Monday Poster Session
Category: IBD
P3329 - Does Thrombosis Drive Worse Clinical and Economic Outcomes in Hospitalized Inflammatory Bowel Disease Patients? A High-Risk Phenotype Revealed Through National Hospitalization Trends
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Silpa Choday, MD (she/her/hers)
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Silpa Choday, MD1, Sunanda Ellina, MD1, Gautam Maddineni, MD2, Tamer Zahdeh, MD3, Akanksha Togra, MD4, Keng-Yu Chuang, MD5, Neil Vyas, MD1, Savio Reddymasu, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Florida State University, Cape Coral, FL; 3Montefiore Medical Center, New York, NY; 4Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 5GI Alliance, Phoenix, AZ
Introduction: Inflammatory Bowel Disease (IBD) is associated with an elevated risk of thromboembolic events due to chronic systemic inflammation and disrupted coagulation pathways. This study evaluates national trends in IBD-related hospitalizations with and without thrombosis.
Methods: A retrospective cohort analysis was conducted using the Nationwide Inpatient Sample from 2016 to 2021. Adult patients hospitalized with IBD were stratified based on the presence of thrombotic complications. Total hospital costs are adjusted for inflation to 2021 USD using the Consumer Price Index.
Results: A total of 52,345 hospitalizations for IBD with thrombosis and 565,600 without thrombosis were analyzed. Patients with IBD and thrombosis were older (mean age: 48 vs. 42 years), predominantly female (75% vs. 32%), and more racially diverse compared to those without thrombosis (White: 50%, Black: 25%, Other: 25% vs. White: 90%, Black: 5%, Other: 5%).
Among patients with IBD and thrombosis, the prevalence of phlebitis, thrombophlebitis, and embolism was 15%, compared to zero in those without thrombosis. These patients also had higher rates of long-term steroid use (8% vs. 6.2%), postprocedural complications (2% vs. 0%), sepsis (5% vs. 0%), and presence of vascular implants (37% vs. 0%). Interestingly, there are higher rates of malnutrition (25% vs. 14%), and dehydration (40% vs. 21%) among IBD patients without thrombosis.
The length of hospital stay was significantly longer in patients with thrombosis (mean: 12.25 vs. 7.3 days), with a higher mortality rate (2.2% vs. 0%) and mean total hospital charges ($123,247 vs. $79,173).
Trends over time revealed a statistically significant decline in hospitalizations for both IBD with thrombosis (p = 0.040) and IBD without thrombosis (p = 0.04) from 2016 to 2021. However, the incidence of phlebitis, thrombophlebitis, and embolism showed a marked increase from 0% in 2019 to 29% in 2021, and postprocedural thrombotic complications rose from 1.7% in 2016 to 3% in 2021. Overall, IBD with thrombosis was associated with increased severity, resource utilization, and worse outcomes compared to IBD without thrombosis.
Discussion: IBD patients with thrombosis represent a high-risk subgroup defined by older age, female predominance, and greater racial diversity. This group experiences more complications, higher mortality, longer hospital stays, and significantly greater healthcare costs. While overall IBD hospitalizations declined, thromboembolic events have risen sharply over recent years.
