Monday Poster Session
Category: IBD
P3313 - Safety and Outcomes of Advanced IBD Therapies in People With HIV: A Propensity-Matched Cohort Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Avneet Kaur, MBBS (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Avneet Kaur, MBBS1, Avleen Kaur, MD2, Anjul Verma, MD3, Idan Goren, MD2
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3Texas Tech University Health Sciences Center, Odessa, TX
Introduction: Data on the safety of advanced therapy (AT) in people living with HIV and coexisting inflammatory bowel disease (IBD) remains limited. We aimed to evaluate IBD related outcomes in this population using a large real-world database.
Methods: We conducted a retrospective cohort study using the TriNetX database. Adults aged 14–80 years with both HIV and IBD were identified using ICD-10 codes from 2015–2020. Patients were stratified by receipt of AT. Propensity score matching (PSM) was applied to balance demographics, IBD subtype, comorbidities, and smoking history. Primary outcomes included serious infections, opportunistic infections, and cancer incidence; secondary outcomes included IBD related surgeries and all cause mortality.
Results: Among 674,115 IBD patients across 103 healthcare organizations, 2,290 had coexisting HIV and IBD and 156 (6.81%) received advanced therapy (AT). Mean follow up was 4.86 ± 1.64 years. The mean age was 44.9 ± 13.2 years. Males accounted for 79.50% of the cohort. Ulcerative colitis and Crohn’s disease were present in 65.02% and 39.78%, respectively. The most used advanced therapies were adalimumab (37.18%), infliximab (32.05%), and ustekinumab (20.51%).
