Monday Poster Session
Category: IBD
P3300 - Biologic Therapy vs Non-Biologics in Reducing Myocardial Infarction Risk in Inflammatory Bowel Disease: A 5-Year Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Arman, MD, MPH
University at Buffalo
Depew, NY
Presenting Author(s)
Omar Arman, MD, MPH1, Khaled Rafeh, MD2, Laith M.. Haj-Ahmad, MD3, Amer Arman, MD4, Kamal Hamad, MD5, Mazen Zamzam, BS6, Osama Alshakhatreh, MD7, Jad Bou-Abdallah, MD1
1University at Buffalo, Buffalo, NY; 2School of Medicine, The University of Jordan, Shmeisani, 'Amman, Jordan; 3University of Jordan, Amman, 'Amman, Jordan; 4MedStar Health, Washington, WA; 5Jordan University of Science and Technology, Irbid, Irbid, Jordan; 6Oakland University William Beaumont School of Medicine, Royal Oak, MI; 7Albany Medical Center, Albany, NY
Introduction: Patients with inflammatory bowel disease (IBD) face an elevated risk of myocardial infarction (MI) due to chronic systemic inflammation, increased pro-inflammatory cytokines, and accelerated atherosclerosis. This risk is further heightened during disease flares. Biologic therapy, which effectively controls inflammation, may reduce MI risk, yet limited data exist comparing its impact to non-biologic therapies. This study aims to assess whether biologic therapy is associated with a lower risk of MI compared to non-biologic therapy at 1-, 3-, and 5-year time points.
Methods: We obtained electronic medical records for 225,303 adult IBD patients from 94 healthcare organizations through the TriNetX Research Network. We excluded patients with prior MI, stroke, heart failure, or arrhythmia. We divided the patients into biologic and non-biologic therapy cohorts and performed propensity score matching (PSM) to balance demographics, comorbidities, and disease severity. This resulted in balanced groups at 1 year (N=16,179), 3 years (N=16,181), and 5 years (N=15,821). MI incidence was the primary outcome. Comparative analyses included MI risk ratios (RRs), hazard ratios (HRs), and Kaplan-Meier survival probabilities.
Results: Biologic therapy significantly reduced MI risk at 3 and 5 years, with absolute risk differences of 0.10% (p=0.008) at 3 years and 0.18% (p< 0.001) at 5 years. The 1-year difference (0.03%, p=0.317) was not significant. Kaplan-Meier analysis demonstrated higher MI-free survival in the biologic group at all time points. Corresponding HRs (95% CI) were 3.00 (1.10-8.26) at 1 year, 5.02 (1.93-13.09) at 3 years, and 5.97 (2.52-14.13) at 5 years. These findings suggest a growing survival benefit with biologic therapy over time. Statistics are available in Table 1, with risk differences visualized in Figure 1.
Discussion: Biologic therapy significantly reduces the long-term risk of myocardial infarction in IBD patients, with substantial benefits at 3 and 5 years. These effects may stem from biologics’ ability to suppress systemic inflammation, a key driver of cardiovascular events. While propensity score matching minimizes confounding, the retrospective design limits causality. Prospective studies are needed to confirm these findings and explain biologic therapy’s cardioprotective effects.
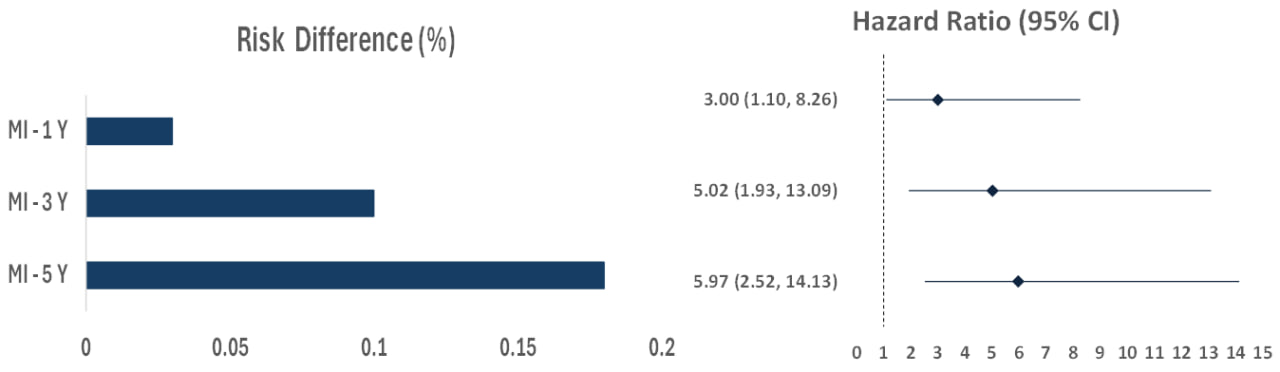
Figure: Figure 1. Comparison of Risk Differences and Hazard Ratios for MI in Biologic vs. Non-Biologic Therapy at 1, 3, and 5 Years.