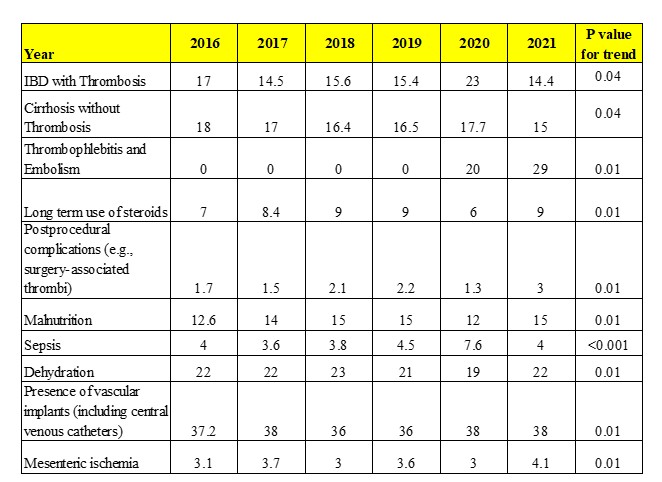
Figure: Table1: Trends of hospitalization of comorbid conditions for IBD with Thrombosis
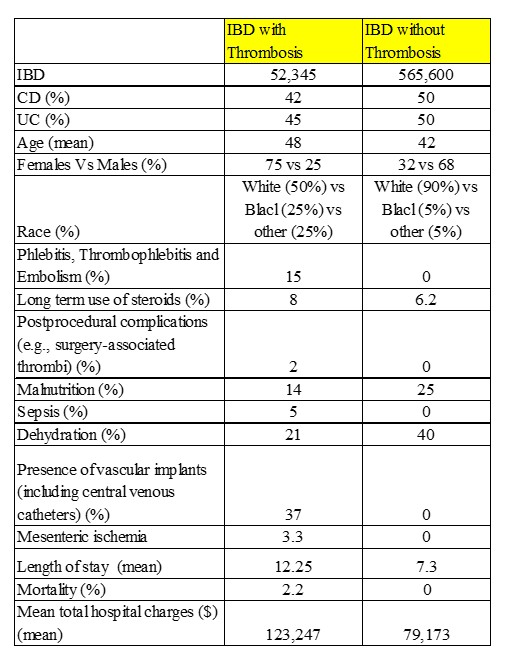
Figure: Table 2: Comparison of IBD with and without Thrombosis
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Sunanda Ellina indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Tamer Zahdeh indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Silpa Choday, MD1, Sunanda Ellina, MD1, Gautam Maddineni, MD2, Tamer Zahdeh, MD3, Akanksha Togra, MD4, Keng-Yu Chuang, MD5, Neil Vyas, MD1, Savio Reddymasu, MD1. P3329 - Does Thrombosis Drive Worse Clinical and Economic Outcomes in Hospitalized Inflammatory Bowel Disease Patients? A High-Risk Phenotype Revealed Through National Hospitalization Trends, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Florida State University, Cape Coral, FL; 3Montefiore Medical Center, New York, NY; 4Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 5GI Alliance, Phoenix, AZ
Introduction: Inflammatory Bowel Disease (IBD) is associated with an elevated risk of thromboembolic events due to chronic systemic inflammation and disrupted coagulation pathways. This study evaluates national trends in IBD-related hospitalizations with and without thrombosis.
Methods: A retrospective cohort analysis was conducted using the Nationwide Inpatient Sample from 2016 to 2021. Adult patients hospitalized with IBD were stratified based on the presence of thrombotic complications. Total hospital costs are adjusted for inflation to 2021 USD using the Consumer Price Index.
Results: A total of 52,345 hospitalizations for IBD with thrombosis and 565,600 without thrombosis were analyzed. Patients with IBD and thrombosis were older (mean age: 48 vs. 42 years), predominantly female (75% vs. 32%), and more racially diverse compared to those without thrombosis (White: 50%, Black: 25%, Other: 25% vs. White: 90%, Black: 5%, Other: 5%).
Among patients with IBD and thrombosis, the prevalence of phlebitis, thrombophlebitis, and embolism was 15%, compared to zero in those without thrombosis. These patients also had higher rates of long-term steroid use (8% vs. 6.2%), postprocedural complications (2% vs. 0%), sepsis (5% vs. 0%), and presence of vascular implants (37% vs. 0%). Interestingly, there are higher rates of malnutrition (25% vs. 14%), and dehydration (40% vs. 21%) among IBD patients without thrombosis.
The length of hospital stay was significantly longer in patients with thrombosis (mean: 12.25 vs. 7.3 days), with a higher mortality rate (2.2% vs. 0%) and mean total hospital charges ($123,247 vs. $79,173).
