Monday Poster Session
Category: IBD
P3336 - Healthcare Burden of Intestinal Obstruction in Hospitalized Patients With Crohn’s Disease: A Population-Based Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anjul Verma, MD (he/him/his)
Texas Tech University Health Sciences Center
Syracuse, NY
Presenting Author(s)
Anjul Verma, MD1, Avneet Kaur, MBBS2, Guy Loic Nguefang Tchoukeu, MD1, Ooreoluwa Fasola, MD1, Gloria Erazo, MD1, Edgar Luna Landa, MD1, Sameer Rao, MBBS3, Rohit Goyal, MD4, Karan Sachdeva, MD5, Hayden Mathews, BS6, Lauren Glover, 6, Megan Mobley, 6, Sachi Khemka, MBA, BS7, Merry Mathew, BS6, Virginia McGrath, BS6, John Garza, PhD8, Kalyan Chakrala, DO1
1Texas Tech University Health Sciences Center, Odessa, TX; 2SUNY Upstate Medical University, Syracuse, NY; 3Rutgers New Jersey Medical School, Newark, NJ; 4Louisiana State University, Shreveport, LA; 5LSU Health, Shreveport, LA; 6Texas Tech University Health Sciences Center School of Medicine, Odessa, TX; 7Texas Tech University Health Sciences Center, Amarillo, TX; 8Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX
Introduction: Intestinal obstruction is clinically significant complication of Crohn’s disease (CD), often resulting in surgical intervention and increased healthcare utilization. However, population-level data on the impact of obstruction on hospitalization outcomes among patients with CD are limited. We aimed to evaluate the association of intestinal obstruction with hospital length of stay and total charges in a statewide cohort of hospitalized CD patients.
Methods: We performed a population-based cohort study using deidentified, publicly available data from adult hospitalizations to acute care hospitals in Texas (Q1 2016–Q2 2024). Patients with Crohn’s disease (CD) were identified using ICD-10-CM codes K52.0x under CCSR category DIG011. Elective admissions and interhospital transfers were excluded. The primary exposure was CD with intestinal obstruction (DIG012). The primary outcomes were length of stay and inflation-adjusted total hospital charges. Overlap propensity score weighting was applied; results are reported as adjusted risk ratios (aRR) with 95% confidence intervals (CI).
Results: Among 78,858 hospitalizations with Crohn’s disease, 7,651 (9.7%) had a diagnosis of intestinal obstruction. These patients were younger (≥65 years: 19.1% vs 31.4%), more often male (43.5% vs 34.1%), and had a lower comorbidity burden. They also had lower rates of ICU admission (17.0% vs 31.5%) and fewer comorbid conditions, including diabetes, cardiovascular, and renal disease (p < 0.0001). Despite lower baseline acuity, obstruction was associated with significantly increased healthcare utilization: in the overlap-weighted cohort, obstruction was linked to longer hospital stay (mean 5.70 vs 4.55 days; aRR 1.25, 95% CI 1.22–1.29) and higher total charges. These associations remained consistent across subgroups including elderly patients, emergency admissions, and ICU stays. Hospitalizations with obstruction also had higher rates of intestinal procedures but were more often discharged home (86.6% vs 72.2%) and less likely to require chronic care (2.9% vs 10.0%).
Discussion: In a large population-based cohort of hospitalized Crohn’s disease patients, intestinal obstruction was associated with significantly longer hospital stays and higher total charges, despite a lower burden of baseline comorbidity. These findings highlight the disproportionate healthcare impact of obstruction and underscore the need for timely recognition and targeted interventions to mitigate its clinical and economic burden.