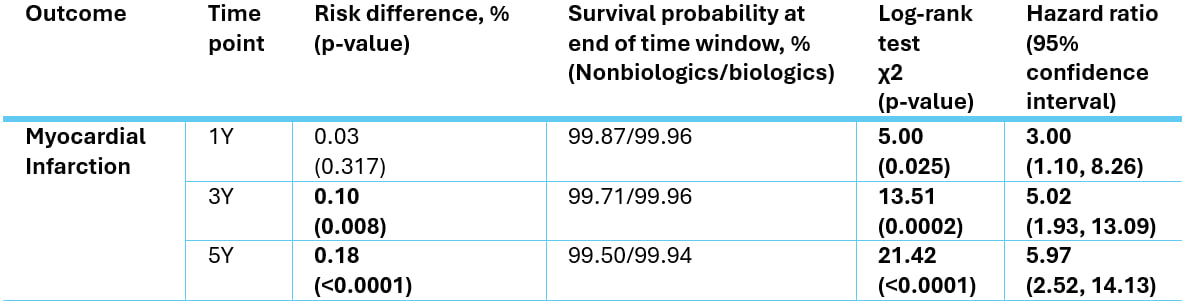
Figure: Table 1. Key statistics for MI outcomes in patients taking biologic vs. non-biologic therapy.
Disclosures:
Omar Arman indicated no relevant financial relationships.
Khaled Rafeh indicated no relevant financial relationships.
Laith Haj-Ahmad indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Kamal Hamad indicated no relevant financial relationships.
Mazen Zamzam indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Jad Bou-Abdallah indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Khaled Rafeh, MD2, Laith M.. Haj-Ahmad, MD3, Amer Arman, MD4, Kamal Hamad, MD5, Mazen Zamzam, BS6, Osama Alshakhatreh, MD7, Jad Bou-Abdallah, MD1. P3300 - Biologic Therapy vs Non-Biologics in Reducing Myocardial Infarction Risk in Inflammatory Bowel Disease: A 5-Year Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2School of Medicine, The University of Jordan, Shmeisani, 'Amman, Jordan; 3University of Jordan, Amman, 'Amman, Jordan; 4MedStar Health, Washington, WA; 5Jordan University of Science and Technology, Irbid, Irbid, Jordan; 6Oakland University William Beaumont School of Medicine, Royal Oak, MI; 7Albany Medical Center, Albany, NY
Introduction: Patients with inflammatory bowel disease (IBD) face an elevated risk of myocardial infarction (MI) due to chronic systemic inflammation, increased pro-inflammatory cytokines, and accelerated atherosclerosis. This risk is further heightened during disease flares. Biologic therapy, which effectively controls inflammation, may reduce MI risk, yet limited data exist comparing its impact to non-biologic therapies. This study aims to assess whether biologic therapy is associated with a lower risk of MI compared to non-biologic therapy at 1-, 3-, and 5-year time points.
Methods: We obtained electronic medical records for 225,303 adult IBD patients from 94 healthcare organizations through the TriNetX Research Network. We excluded patients with prior MI, stroke, heart failure, or arrhythmia. We divided the patients into biologic and non-biologic therapy cohorts and performed propensity score matching (PSM) to balance demographics, comorbidities, and disease severity. This resulted in balanced groups at 1 year (N=16,179), 3 years (N=16,181), and 5 years (N=15,821). MI incidence was the primary outcome. Comparative analyses included MI risk ratios (RRs), hazard ratios (HRs), and Kaplan-Meier survival probabilities.
Results: Biologic therapy significantly reduced MI risk at 3 and 5 years, with absolute risk differences of 0.10% (p=0.008) at 3 years and 0.18% (p< 0.001) at 5 years. The 1-year difference (0.03%, p=0.317) was not significant. Kaplan-Meier analysis demonstrated higher MI-free survival in the biologic group at all time points. Corresponding HRs (95% CI) were 3.00 (1.10-8.26) at 1 year, 5.02 (1.93-13.09) at 3 years, and 5.97 (2.52-14.13) at 5 years. These findings suggest a growing survival benefit with biologic therapy over time. Statistics are available in Table 1, with risk differences visualized in Figure 1.