Trends over time revealed a statistically significant decline in hospitalizations for both IBD with thrombosis (p = 0.040) and IBD without thrombosis (p = 0.04) from 2016 to 2021. However, the incidence of phlebitis, thrombophlebitis, and embolism showed a marked increase from 0% in 2019 to 29% in 2021, and postprocedural thrombotic complications rose from 1.7% in 2016 to 3% in 2021. Overall, IBD with thrombosis was associated with increased severity, resource utilization, and worse outcomes compared to IBD without thrombosis.
Discussion: IBD patients with thrombosis represent a high-risk subgroup defined by older age, female predominance, and greater racial diversity. This group experiences more complications, higher mortality, longer hospital stays, and significantly greater healthcare costs. While overall IBD hospitalizations declined, thromboembolic events have risen sharply over recent years.
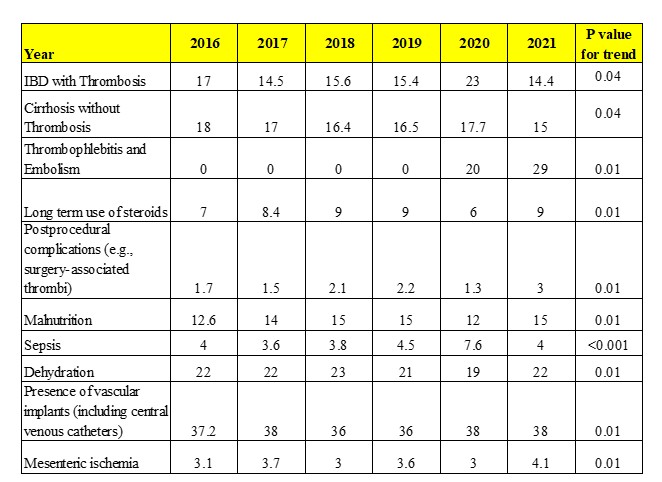
Figure: Table1: Trends of hospitalization of comorbid conditions for IBD with Thrombosis
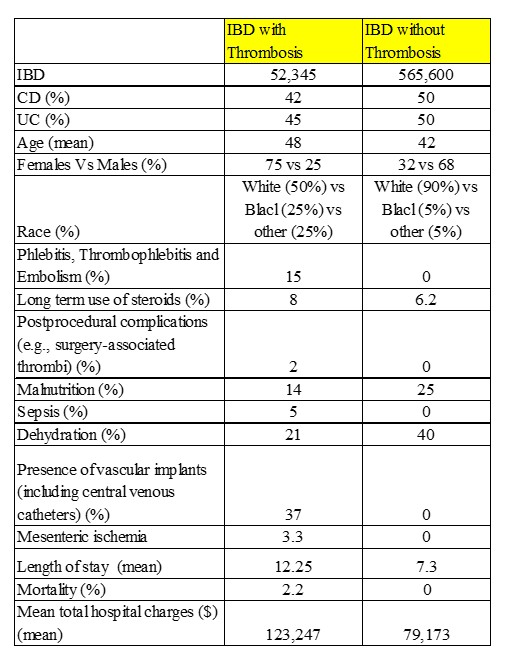
Figure: Table 2: Comparison of IBD with and without Thrombosis
Disclosures:
Silpa Choday indicated no relevant financial relationships.
Sunanda Ellina indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Tamer Zahdeh indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Keng-Yu Chuang indicated no relevant financial relationships.
Neil Vyas indicated no relevant financial relationships.
Savio Reddymasu indicated no relevant financial relationships.
Silpa Choday, MD1, Sunanda Ellina, MD1, Gautam Maddineni, MD2, Tamer Zahdeh, MD3, Akanksha Togra, MD4, Keng-Yu Chuang, MD5, Neil Vyas, MD1, Savio Reddymasu, MD1. P3329 - Does Thrombosis Drive Worse Clinical and Economic Outcomes in Hospitalized Inflammatory Bowel Disease Patients? A High-Risk Phenotype Revealed Through National Hospitalization Trends, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