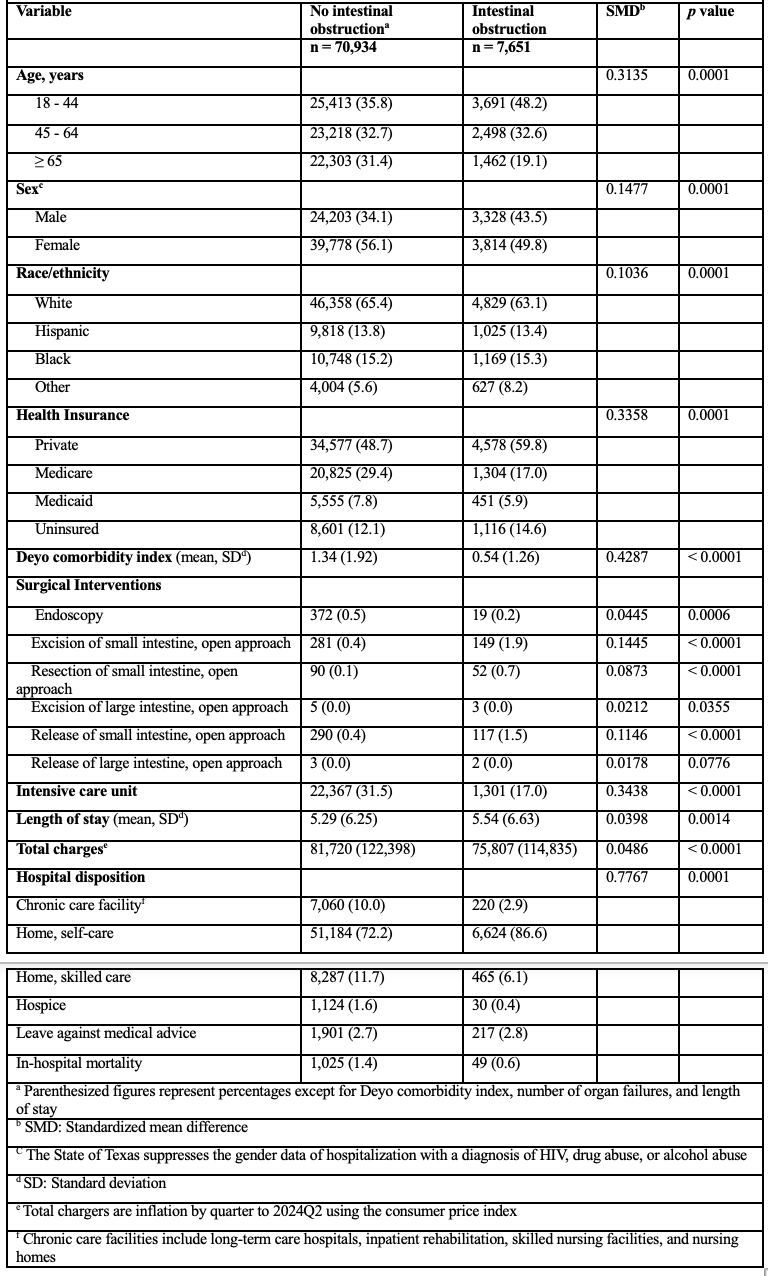
Figure: The characteristics and outcomes of Crohn's disease patients with and without intestinal obstruction
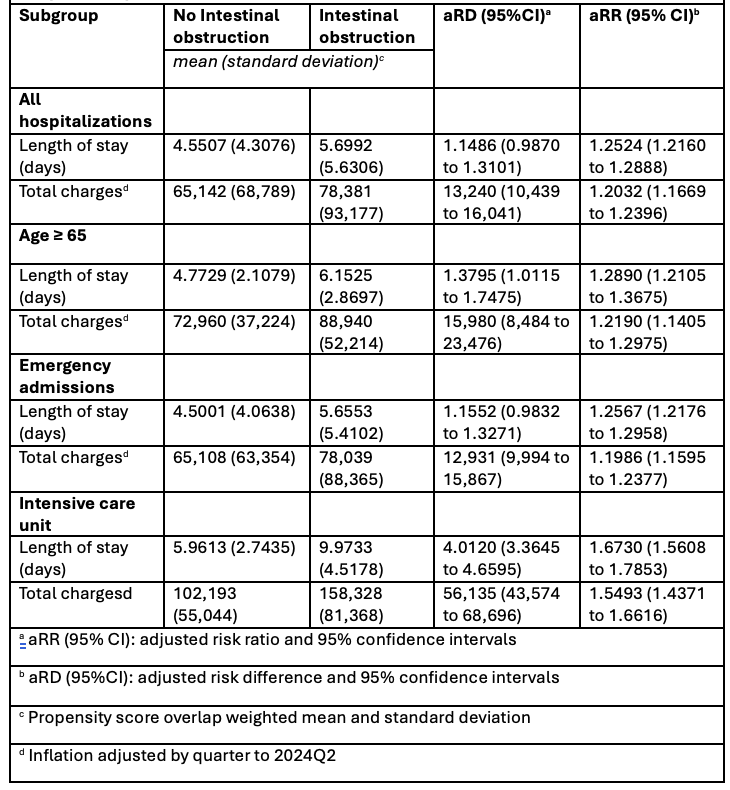
Figure: The association of intestinal obstruction and resource utilizations among hospitalized patients with Crohn's disease
Disclosures:
Anjul Verma indicated no relevant financial relationships.
