Monday Poster Session
Category: IBD
P3301 - Cardiovascular Outcomes of Biologics vs Non-Biologics Therapy in Inflammatory Bowel Disease: A Propensity-Matched Cohort Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Arman, MD, MPH
University at Buffalo
Depew, NY
Presenting Author(s)
Omar Arman, MD, MPH1, Khaled Rafeh, MD2, Kamal Hamad, MD3, Laith M.. Haj-Ahmad, MD4, Amer Arman, MD5, Mazen Zamzam, BS6, Osama Alshakhatreh, MD7, Jad Bou-Abdallah, MD1
1University at Buffalo, Buffalo, NY; 2School of Medicine, The University of Jordan, Shmeisani, 'Amman, Jordan; 3Jordan University of Science and Technology, Irbid, Irbid, Jordan; 4University of Jordan, Amman, 'Amman, Jordan; 5MedStar Health, Washington, WA; 6Oakland University William Beaumont School of Medicine, Royal Oak, MI; 7Albany Medical Center, Albany, NY
Introduction: Inflammatory bowel disease (IBD) increases the risk of cardiovascular (CV) complications, including myocardial infarction (MI), stroke, heart failure, and arrhythmia, especially during flares. Effective treatment may reduce CV risk, but data comparing biologic vs. non-biologic therapies are limited. This study evaluates the impact of therapy type on CV risk in IBD over 1, 3, and 5 years.
Methods: Using the TriNetX Research Network, we analyzed 225,303 IBD patients from 94 healthcare organizations. Adults (≥18 years) with Crohn’s disease or ulcerative colitis and no prior MI, stroke, heart failure, or significant arrhythmia were included. Patients were stratified into biologic and non-biologic cohorts and propensity score-matched for demographics, comorbidities, and disease severity, yielding balanced groups at 1 year (N=16,179), 3 years (N=16,181), and 5 years (N=15,821). Primary outcomes included incidence of stroke, MI, heart failure, and arrhythmias. Kaplan-Meier analysis estimated event-free survival, and hazard ratios with 95% confidence intervals were calculated.
Results: At 5 years, biologics reduced MI risk by 0.18% (p < 0.0001), stroke by 0.12% (p = 0.002), heart failure by 0.22% (p < 0.0001), and arrhythmia by 0.91% (p < 0.0001), with significantly higher event-free survival probabilities (Table 1). Figure 1 presents a bar chart of risk differences and a forest plot of hazard ratios.
Discussion: Biologic therapy is associated with significant reductions in cardiovascular events, including myocardial infarction, stroke, heart failure, and arrhythmias, over 5 years in IBD patients. These findings highlight the potential cardioprotective effects of biologics, likely through the reduction of systemic inflammation which is a known contributor to cardiovascular risk. While these results emphasize the importance of incorporating biologics into IBD management, prospective studies are needed to confirm causality and explore the underlying mechanisms driving these benefits.
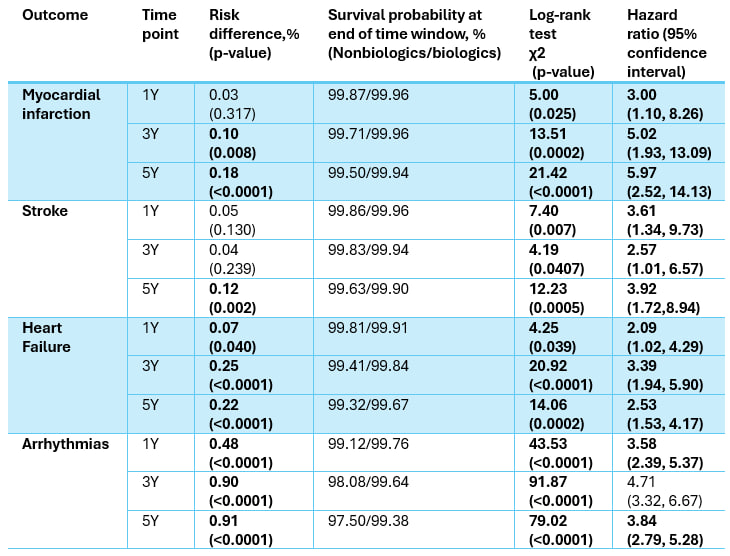
Figure: Key statistics for major cardiovascular outcomes in patients taking biologic vs. non-biologic therapy.