Serious infections occurred in 74.36% of the AT group versus 72.11% in the non-AT group (OR 1.12, p=0.55). Opportunistic infections were comparable between groups (25.64% vs. 27.47%, OR 0.91, p=0.62). Syphilis was significantly less frequent in the AT group (10.26% vs. 17.25%, OR 0.55, p=0.02), while eye infections were significantly more common (7.69% vs. 3.70%, OR 2.17, p=0.01). Cancer incidence (6.41% vs. 1.55%) and IBD-related surgeries (6.41% vs. 1.36%) were more common in the AT group, but differences were not statistically significant. All-cause mortality was similar (6.41% vs. 7.73%).
In PSM analysis (135 matched pairs), infection, cancer, surgery, and mortality rates were similar between groups. Differences in syphilis and eye infections were no longer significant.
Discussion: In this large real-world cohort of HIV-IBD patients, advanced therapy was used in fewer than 7% of patients. This low utilization may reflect either a milder IBD course or underuse of AT due to perceived risks. AT was not associated with increased rates of serious or opportunistic infections, cumulative cancer incidence, IBD-related surgeries, or mortality. These findings suggest that advanced therapies can be safely used in the HIV-IBD population.
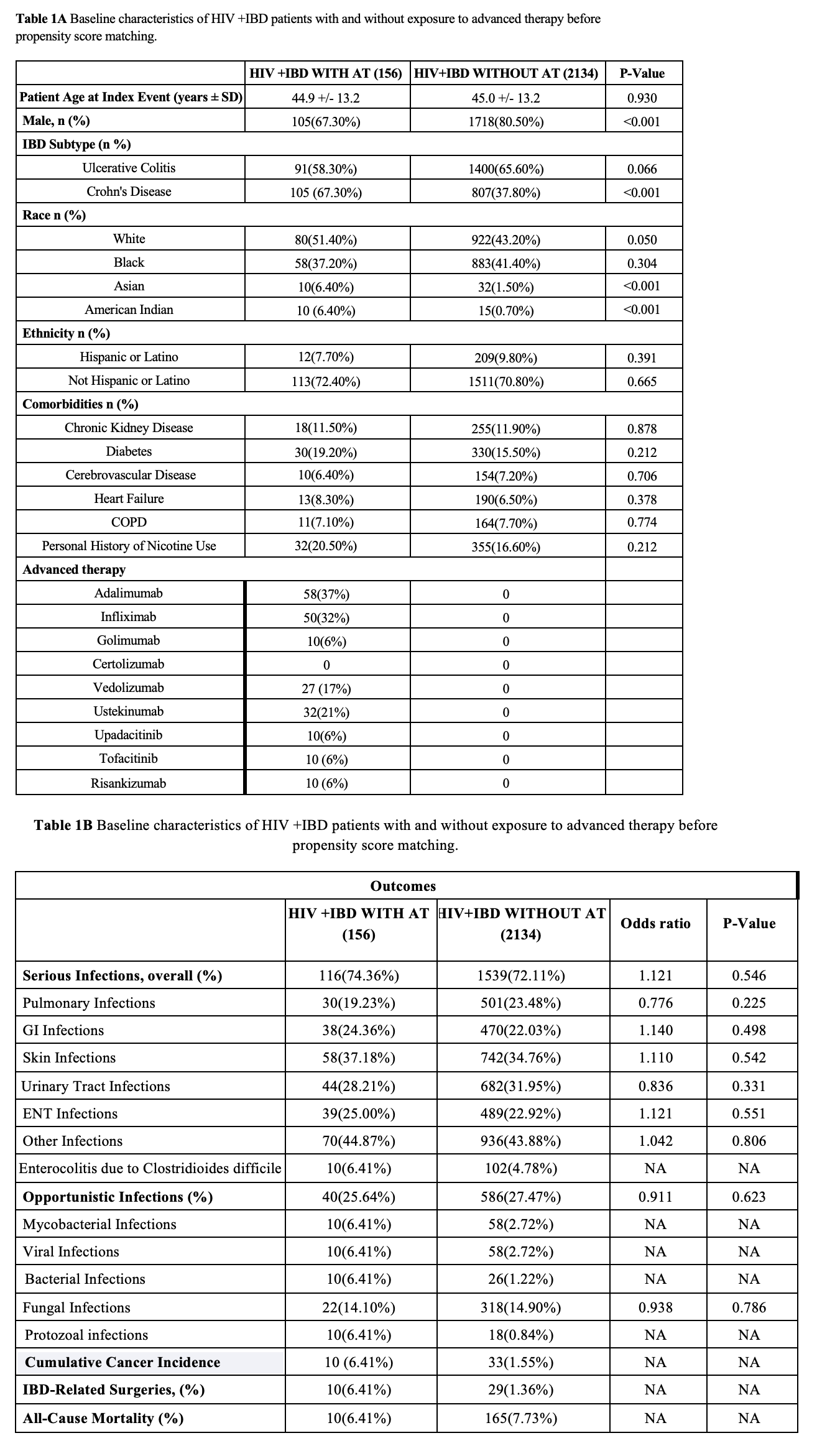
Figure: Figure1. Baseline characteristics and clinical outcomes of HIV+IBD patients with and without exposure to advanced therapy before propensity score matching.
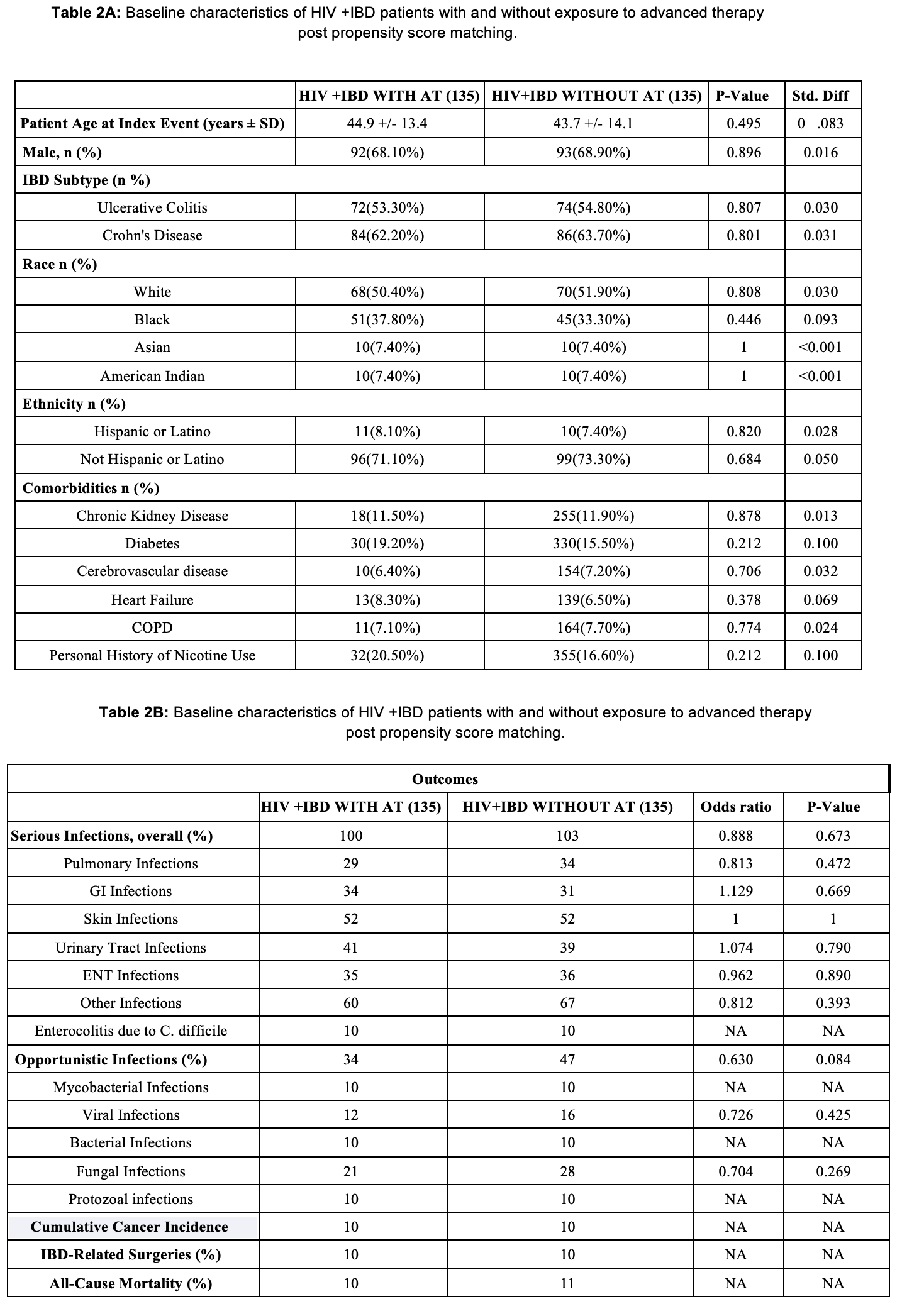
Figure: Figure2.Baseline characteristics and clinical outcomes of HIV+IBD patients with and without exposure to advanced therapy after propensity score matching.
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Avleen Kaur, MD2, Anjul Verma, MD3, Idan Goren, MD2. P3313 - Safety and Outcomes of Advanced IBD Therapies in People With HIV: A Propensity-Matched Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2SUNY Upstate Medical University, Syracuse, NY; 3Texas Tech University Health Sciences Center, Odessa, TX
