Monday Poster Session
Category: IBD
P3314 - Impact of GLP-1 Receptor Agonists on IBD Outcomes in Patients With Diabetes Mellitus: A Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Avneet Kaur, MBBS (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Avneet Kaur, MBBS1, Anjul Verma, MD2, Abdelkader Chaar, MD1, Babu P. Mohan, MD3, Idan Goren, MD1
1SUNY Upstate Medical University, Syracuse, NY; 2Texas Tech University Health Sciences Center, Odessa, TX; 3Orlando Gastroenterology PA, Orlando, FL
Introduction: GLP-1 receptor agonists (GLP-1 RAs) are known for their metabolic benefits in managing diabetes mellitus (DM) and are thought to have anti-inflammatory effects. However, their impact on inflammatory bowel disease (IBD) outcomes among patients with both DM and IBD is not well understood. We conducted a systematic review and meta-analysis to evaluate IBD-related outcomes in patients with coexisting DM and IBD who were treated with GLP-1 RAs compared to those who were not.
Methods: We conducted a systematic search of PubMed, Embase, Scopus, and Google Scholar through April 2025 to identify studies reporting IBD-specific outcomes in patients with coexisting DM, stratified by GLP-1 RA use. Outcomes of interest included hospitalization related to IBD, initiation of oral corticosteroid therapy, and IBD-related surgery. A meta-analysis was conducted using a random-effects model, and heterogeneity among studies was assessed using the I² statistic.
Results: A total of four studies comprising 11,234 patients were included, with 3,905 patients in the GLP-1 RA group and 7,329 in the non-GLP-1 RA group. Patient ages ranged from 36 to 59 years. Among studies reporting sex distribution, 59.1% of participants were female. Among those reporting IBD subtype, 48.5% had ulcerative colitis (UC) and 51.5% had Crohn’s disease (CD).
