Monday Poster Session
Category: IBD
P3271 - Discharge Disposition of Older Adults Admitted With Inflammatory Bowel Diseases: A Nationwide Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chisom Nwaneki, MD, MPH
Saint Peter's University Hospital, New Brunswick, NJ
New Brunswick, NJ
Presenting Author(s)
Chisom Nwaneki, MD, MPH1, Adam Faye, MD, MS2
1Saint Peter's University Hospital, New Brunswick, NJ, New Brunswick, NJ; 2NYU Langone Health, New York, NY
Introduction: The burden of inflammatory bowel disease (IBD) among older adults has risen significantly over the past three decades, presenting unique clinical challenges and placing increased strain on healthcare resources. However, data remain limited on in-hospital outcomes and discharge disposition among older adults hospitalized with IBD in the United States.
Methods: We conducted a retrospective cross-sectional study using the National Inpatient Sample (NIS) from 2016 to 2020. Adult patients (≥18 years) hospitalized with a primary diagnosis of IBD, either ulcerative colitis (UC) or Crohn’s disease (CD), were included. The primary outcome was discharge disposition. Multivariable logistic regression was used to assess the association between age group and discharge disposition, adjusting for potential confounders, with additional analysis comparing older adults with diverticulitis to older adults with IBD performed.
Results: We identified 55,025 patients with a primary diagnosis of IBD (70% CD, 30% UC). Of these, 23.9% of all IBD patients, 20.3% of CD patients, and 32.2% of UC patients were aged 60 years or older. Among all IBD patients, 0.1% of younger adults vs 1.0% of older adults died, 88.5% of younger adults were discharged home vs 71.7% of older adults, 8.6% of younger adults were