Discussion: Biologic therapy significantly reduces the long-term risk of myocardial infarction in IBD patients, with substantial benefits at 3 and 5 years. These effects may stem from biologics’ ability to suppress systemic inflammation, a key driver of cardiovascular events. While propensity score matching minimizes confounding, the retrospective design limits causality. Prospective studies are needed to confirm these findings and explain biologic therapy’s cardioprotective effects.
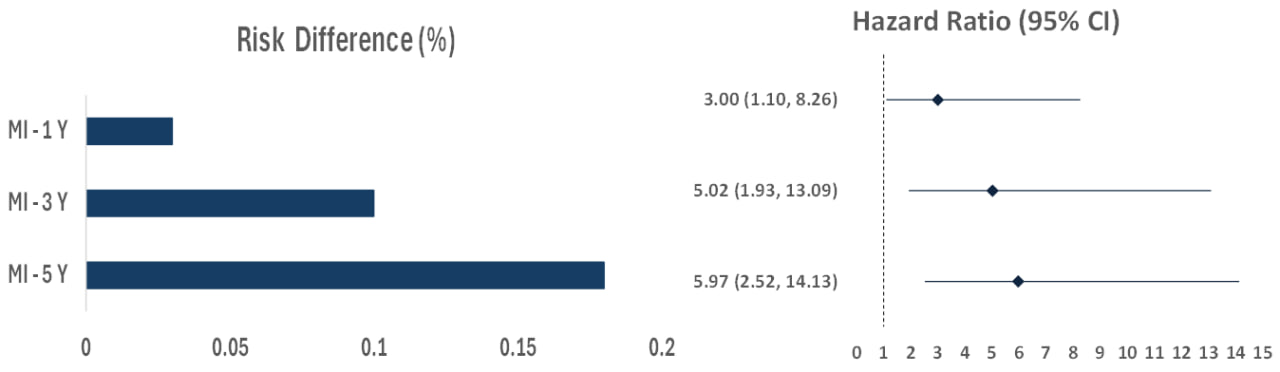
Figure: Figure 1. Comparison of Risk Differences and Hazard Ratios for MI in Biologic vs. Non-Biologic Therapy at 1, 3, and 5 Years.
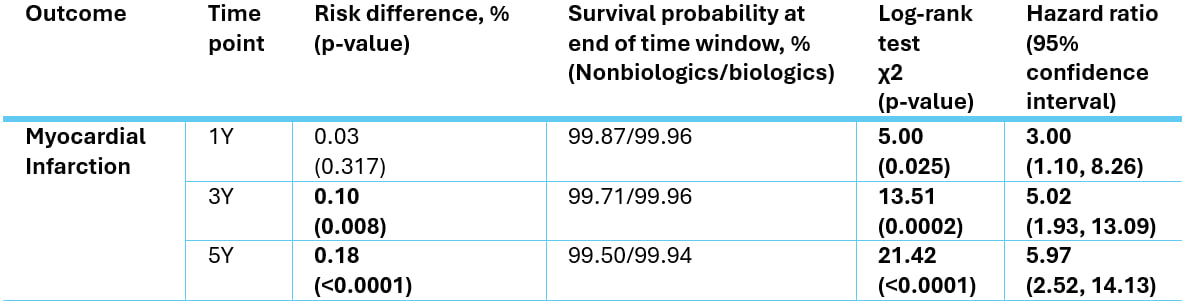
Figure: Table 1. Key statistics for MI outcomes in patients taking biologic vs. non-biologic therapy.
Disclosures:
Omar Arman indicated no relevant financial relationships.
Khaled Rafeh indicated no relevant financial relationships.
Laith Haj-Ahmad indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Kamal Hamad indicated no relevant financial relationships.
Mazen Zamzam indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Jad Bou-Abdallah indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Khaled Rafeh, MD2, Laith M.. Haj-Ahmad, MD3, Amer Arman, MD4, Kamal Hamad, MD5, Mazen Zamzam, BS6, Osama Alshakhatreh, MD7, Jad Bou-Abdallah, MD1. P3300 - Biologic Therapy vs Non-Biologics in Reducing Myocardial Infarction Risk in Inflammatory Bowel Disease: A 5-Year Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