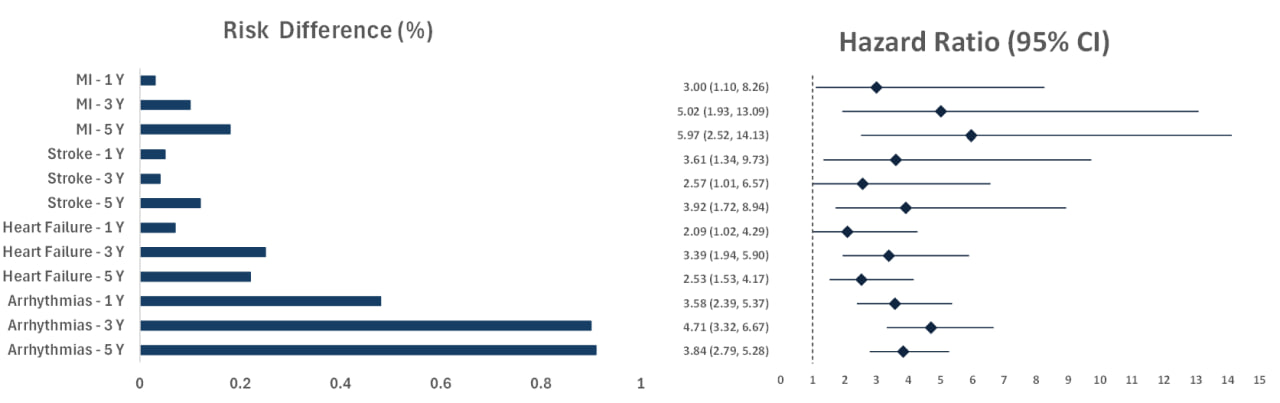
Figure: Figure 1. Risk Differences and Hazard Ratios for Cardiovascular Outcomes Over Five Years in Biologic vs. Non-Biologic Therapy.
MI: Myocardial Infarction, CI: Confidence Interval
Disclosures:
Omar Arman indicated no relevant financial relationships.
Khaled Rafeh indicated no relevant financial relationships.
Kamal Hamad indicated no relevant financial relationships.
Laith Haj-Ahmad indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Mazen Zamzam indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Jad Bou-Abdallah indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Khaled Rafeh, MD2, Kamal Hamad, MD3, Laith M.. Haj-Ahmad, MD4, Amer Arman, MD5, Mazen Zamzam, BS6, Osama Alshakhatreh, MD7, Jad Bou-Abdallah, MD1. P3301 - Cardiovascular Outcomes of Biologics vs Non-Biologics Therapy in Inflammatory Bowel Disease: A Propensity-Matched Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2School of Medicine, The University of Jordan, Shmeisani, 'Amman, Jordan; 3Jordan University of Science and Technology, Irbid, Irbid, Jordan; 4University of Jordan, Amman, 'Amman, Jordan; 5MedStar Health, Washington, WA; 6Oakland University William Beaumont School of Medicine, Royal Oak, MI; 7Albany Medical Center, Albany, NY
Introduction: Inflammatory bowel disease (IBD) increases the risk of cardiovascular (CV) complications, including myocardial infarction (MI), stroke, heart failure, and arrhythmia, especially during flares. Effective treatment may reduce CV risk, but data comparing biologic vs. non-biologic therapies are limited. This study evaluates the impact of therapy type on CV risk in IBD over 1, 3, and 5 years.
Methods: Using the TriNetX Research Network, we analyzed 225,303 IBD patients from 94 healthcare organizations. Adults (≥18 years) with Crohn’s disease or ulcerative colitis and no prior MI, stroke, heart failure, or significant arrhythmia were included. Patients were stratified into biologic and non-biologic cohorts and propensity score-matched for demographics, comorbidities, and disease severity, yielding balanced groups at 1 year (N=16,179), 3 years (N=16,181), and 5 years (N=15,821). Primary outcomes included incidence of stroke, MI, heart failure, and arrhythmias. Kaplan-Meier analysis estimated event-free survival, and hazard ratios with 95% confidence intervals were calculated.
Results: At 5 years, biologics reduced MI risk by 0.18% (p < 0.0001), stroke by 0.12% (p = 0.002), heart failure by 0.22% (p < 0.0001), and arrhythmia by 0.91% (p < 0.0001), with significantly higher event-free survival probabilities (Table 1). Figure 1 presents a bar chart of risk differences and a forest plot of hazard ratios.