GLP-1 RA use was associated with a significantly lower risk of IBD-related surgery (OR 0.62; 95% confidence interval [CI] 0.47–0.83; p = 0.001; I² = 0%), with this effect driven primarily by patients with CD (OR 0.60; 95% CI 0.43–0.84).
For oral corticosteroid use, no significant difference was observed between GLP-1 RA users and non-users (OR 1.10; 95% CI 0.92–1.31; p = 0.30; I² = 53%). Results remained similar with subgroup analyses for both UC (OR 0.99; 95% CI 0.61–1.61; p = 0.96) and CD (OR 1.18; 95% CI 1.01–1.37; p = 0.04).
Similarly, hospitalization rates did not differ significantly between groups (OR 0.79; 95% CI 0.56–1.11; p = 0.18; I² = 84%). Subgroup analysis revealed no significant differences for UC (OR 0.97; 95% CI 0.54–1.75; I² = 89%) or CD (OR 0.97; 95% CI 0.80–1.18; I² = 18%).
Discussion: Our findings suggest that in patients with IBD and DM, GLP-1 RA use is associated with a significant reduction in the need for CD-related surgery. However, no consistent benefits were observed in hospitalization rates or corticosteroid use. Further studies are needed to explore the direct immunomodulatory effects of GLP-1 RAs on intestinal inflammation.
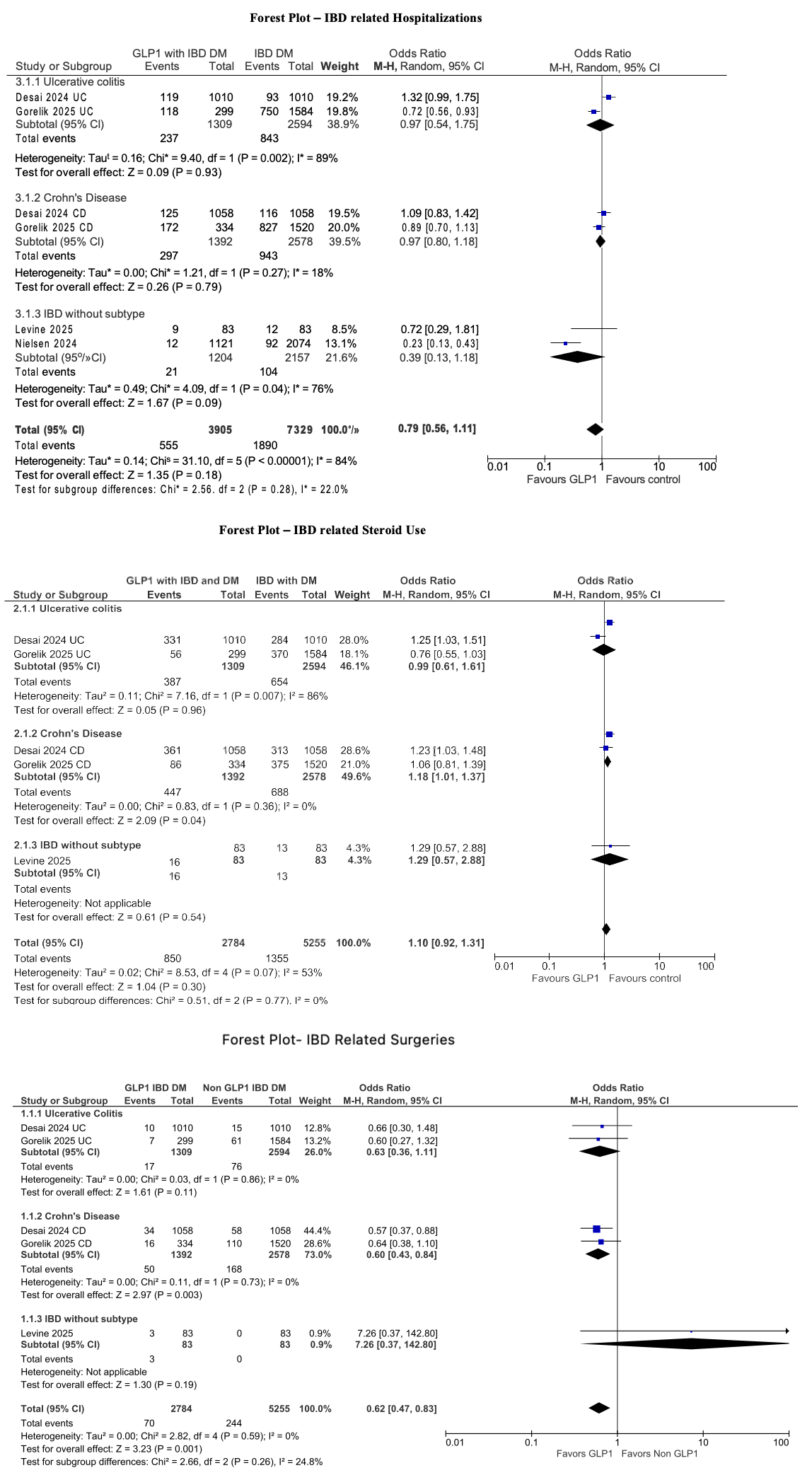
Figure: Figure1: Summary of Meta-Analysis Outcomes and Included Studies Evaluating GLP-1 Receptor Agonists (GLP-1 RAs) in Patients with Inflammatory Bowel Disease (IBD) and Diabetes Mellitus (DM)
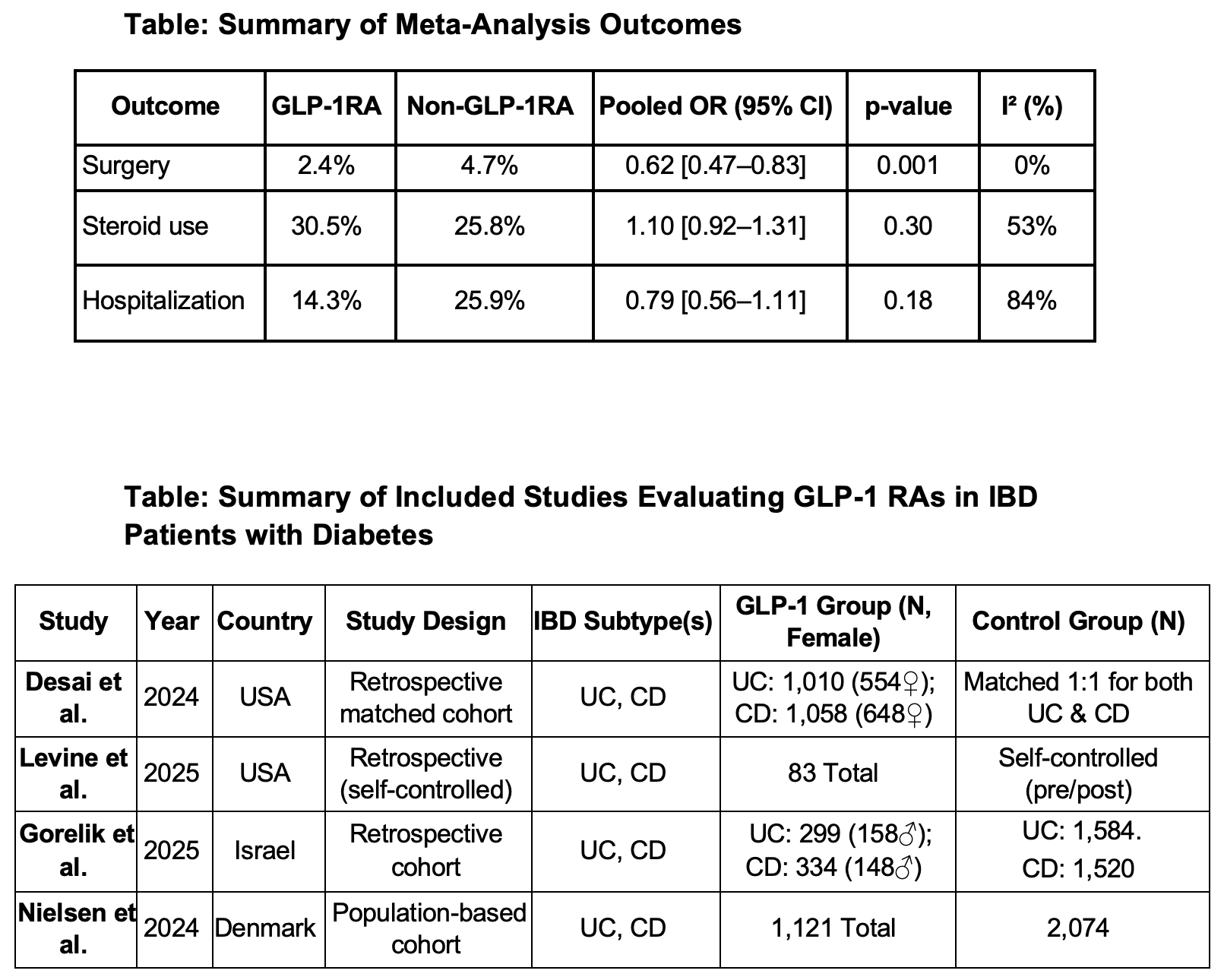
Figure: Figure2: Forest plots showing: (1) IBD-related hospitalizations, (2) IBD-related surgeries, and (3) IBD-related steroid use among GLP-1 RA users vs. non-users in patients with coexisting diabetes.
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Abdelkader Chaar indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Anjul Verma, MD2, Abdelkader Chaar, MD1, Babu P. Mohan, MD3, Idan Goren, MD1. P3314 - Impact of GLP-1 Receptor Agonists on IBD Outcomes in Patients With Diabetes Mellitus: A Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University, Syracuse, NY; 2Texas Tech University Health Sciences Center, Odessa, TX; 3Orlando Gastroenterology PA, Orlando, FL
