Monday Poster Session
Category: IBD
P3223 - Cannabis Use and 30-Day Readmission in Inflammatory Bowel Disease: A Nationwide Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Bhargav Koyani, MBBS
Saint Francis Hospital, Evanston
Evanston, IL
Presenting Author(s)
Bhargav Koyani, MD1, Vikram Kotwal, MD2, Rajvi Pathak, MBBS3
1Ascension Saint Francis Hospital, Evanston, IL; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3GMERS Medical College and Hospital Sola, Ahmedabad, Gujarat, India
Introduction: Thirty-day readmissions following hospitalization for ulcerative colitis (UC) or Crohn’s disease (CD) impose significant clinical and economic burden. Cannabis is increasingly used by patients for symptom and pain management, but its effect on readmission outcomes remains unclear.
Methods: We conducted a retrospective cohort study using the 2021 Nationwide Readmissions Database. Adult hospitalizations for UC and CD were identified using ICD-10 codes. Index admissions excluded December discharges, and unplanned 30-day readmissions were assessed. Survey-weighted logistic regression models were used separately for UC, CD, and the overall IBD cohort to estimate odds ratios (ORs) for 30-day readmission associated with cannabis use. Models adjusted for age, sex, tobacco use, primary payer, ZIP-code income quartile, length of stay, elective and weekend admission, hospital teaching status, urban–rural category, hospital bed size, and Elixhauser comorbidity score.
Results:
Discussion: In this nationally representative sample, cannabis use was associated with a significant 30% reduction in 30-day readmission odds among patients hospitalized with ulcerative colitis that warrants further investigation. No such association was found among patients with Crohn’s disease.
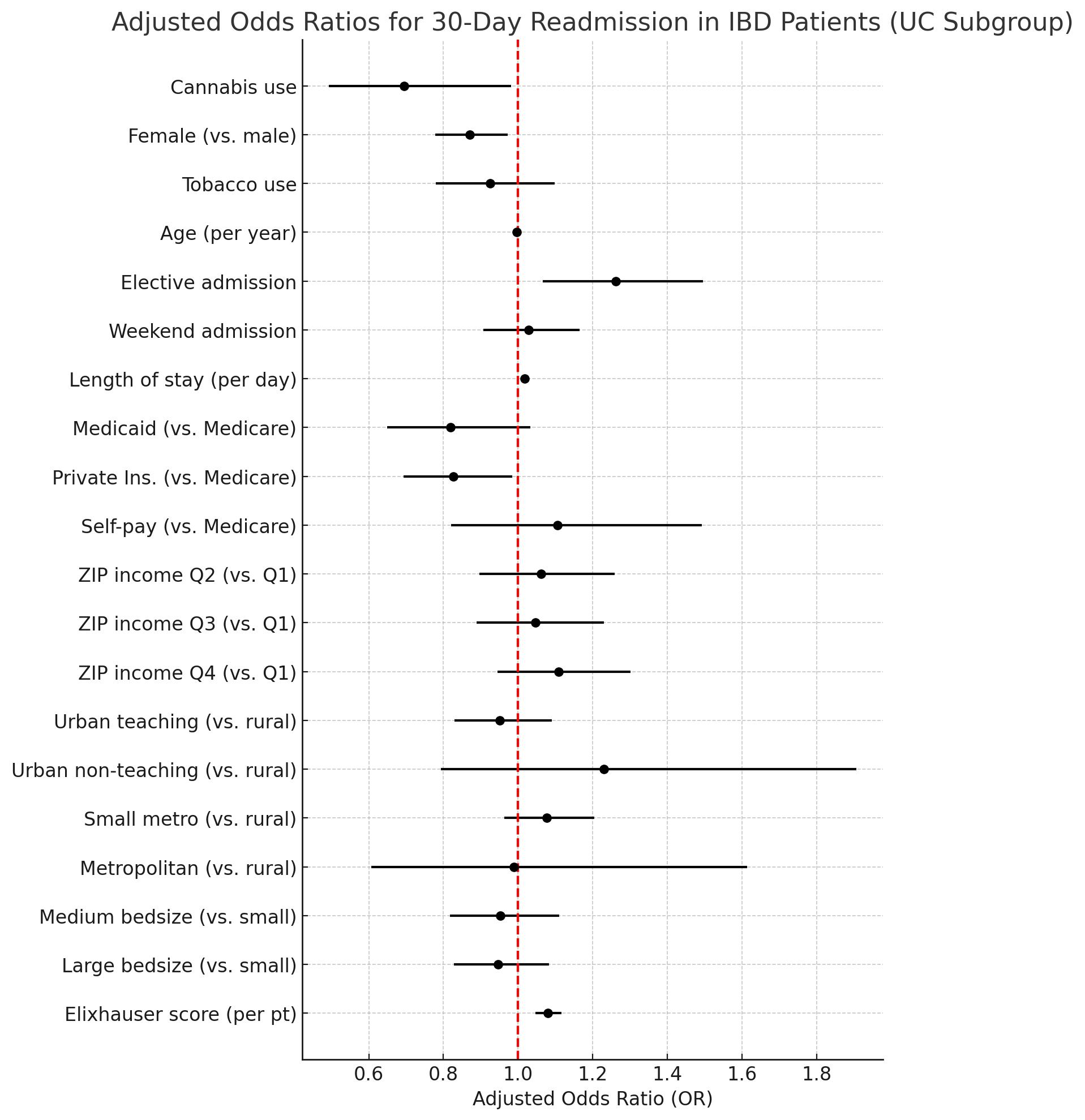