Discussion: Biologic therapy is associated with significant reductions in cardiovascular events, including myocardial infarction, stroke, heart failure, and arrhythmias, over 5 years in IBD patients. These findings highlight the potential cardioprotective effects of biologics, likely through the reduction of systemic inflammation which is a known contributor to cardiovascular risk. While these results emphasize the importance of incorporating biologics into IBD management, prospective studies are needed to confirm causality and explore the underlying mechanisms driving these benefits.
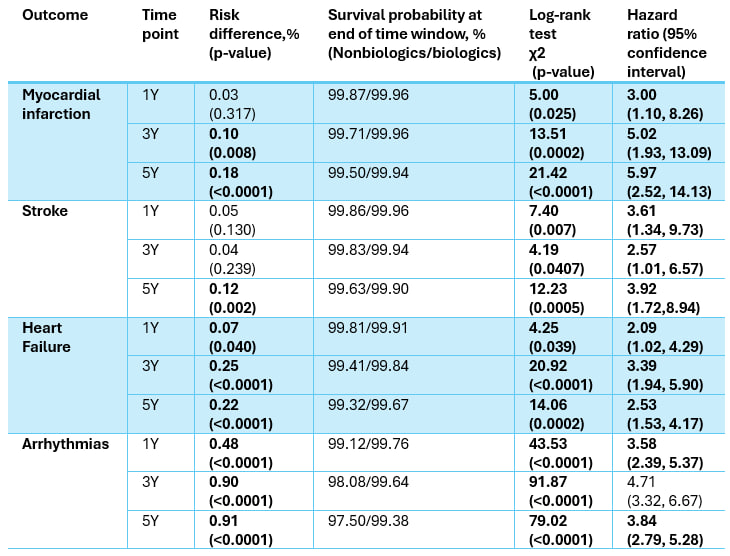
Figure: Key statistics for major cardiovascular outcomes in patients taking biologic vs. non-biologic therapy.
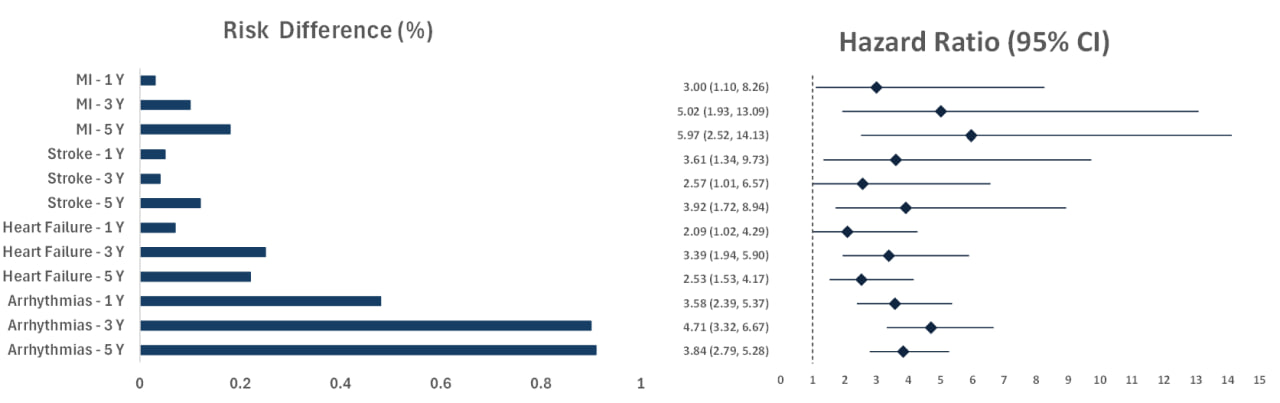
Figure: Figure 1. Risk Differences and Hazard Ratios for Cardiovascular Outcomes Over Five Years in Biologic vs. Non-Biologic Therapy.
MI: Myocardial Infarction, CI: Confidence Interval
Disclosures:
Omar Arman indicated no relevant financial relationships.
Khaled Rafeh indicated no relevant financial relationships.
Kamal Hamad indicated no relevant financial relationships.
Laith Haj-Ahmad indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Mazen Zamzam indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Jad Bou-Abdallah indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Khaled Rafeh, MD2, Kamal Hamad, MD3, Laith M.. Haj-Ahmad, MD4, Amer Arman, MD5, Mazen Zamzam, BS6, Osama Alshakhatreh, MD7, Jad Bou-Abdallah, MD1. P3301 - Cardiovascular Outcomes of Biologics vs Non-Biologics Therapy in Inflammatory Bowel Disease: A Propensity-Matched Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