Introduction: GLP-1 receptor agonists (GLP-1 RAs) are known for their metabolic benefits in managing diabetes mellitus (DM) and are thought to have anti-inflammatory effects. However, their impact on inflammatory bowel disease (IBD) outcomes among patients with both DM and IBD is not well understood. We conducted a systematic review and meta-analysis to evaluate IBD-related outcomes in patients with coexisting DM and IBD who were treated with GLP-1 RAs compared to those who were not.
Methods: We conducted a systematic search of PubMed, Embase, Scopus, and Google Scholar through April 2025 to identify studies reporting IBD-specific outcomes in patients with coexisting DM, stratified by GLP-1 RA use. Outcomes of interest included hospitalization related to IBD, initiation of oral corticosteroid therapy, and IBD-related surgery. A meta-analysis was conducted using a random-effects model, and heterogeneity among studies was assessed using the I² statistic.
Results: A total of four studies comprising 11,234 patients were included, with 3,905 patients in the GLP-1 RA group and 7,329 in the non-GLP-1 RA group. Patient ages ranged from 36 to 59 years. Among studies reporting sex distribution, 59.1% of participants were female. Among those reporting IBD subtype, 48.5% had ulcerative colitis (UC) and 51.5% had Crohn’s disease (CD).
GLP-1 RA use was associated with a significantly lower risk of IBD-related surgery (OR 0.62; 95% confidence interval [CI] 0.47–0.83; p = 0.001; I² = 0%), with this effect driven primarily by patients with CD (OR 0.60; 95% CI 0.43–0.84).
For oral corticosteroid use, no significant difference was observed between GLP-1 RA users and non-users (OR 1.10; 95% CI 0.92–1.31; p = 0.30; I² = 53%). Results remained similar with subgroup analyses for both UC (OR 0.99; 95% CI 0.61–1.61; p = 0.96) and CD (OR 1.18; 95% CI 1.01–1.37; p = 0.04).
