Monday Poster Session
Category: IBD
P3256 - Comparative Outcomes of Surgical Monotherapy vs Adjunctive Biologic Use in Elderly Patients With Crohn’s Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Karecia Byfield, MBBS
Jefferson Einstein Hospital
Philadelphia, PA
Presenting Author(s)
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Fnu Deepali, MD2, Kevin Robinson, MBBS3, James Walter, MD3
1Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Jefferson Einstein Philadelphia Hospital, Philadelphia, PA
Introduction: Medical management of Inflammatory Bowel Disease (IBD) in the elderly remains challenging due to underrepresentation in clinical trials for newer therapy along with added complexity from comorbidities, side effects and cost concerns. Gaps in evidence for effective medical management presents an opportunity for physicians to favor surgical management. A randomized controlled trial by C.Y. Ponsioen et al. revealed that in patients with non-stricturing, limited ileocecal Crohn’s disease that is unresponsive to standard therapy, laparoscopic resection may be a viable option instead of infliximab. Similarly, a Swedish cohort study found that patients with IBD age 60 years and older had lower biologic and immunomodulator use and higher risks of bowel surgery. With the growing population of elderly patients with IBD, our study aims to explore the clinical outcomes of patients receiving surgical monotherapy vs. adjunctive biologic use in the management of Crohn’s Disease.
Methods: Data from the U.S Collaborative Network-TriNetX was used to compare clinical outcomes of patients who received surgical intervention only to those with adjunctive biologic use. Patients were divided into two groups: those with surgical intervention only and those with surgery followed by biologic use. The cohorts were propensity score-matched based on demographics, laboratory investigations e.g., C-reactive protein, medications and comorbidities such as cardiovascular disease. Patients were then followed for 1 year to assess outcomes such as mortality, need for repeat surgical intervention, hospitalization and sepsis.
Results: Both cohorts consisted of 679 patients with similar baseline characteristics after propensity score matching. The mean age was 71
± 7 years with 54% of the cohort being female. Our analysis found that within 1 year of the index event, the cohort who received surgical monotherapy, had a significantly higher risk of mortality, need for repeat surgical intervention such as colectomy, sepsis, hospitalization and ICU admission.
Discussion: Our study highlights that adjunctive biologic use after surgical intervention in elderly patients is associated with a significantly reduced risk of sepsis, repeat surgical interventions, hospitalizations and mortality. Despite concerns for medication risks and limited evidence from trials, biologics may offer improved outcomes in conjunction with surgery. Further longitudinal studies are needed to explore the therapeutic benefits of biologics in the elderly.
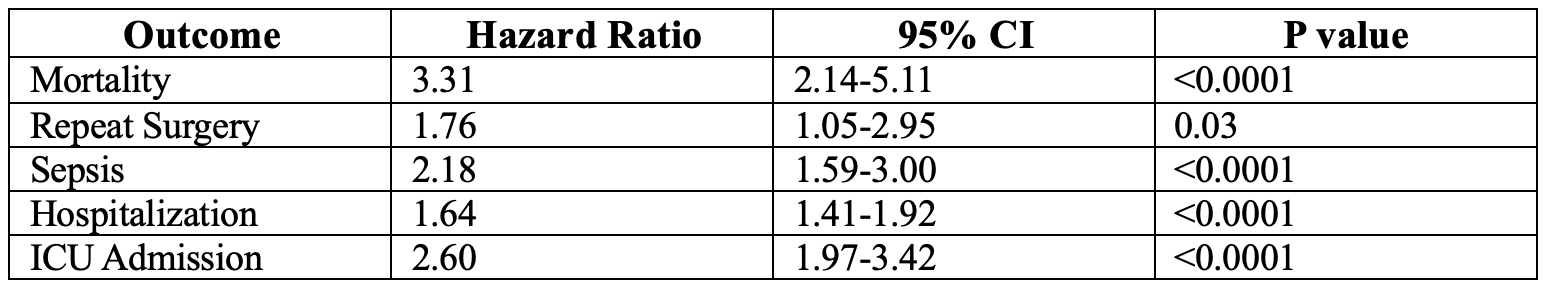
Figure: Table Showing Clinical Outcomes
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Fnu Deepali indicated no relevant financial relationships.
Kevin Robinson indicated no relevant financial relationships.