Figure: Figure 1. Forest plot showing adjusted odds ratios for 30-day readmission among hospitalized ulcerative colitis (UC) patients.
Cannabis use was associated with a significant 30% reduction in readmission risk. Estimates are adjusted for age, sex, tobacco use, payer type, income quartile, hospital characteristics, length of stay, admission type, and comorbidity burden using survey-weighted logistic regression.
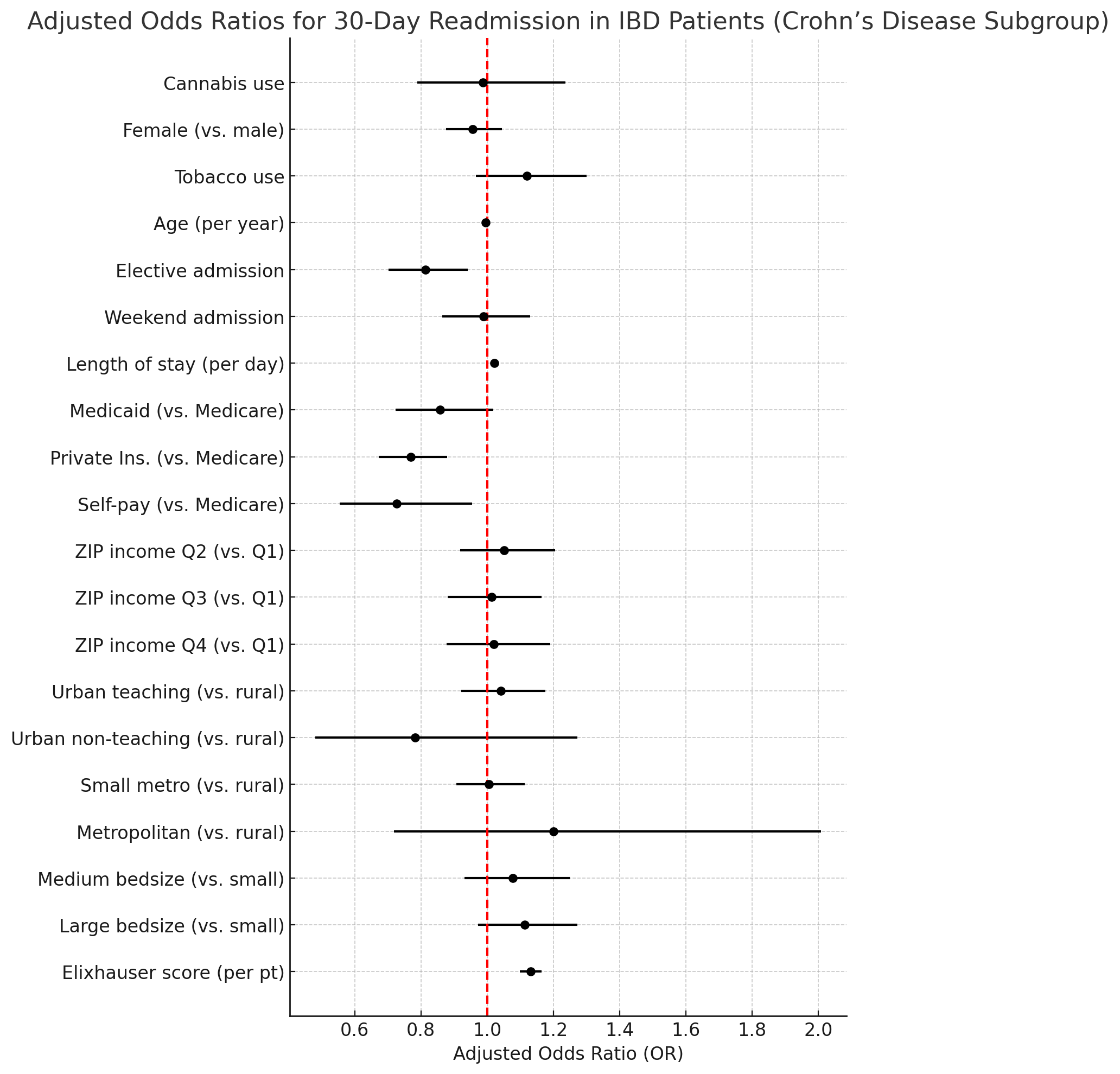
Figure: Figure 2. Forest plot showing adjusted odds ratios for 30-day readmission among hospitalized Crohn’s disease patients.
Cannabis use was not significantly associated with readmission risk. Estimates are adjusted for age, sex, tobacco use, payer type, income quartile, hospital characteristics, length of stay, admission type, and comorbidity burden using survey-weighted logistic regression.
Disclosures:
Bhargav Koyani indicated no relevant financial relationships.
Vikram Kotwal indicated no relevant financial relationships.
Rajvi Pathak indicated no relevant financial relationships.
Bhargav Koyani, MD1, Vikram Kotwal, MD2, Rajvi Pathak, MBBS3. P3223 - Cannabis Use and 30-Day Readmission in Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ascension Saint Francis Hospital, Evanston, IL; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3GMERS Medical College and Hospital Sola, Ahmedabad, Gujarat, India
Introduction: Thirty-day readmissions following hospitalization for ulcerative colitis (UC) or Crohn’s disease (CD) impose significant clinical and economic burden. Cannabis is increasingly used by patients for symptom and pain management, but its effect on readmission outcomes remains unclear.