Introduction: Data on the safety of advanced therapy (AT) in people living with HIV and coexisting inflammatory bowel disease (IBD) remains limited. We aimed to evaluate IBD related outcomes in this population using a large real-world database.
Methods: We conducted a retrospective cohort study using the TriNetX database. Adults aged 14–80 years with both HIV and IBD were identified using ICD-10 codes from 2015–2020. Patients were stratified by receipt of AT. Propensity score matching (PSM) was applied to balance demographics, IBD subtype, comorbidities, and smoking history. Primary outcomes included serious infections, opportunistic infections, and cancer incidence; secondary outcomes included IBD related surgeries and all cause mortality.
Results: Among 674,115 IBD patients across 103 healthcare organizations, 2,290 had coexisting HIV and IBD and 156 (6.81%) received advanced therapy (AT). Mean follow up was 4.86 ± 1.64 years. The mean age was 44.9 ± 13.2 years. Males accounted for 79.50% of the cohort. Ulcerative colitis and Crohn’s disease were present in 65.02% and 39.78%, respectively. The most used advanced therapies were adalimumab (37.18%), infliximab (32.05%), and ustekinumab (20.51%).
Serious infections occurred in 74.36% of the AT group versus 72.11% in the non-AT group (OR 1.12, p=0.55). Opportunistic infections were comparable between groups (25.64% vs. 27.47%, OR 0.91, p=0.62). Syphilis was significantly less frequent in the AT group (10.26% vs. 17.25%, OR 0.55, p=0.02), while eye infections were significantly more common (7.69% vs. 3.70%, OR 2.17, p=0.01). Cancer incidence (6.41% vs. 1.55%) and IBD-related surgeries (6.41% vs. 1.36%) were more common in the AT group, but differences were not statistically significant. All-cause mortality was similar (6.41% vs. 7.73%).
In PSM analysis (135 matched pairs), infection, cancer, surgery, and mortality rates were similar between groups. Differences in syphilis and eye infections were no longer significant.