Avneet Kaur indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Ooreoluwa Fasola indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Edgar Luna Landa indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Karan Sachdeva indicated no relevant financial relationships.
Hayden Mathews indicated no relevant financial relationships.
Lauren Glover indicated no relevant financial relationships.
Megan Mobley indicated no relevant financial relationships.
Sachi Khemka indicated no relevant financial relationships.
Merry Mathew indicated no relevant financial relationships.
Virginia McGrath indicated no relevant financial relationships.
John Garza indicated no relevant financial relationships.
Kalyan Chakrala indicated no relevant financial relationships.
Anjul Verma, MD1, Avneet Kaur, MBBS2, Guy Loic Nguefang Tchoukeu, MD1, Ooreoluwa Fasola, MD1, Gloria Erazo, MD1, Edgar Luna Landa, MD1, Sameer Rao, MBBS3, Rohit Goyal, MD4, Karan Sachdeva, MD5, Hayden Mathews, BS6, Lauren Glover, 6, Megan Mobley, 6, Sachi Khemka, MBA, BS7, Merry Mathew, BS6, Virginia McGrath, BS6, John Garza, PhD8, Kalyan Chakrala, DO1. P3336 - Healthcare Burden of Intestinal Obstruction in Hospitalized Patients With Crohn’s Disease: A Population-Based Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Odessa, TX; 2SUNY Upstate Medical University, Syracuse, NY; 3Rutgers New Jersey Medical School, Newark, NJ; 4Louisiana State University, Shreveport, LA; 5LSU Health, Shreveport, LA; 6Texas Tech University Health Sciences Center School of Medicine, Odessa, TX; 7Texas Tech University Health Sciences Center, Amarillo, TX; 8Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX
Introduction: Intestinal obstruction is clinically significant complication of Crohn’s disease (CD), often resulting in surgical intervention and increased healthcare utilization. However, population-level data on the impact of obstruction on hospitalization outcomes among patients with CD are limited. We aimed to evaluate the association of intestinal obstruction with hospital length of stay and total charges in a statewide cohort of hospitalized CD patients.
Methods: We performed a population-based cohort study using deidentified, publicly available data from adult hospitalizations to acute care hospitals in Texas (Q1 2016–Q2 2024). Patients with Crohn’s disease (CD) were identified using ICD-10-CM codes K52.0x under CCSR category DIG011. Elective admissions and interhospital transfers were excluded. The primary exposure was CD with intestinal obstruction (DIG012). The primary outcomes were length of stay and inflation-adjusted total hospital charges. Overlap propensity score weighting was applied; results are reported as adjusted risk ratios (aRR) with 95% confidence intervals (CI).