Similarly, hospitalization rates did not differ significantly between groups (OR 0.79; 95% CI 0.56–1.11; p = 0.18; I² = 84%). Subgroup analysis revealed no significant differences for UC (OR 0.97; 95% CI 0.54–1.75; I² = 89%) or CD (OR 0.97; 95% CI 0.80–1.18; I² = 18%).
Discussion: Our findings suggest that in patients with IBD and DM, GLP-1 RA use is associated with a significant reduction in the need for CD-related surgery. However, no consistent benefits were observed in hospitalization rates or corticosteroid use. Further studies are needed to explore the direct immunomodulatory effects of GLP-1 RAs on intestinal inflammation.
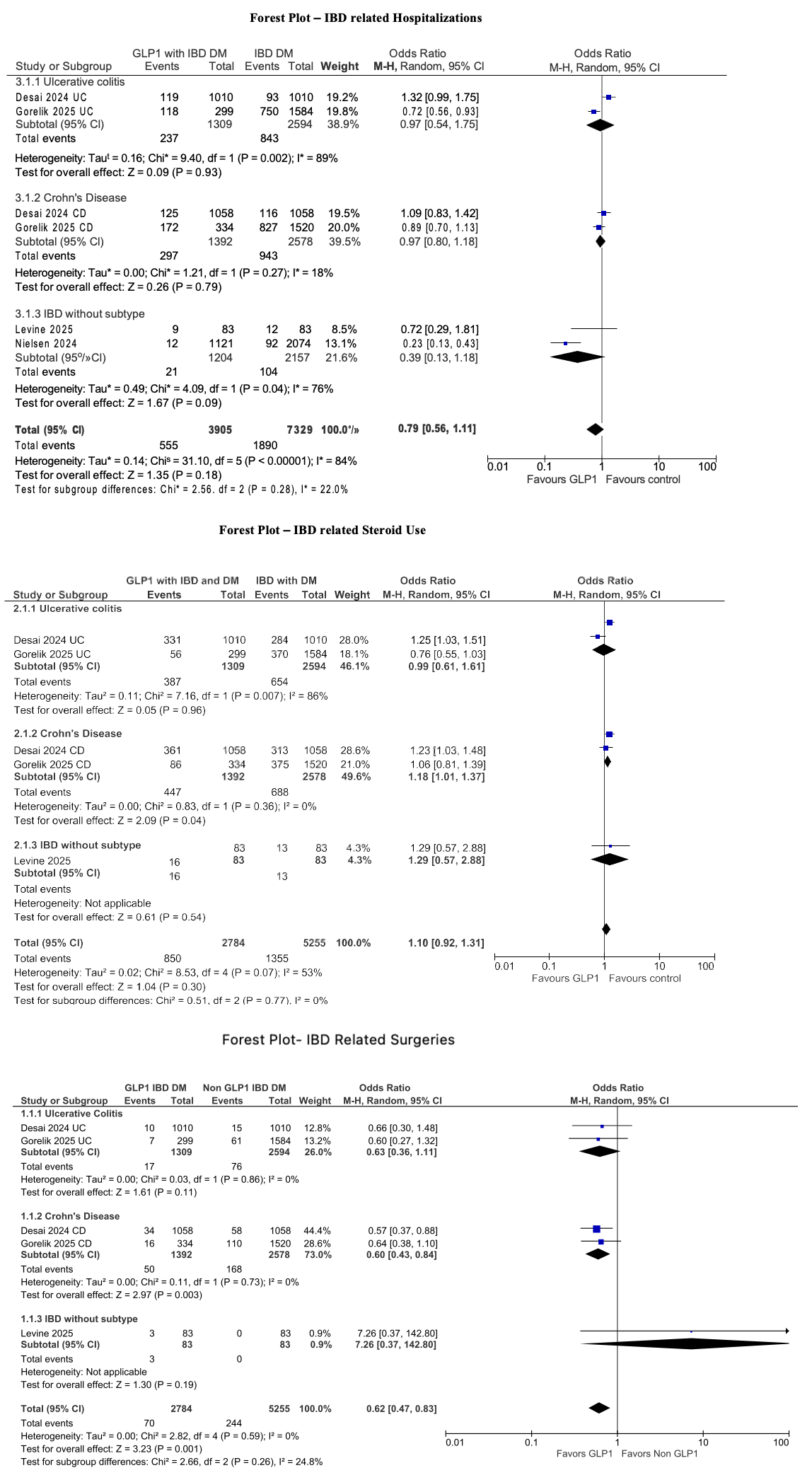