Discussion: In this large real-world cohort of HIV-IBD patients, advanced therapy was used in fewer than 7% of patients. This low utilization may reflect either a milder IBD course or underuse of AT due to perceived risks. AT was not associated with increased rates of serious or opportunistic infections, cumulative cancer incidence, IBD-related surgeries, or mortality. These findings suggest that advanced therapies can be safely used in the HIV-IBD population.
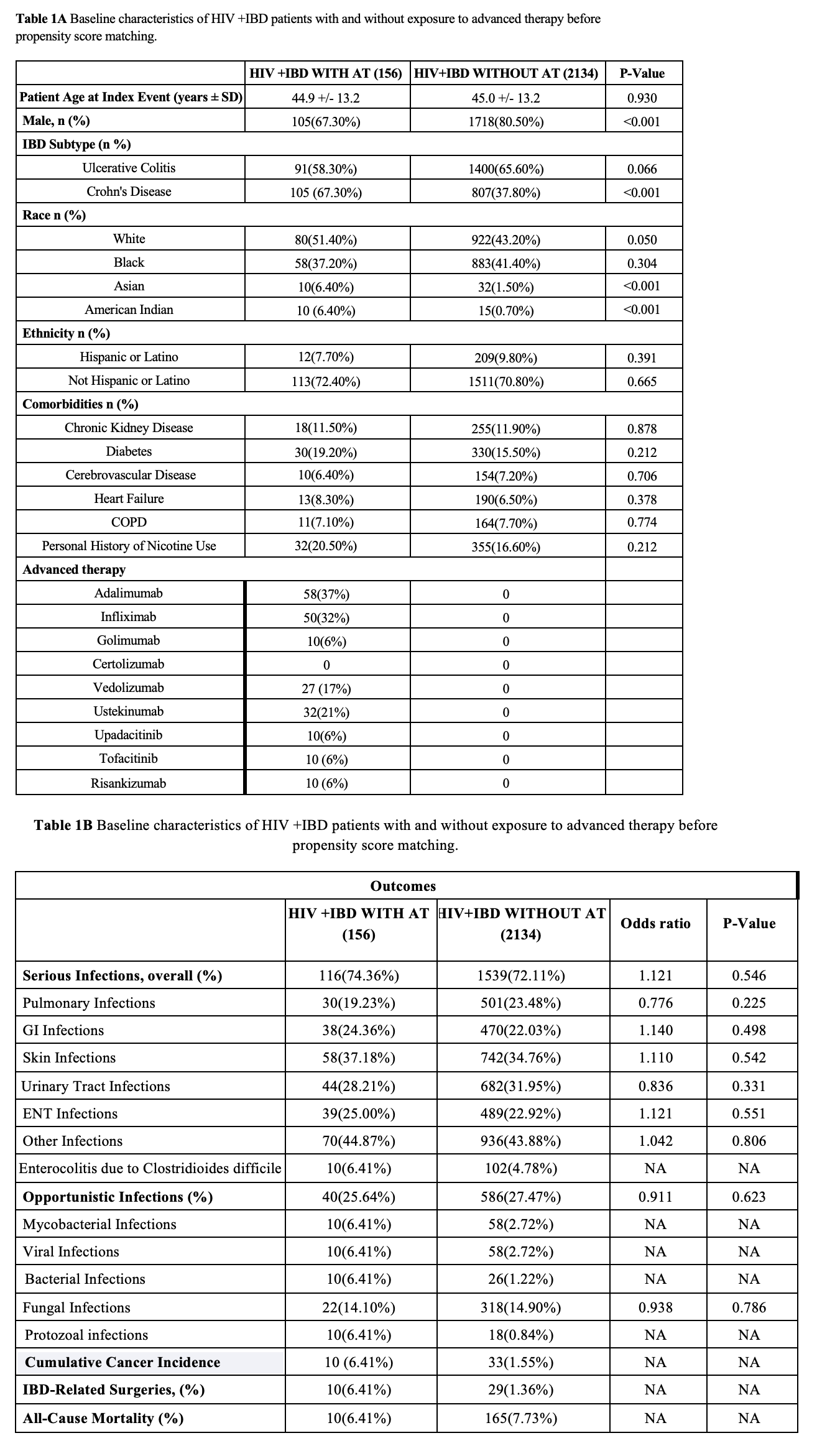
Figure: Figure1. Baseline characteristics and clinical outcomes of HIV+IBD patients with and without exposure to advanced therapy before propensity score matching.