Results: Among 78,858 hospitalizations with Crohn’s disease, 7,651 (9.7%) had a diagnosis of intestinal obstruction. These patients were younger (≥65 years: 19.1% vs 31.4%), more often male (43.5% vs 34.1%), and had a lower comorbidity burden. They also had lower rates of ICU admission (17.0% vs 31.5%) and fewer comorbid conditions, including diabetes, cardiovascular, and renal disease (p < 0.0001). Despite lower baseline acuity, obstruction was associated with significantly increased healthcare utilization: in the overlap-weighted cohort, obstruction was linked to longer hospital stay (mean 5.70 vs 4.55 days; aRR 1.25, 95% CI 1.22–1.29) and higher total charges. These associations remained consistent across subgroups including elderly patients, emergency admissions, and ICU stays. Hospitalizations with obstruction also had higher rates of intestinal procedures but were more often discharged home (86.6% vs 72.2%) and less likely to require chronic care (2.9% vs 10.0%).
Discussion: In a large population-based cohort of hospitalized Crohn’s disease patients, intestinal obstruction was associated with significantly longer hospital stays and higher total charges, despite a lower burden of baseline comorbidity. These findings highlight the disproportionate healthcare impact of obstruction and underscore the need for timely recognition and targeted interventions to mitigate its clinical and economic burden.
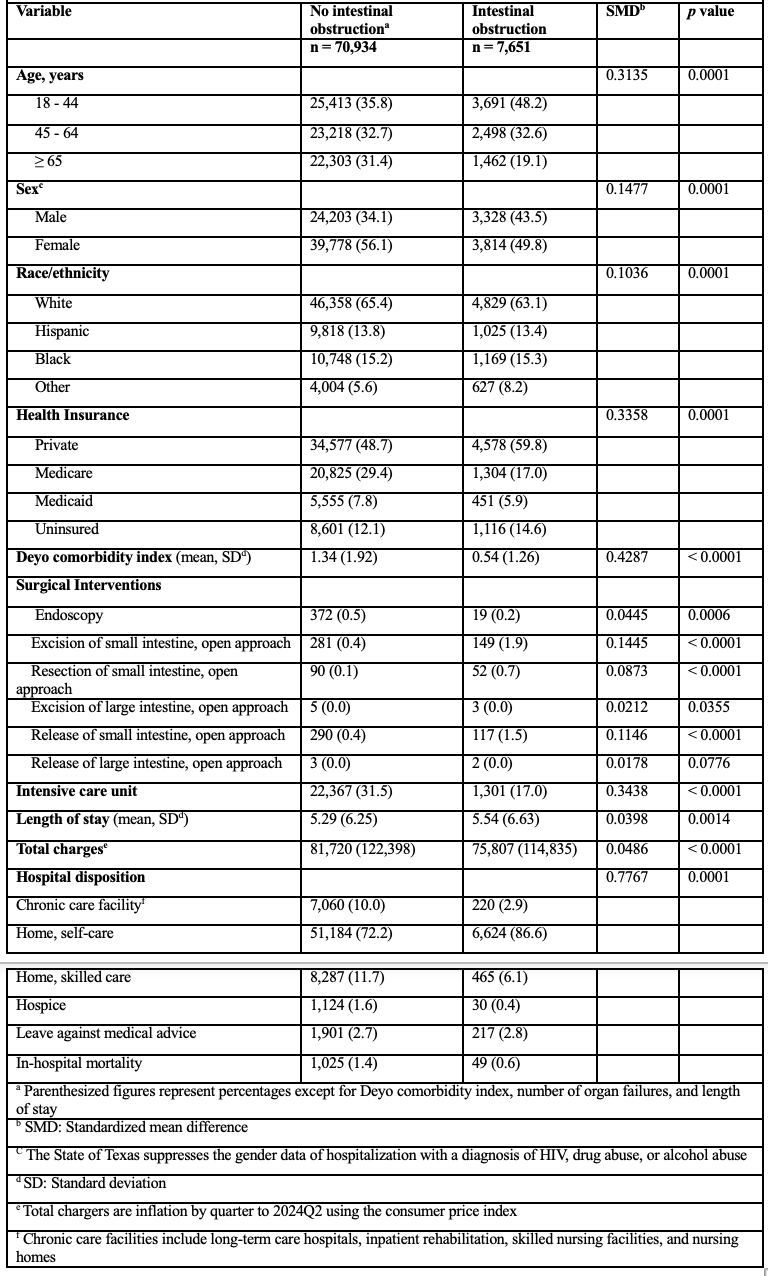
Figure: The characteristics and outcomes of Crohn's disease patients with and without intestinal obstruction