discharged with aide vs 14.9% of older adults, and 2.8% of younger adults were discharged to a facility vs 12.4% of older adults (all p values < 0.001). On multivariable analysis, older adults had 40% higher odds of being discharged home with aide (OR 1.40, CI 1.30-1.53), 129% higher odds of discharge to a facility (OR 2.29, CI 2.05-2.56), and nearly 5 times higher odds of in-hospital mortality (OR 4.94, 95%CI 2.99-8.15) compared to younger adults. When compared to older adults with diverticulitis, those with IBD had 35% higher odds of being discharged to a facility (OR 1.35, CI 1.27-1.43) and 110% higher odds of mortality (OR 2.10, CI 1.76 -2.54).
Discussion: Older adults hospitalized with IBD are more likely to require home health services or facility care upon discharge and are at significantly increased risk of in-hospital mortality compared to younger adults with IBD. Additionally, older adults with IBD are more likely to die or require discharge to a facility as compared to older adults hospitalized for diverticulitis. These findings underscore the need for tailored inpatient care strategies and proactive discharge planning in this vulnerable patient population.
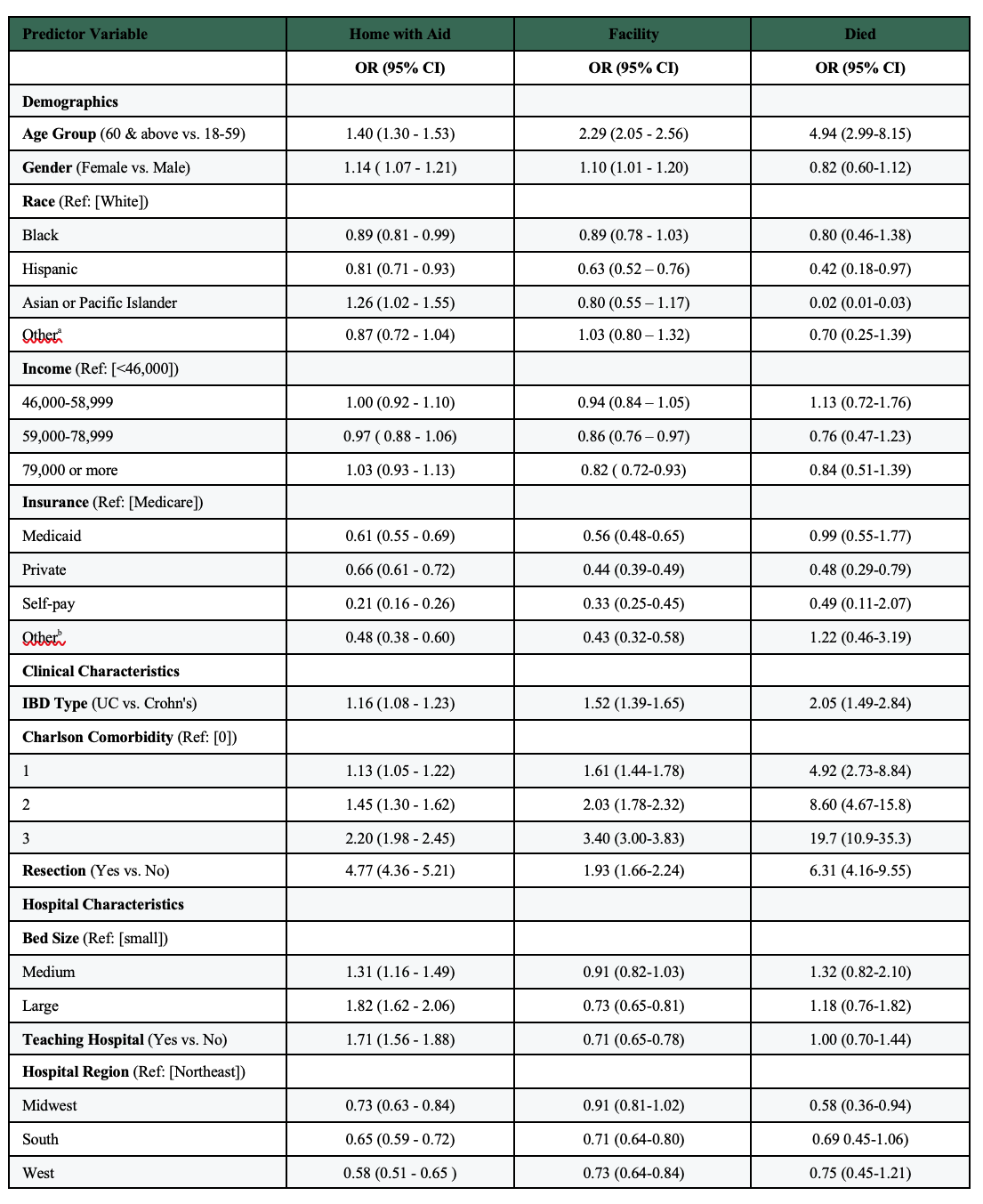
Figure: Fig 1. Discharge Disposition of the General IBD population 2016-2020
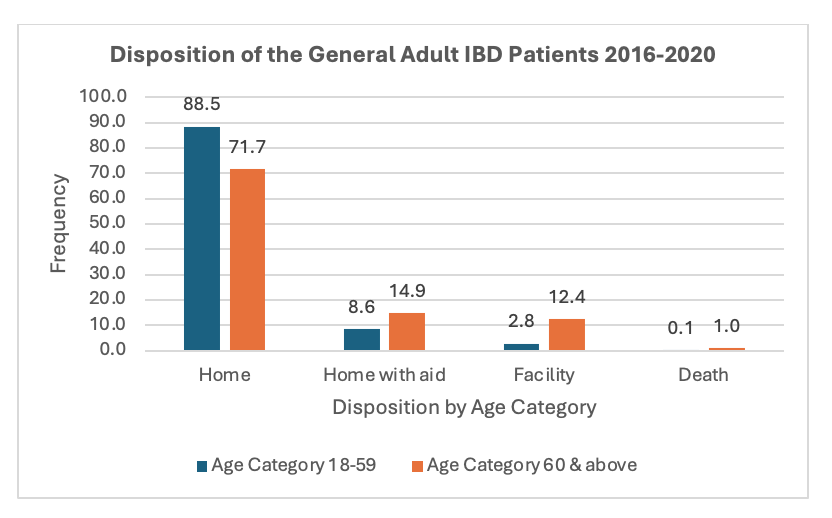
Figure: Table 1. Multivariate Regression Analysis on Discharge Disposition in the General IBD Population.
Disclosures:
Chisom Nwaneki indicated no relevant financial relationships.
Adam Faye: AbbVie – Honorarium. Eli Lilly – Consultant. NIH Grant K76AG083286 – Grant/Research Support. Takeda – Honorarium. The American College of Gastroenterology – Grant/Research Support. The Crohn's and Colitis Foundation – Grant/Research Support.