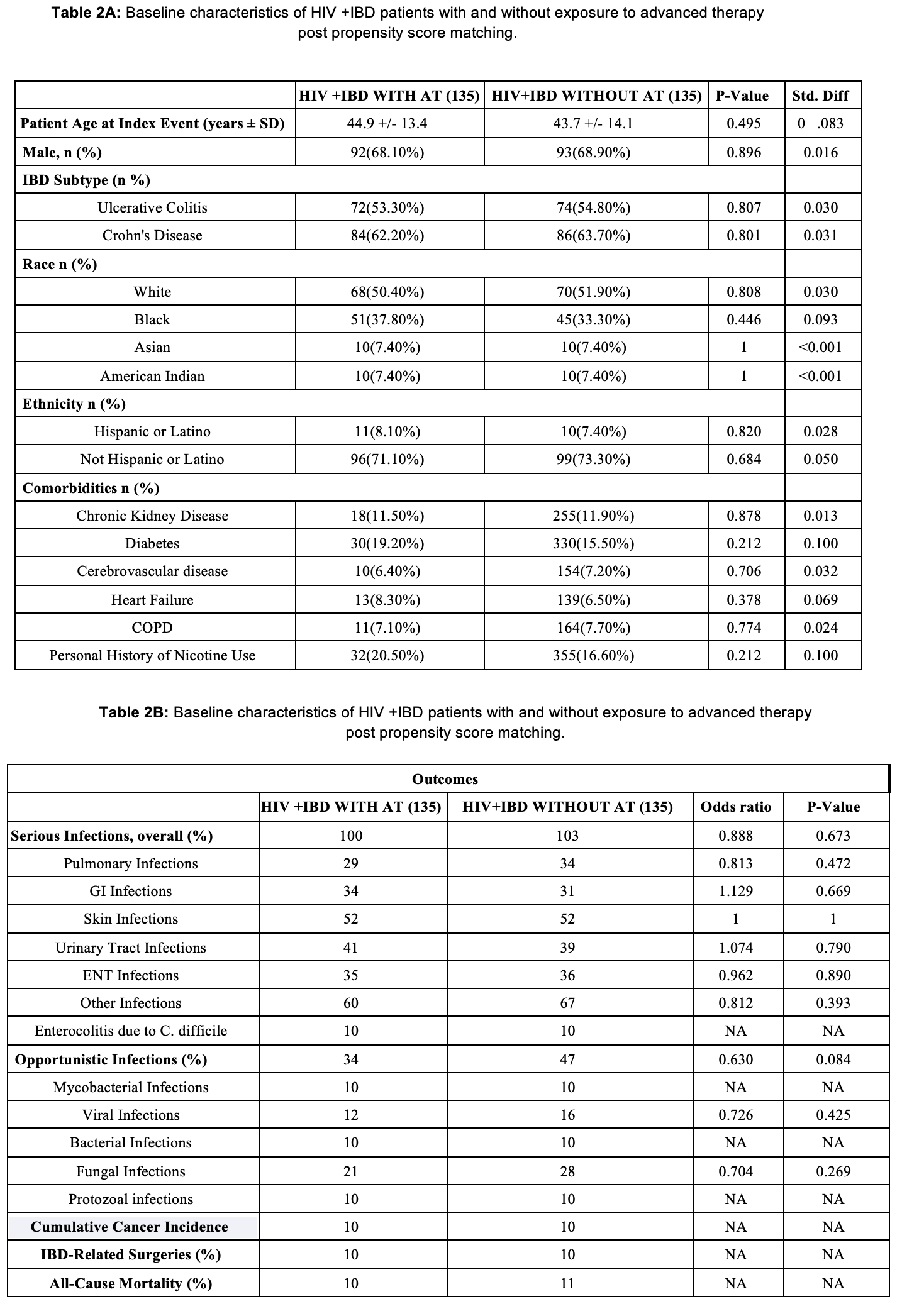
Figure: Figure2.Baseline characteristics and clinical outcomes of HIV+IBD patients with and without exposure to advanced therapy after propensity score matching.
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Idan Goren indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Avleen Kaur, MD2, Anjul Verma, MD3, Idan Goren, MD2. P3313 - Safety and Outcomes of Advanced IBD Therapies in People With HIV: A Propensity-Matched Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