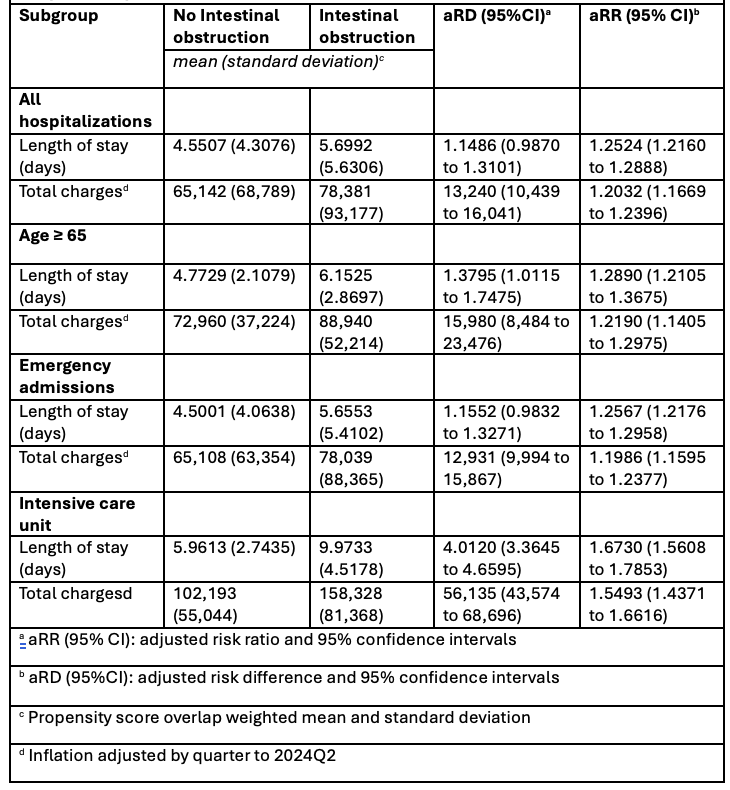
Figure: The association of intestinal obstruction and resource utilizations among hospitalized patients with Crohn's disease
Disclosures:
Anjul Verma indicated no relevant financial relationships.
Avneet Kaur indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Ooreoluwa Fasola indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Edgar Luna Landa indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Karan Sachdeva indicated no relevant financial relationships.
Hayden Mathews indicated no relevant financial relationships.
Lauren Glover indicated no relevant financial relationships.
Megan Mobley indicated no relevant financial relationships.
Sachi Khemka indicated no relevant financial relationships.
Merry Mathew indicated no relevant financial relationships.
Virginia McGrath indicated no relevant financial relationships.
John Garza indicated no relevant financial relationships.
Kalyan Chakrala indicated no relevant financial relationships.
Anjul Verma, MD1, Avneet Kaur, MBBS2, Guy Loic Nguefang Tchoukeu, MD1, Ooreoluwa Fasola, MD1, Gloria Erazo, MD1, Edgar Luna Landa, MD1, Sameer Rao, MBBS3, Rohit Goyal, MD4, Karan Sachdeva, MD5, Hayden Mathews, BS6, Lauren Glover, 6, Megan Mobley, 6, Sachi Khemka, MBA, BS7, Merry Mathew, BS6, Virginia McGrath, BS6, John Garza, PhD8, Kalyan Chakrala, DO1. P3336 - Healthcare Burden of Intestinal Obstruction in Hospitalized Patients With Crohn’s Disease: A Population-Based Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