Figure: Figure1: Summary of Meta-Analysis Outcomes and Included Studies Evaluating GLP-1 Receptor Agonists (GLP-1 RAs) in Patients with Inflammatory Bowel Disease (IBD) and Diabetes Mellitus (DM)
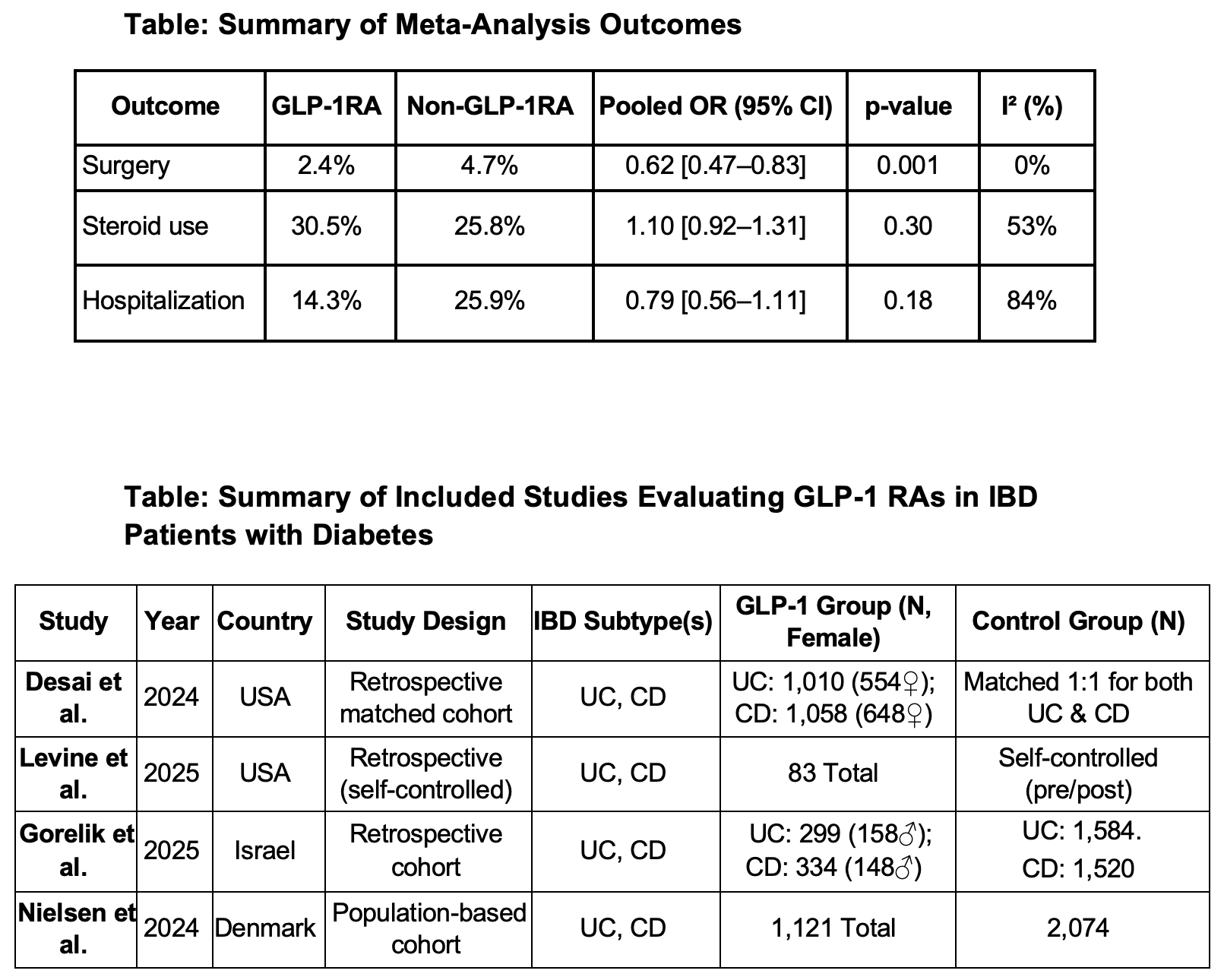
Figure: Figure2: Forest plots showing: (1) IBD-related hospitalizations, (2) IBD-related surgeries, and (3) IBD-related steroid use among GLP-1 RA users vs. non-users in patients with coexisting diabetes.
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Abdelkader Chaar indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Anjul Verma, MD2, Abdelkader Chaar, MD1, Babu P. Mohan, MD3, Idan Goren, MD1. P3314 - Impact of GLP-1 Receptor Agonists on IBD Outcomes in Patients With Diabetes Mellitus: A Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