James Walter indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Fnu Deepali, MD2, Kevin Robinson, MBBS3, James Walter, MD3. P3256 - Comparative Outcomes of Surgical Monotherapy vs Adjunctive Biologic Use in Elderly Patients With Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Jefferson Einstein Philadelphia Hospital, Philadelphia, PA
Introduction: Medical management of Inflammatory Bowel Disease (IBD) in the elderly remains challenging due to underrepresentation in clinical trials for newer therapy along with added complexity from comorbidities, side effects and cost concerns. Gaps in evidence for effective medical management presents an opportunity for physicians to favor surgical management. A randomized controlled trial by C.Y. Ponsioen et al. revealed that in patients with non-stricturing, limited ileocecal Crohn’s disease that is unresponsive to standard therapy, laparoscopic resection may be a viable option instead of infliximab. Similarly, a Swedish cohort study found that patients with IBD age 60 years and older had lower biologic and immunomodulator use and higher risks of bowel surgery. With the growing population of elderly patients with IBD, our study aims to explore the clinical outcomes of patients receiving surgical monotherapy vs. adjunctive biologic use in the management of Crohn’s Disease.
Methods: Data from the U.S Collaborative Network-TriNetX was used to compare clinical outcomes of patients who received surgical intervention only to those with adjunctive biologic use. Patients were divided into two groups: those with surgical intervention only and those with surgery followed by biologic use. The cohorts were propensity score-matched based on demographics, laboratory investigations e.g., C-reactive protein, medications and comorbidities such as cardiovascular disease. Patients were then followed for 1 year to assess outcomes such as mortality, need for repeat surgical intervention, hospitalization and sepsis.
Results: Both cohorts consisted of 679 patients with similar baseline characteristics after propensity score matching. The mean age was 71
± 7 years with 54% of the cohort being female. Our analysis found that within 1 year of the index event, the cohort who received surgical monotherapy, had a significantly higher risk of mortality, need for repeat surgical intervention such as colectomy, sepsis, hospitalization and ICU admission.
Discussion: Our study highlights that adjunctive biologic use after surgical intervention in elderly patients is associated with a significantly reduced risk of sepsis, repeat surgical interventions, hospitalizations and mortality. Despite concerns for medication risks and limited evidence from trials, biologics may offer improved outcomes in conjunction with surgery. Further longitudinal studies are needed to explore the therapeutic benefits of biologics in the elderly.
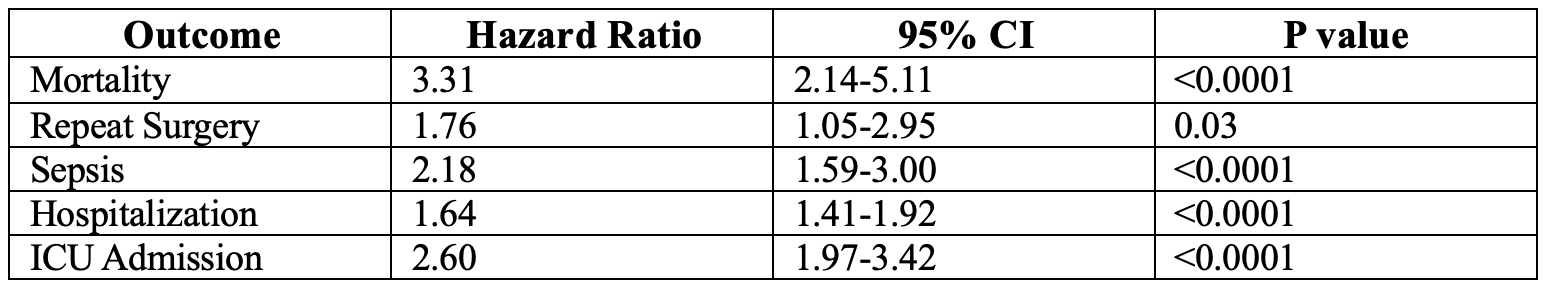
Figure: Table Showing Clinical Outcomes
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Fnu Deepali indicated no relevant financial relationships.
Kevin Robinson indicated no relevant financial relationships.
James Walter indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Fnu Deepali, MD2, Kevin Robinson, MBBS3, James Walter, MD3. P3256 - Comparative Outcomes of Surgical Monotherapy vs Adjunctive Biologic Use in Elderly Patients With Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

