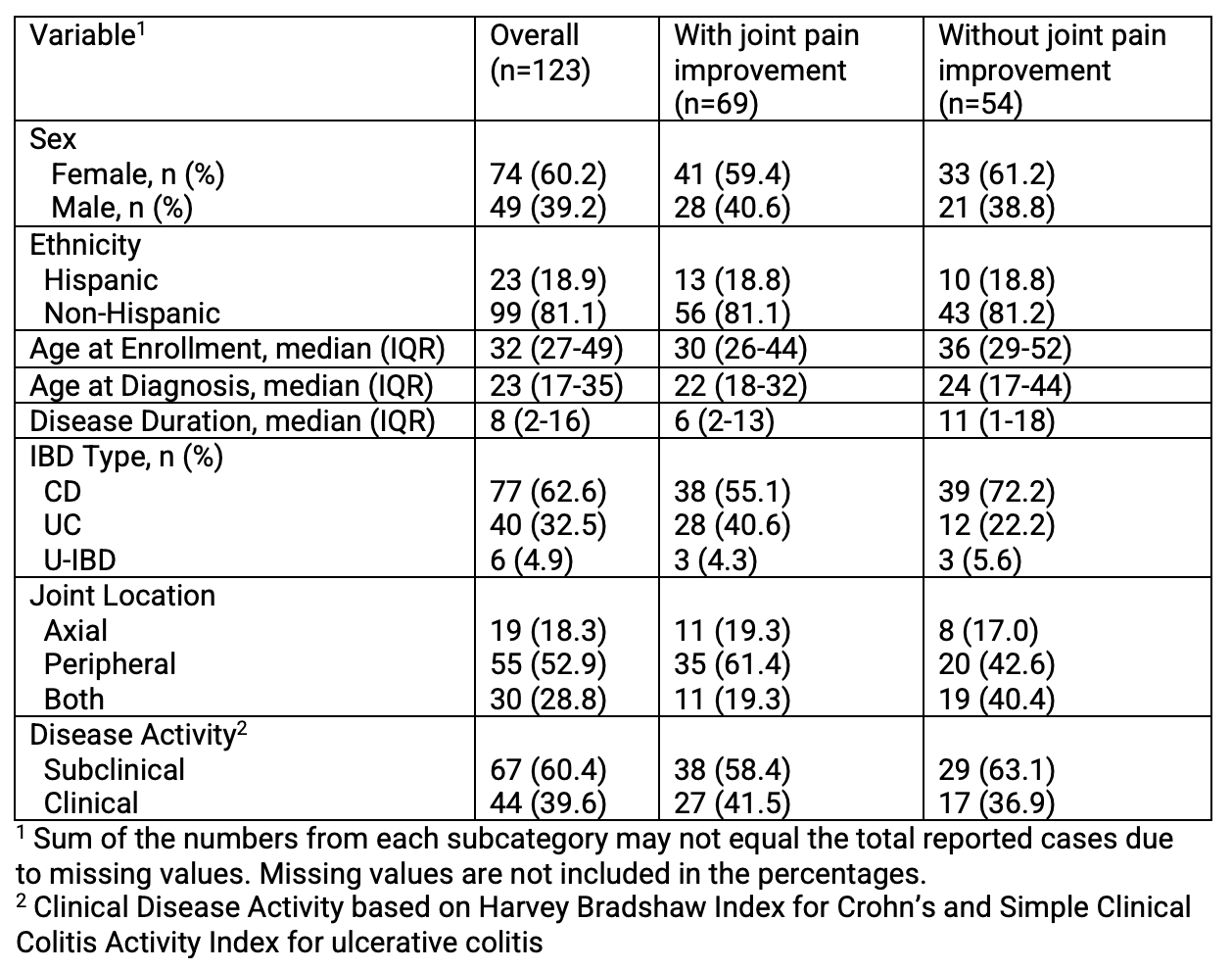
Figure: Table 1. Clinicopathologic Characteristics of Patients at Enrollment with Objective Disease Activity and Joint Pain
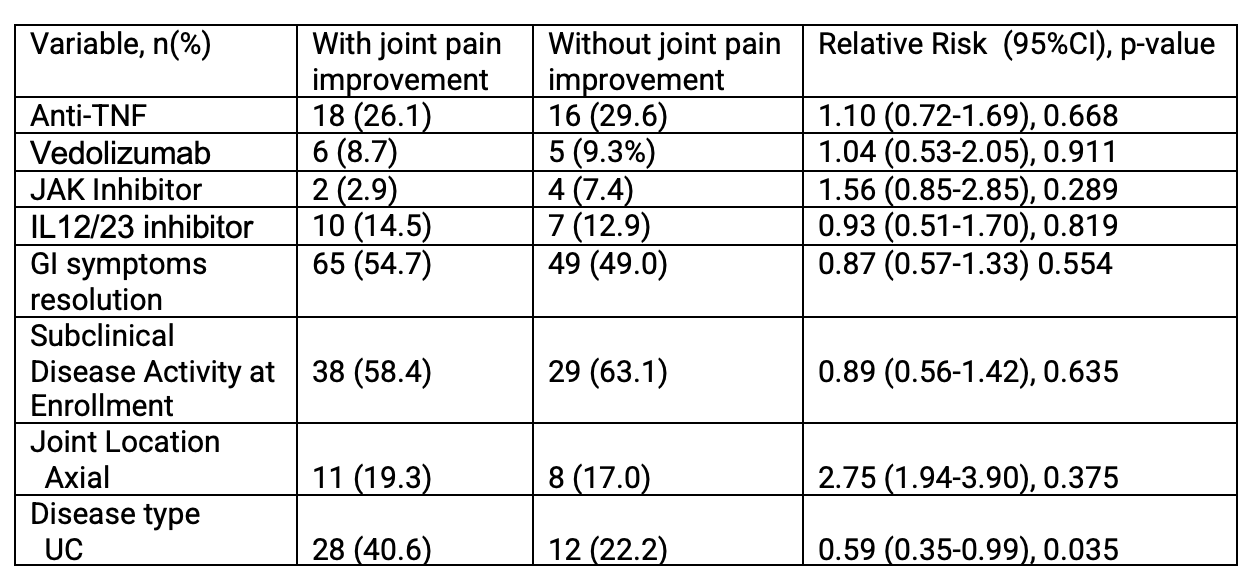
Figure: Table 2. Bivariable Analysis of Variables Associated with Joint Pain Resolution
Disclosures:
Bahar Saberzadeh-Ardestani indicated no relevant financial relationships.
Noah Fanous indicated no relevant financial relationships.
Barbara Mensah indicated no relevant financial relationships.
Aditya Desai indicated no relevant financial relationships.
Rumzah Paracha indicated no relevant financial relationships.
Chandershekhar Shori indicated no relevant financial relationships.
Sara Sheikh indicated no relevant financial relationships.
Bhuvana Mukkamala indicated no relevant financial relationships.
Linda Feagins: Corevitas – Clinical trial participation. Takeda – Clinical trial participation.
Jill Gaidos: Pfizer – Advisory Committee/Board Member.
Bahar Saberzadeh-Ardestani, MD1, Noah Fanous, MD2, Barbara Mensah, MD2, Aditya Desai, MD2, Rumzah Paracha, MD1, Chandershekhar Shori, MS3, Sara Sheikh, BS4, Bhuvana Mukkamala, BS4, Linda A. Feagins, MD2, Jill K. J.. Gaidos, MD, FACG5. P3342 - Comparing the Rate of Arthralgia Improvement in Patients With Active Inflammatory Bowel Disease Treated With Different Biologics: A Retrospective Multicenter Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