Chisom Nwaneki, MD, MPH1, Adam Faye, MD, MS2. P3271 - Discharge Disposition of Older Adults Admitted With Inflammatory Bowel Diseases: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Peter's University Hospital, New Brunswick, NJ, New Brunswick, NJ; 2NYU Langone Health, New York, NY
Introduction: The burden of inflammatory bowel disease (IBD) among older adults has risen significantly over the past three decades, presenting unique clinical challenges and placing increased strain on healthcare resources. However, data remain limited on in-hospital outcomes and discharge disposition among older adults hospitalized with IBD in the United States.
Methods: We conducted a retrospective cross-sectional study using the National Inpatient Sample (NIS) from 2016 to 2020. Adult patients (≥18 years) hospitalized with a primary diagnosis of IBD, either ulcerative colitis (UC) or Crohn’s disease (CD), were included. The primary outcome was discharge disposition. Multivariable logistic regression was used to assess the association between age group and discharge disposition, adjusting for potential confounders, with additional analysis comparing older adults with diverticulitis to older adults with IBD performed.
Results: We identified 55,025 patients with a primary diagnosis of IBD (70% CD, 30% UC). Of these, 23.9% of all IBD patients, 20.3% of CD patients, and 32.2% of UC patients were aged 60 years or older. Among all IBD patients, 0.1% of younger adults vs 1.0% of older adults died, 88.5% of younger adults were discharged home vs 71.7% of older adults, 8.6% of younger adults were discharged with aide vs 14.9% of older adults, and 2.8% of younger adults were discharged to a facility vs 12.4% of older adults (all p values < 0.001). On multivariable analysis, older adults had 40% higher odds of being discharged home with aide (OR 1.40, CI 1.30-1.53), 129% higher odds of discharge to a facility (OR 2.29, CI 2.05-2.56), and nearly 5 times higher odds of in-hospital mortality (OR 4.94, 95%CI 2.99-8.15) compared to younger adults. When compared to older adults with diverticulitis, those with IBD had 35% higher odds of being discharged to a facility (OR 1.35, CI 1.27-1.43) and 110% higher odds of mortality (OR 2.10, CI 1.76 -2.54).
Discussion: Older adults hospitalized with IBD are more likely to require home health services or facility care upon discharge and are at significantly increased risk of in-hospital mortality compared to younger adults with IBD. Additionally, older adults with IBD are more likely to die or require discharge to a facility as compared to older adults hospitalized for diverticulitis. These findings underscore the need for tailored inpatient care strategies and proactive discharge planning in this vulnerable patient population.
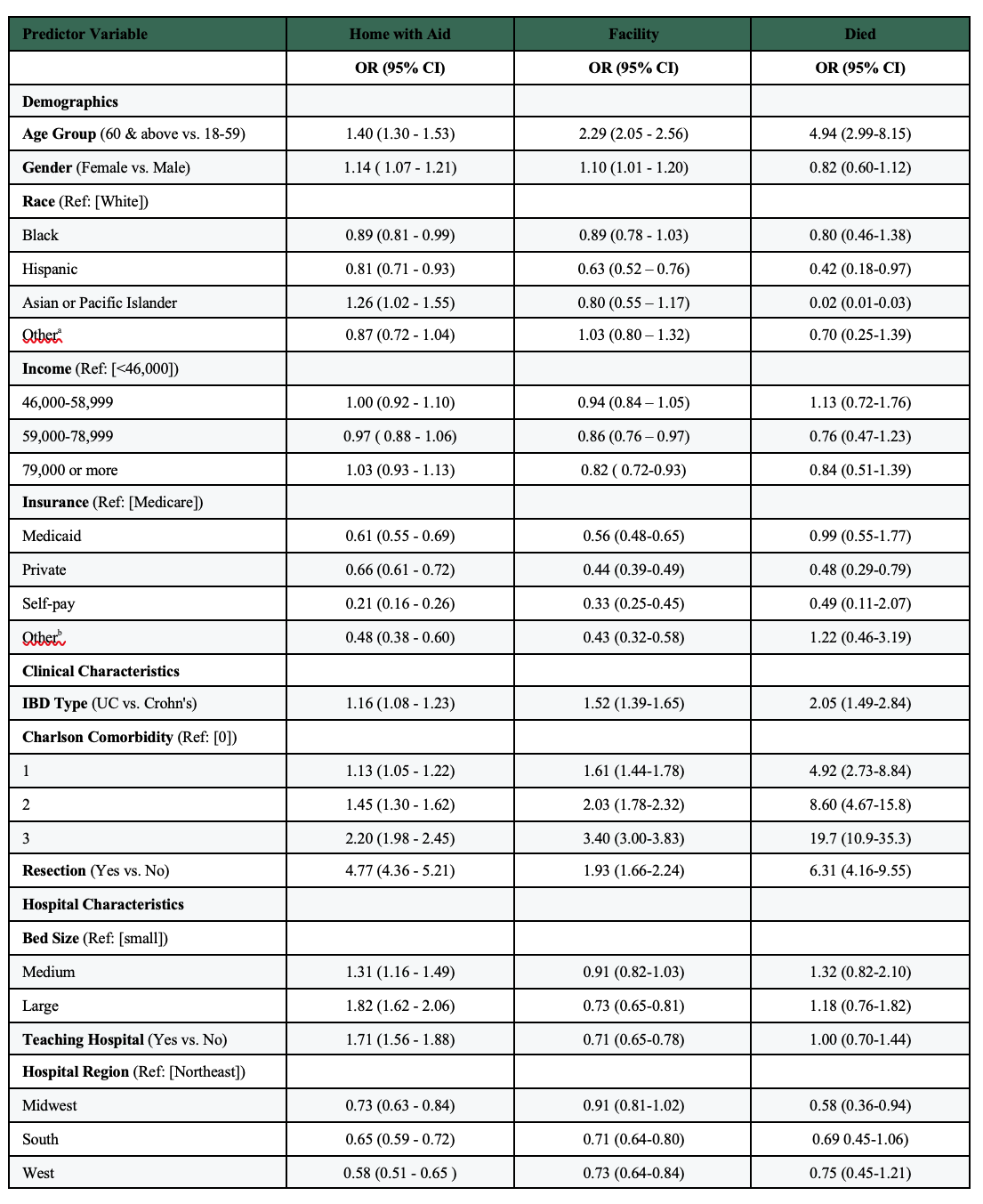
Figure: Fig 1. Discharge Disposition of the General IBD population 2016-2020
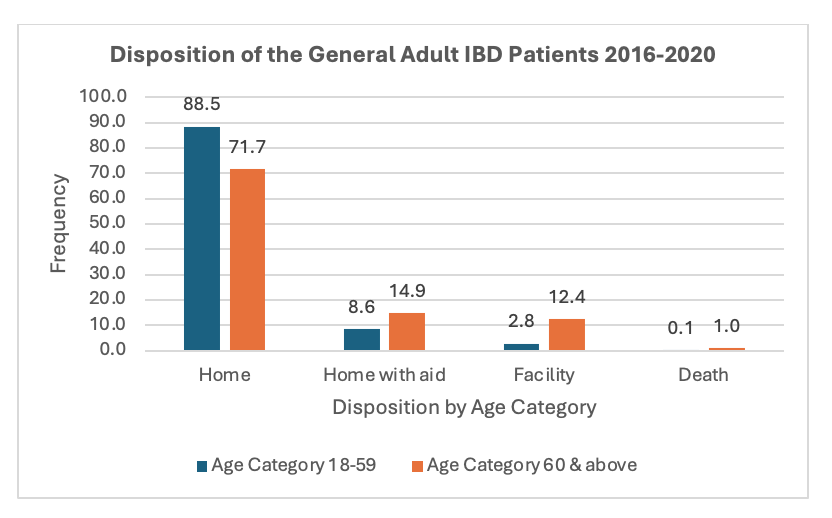
Figure: Table 1. Multivariate Regression Analysis on Discharge Disposition in the General IBD Population.
Disclosures:
Chisom Nwaneki indicated no relevant financial relationships.
Adam Faye: AbbVie – Honorarium. Eli Lilly – Consultant. NIH Grant K76AG083286 – Grant/Research Support. Takeda – Honorarium. The American College of Gastroenterology – Grant/Research Support. The Crohn's and Colitis Foundation – Grant/Research Support.
Chisom Nwaneki, MD, MPH1, Adam Faye, MD, MS2. P3271 - Discharge Disposition of Older Adults Admitted With Inflammatory Bowel Diseases: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