Methods: We conducted a retrospective cohort study using the 2021 Nationwide Readmissions Database. Adult hospitalizations for UC and CD were identified using ICD-10 codes. Index admissions excluded December discharges, and unplanned 30-day readmissions were assessed. Survey-weighted logistic regression models were used separately for UC, CD, and the overall IBD cohort to estimate odds ratios (ORs) for 30-day readmission associated with cannabis use. Models adjusted for age, sex, tobacco use, primary payer, ZIP-code income quartile, length of stay, elective and weekend admission, hospital teaching status, urban–rural category, hospital bed size, and Elixhauser comorbidity score.
Results:
- Ulcerative colitis (n=12,500; weighted population=23,395): Cannabis use was associated with a 30% reduction in the odds of 30-day readmission (OR 0.70; 95% CI 0.49–0.98; p=0.039). Female sex was protective, while elective admission, longer hospital stay, and higher comorbidity burden were associated with increased risk. Tobacco use was not significantly associated with readmission.
- Crohn’s disease (n=18,363; weighted population=35,993): Cannabis use was not significantly associated with 30-day readmission (OR 0.99; 95% CI 0.79–1.24; p=0.915). Elective admission and older age were associated with reduced risk, while longer hospital stay and higher comorbidity burden were associated with increased readmission risk. Tobacco use was not a significant predictor.
- IBD cohort (n=30,863; weighted population=59,389): Cannabis use was not significantly associated with 30-day readmission (OR 0.90; 95% CI 0.75–1.09; p=0.269). Older age, female sex, and Medicaid insurance were associated with reduced risk, while longer hospital stay and higher comorbidity burden increased readmission risk.
Discussion: In this nationally representative sample, cannabis use was associated with a significant 30% reduction in 30-day readmission odds among patients hospitalized with ulcerative colitis that warrants further investigation. No such association was found among patients with Crohn’s disease.
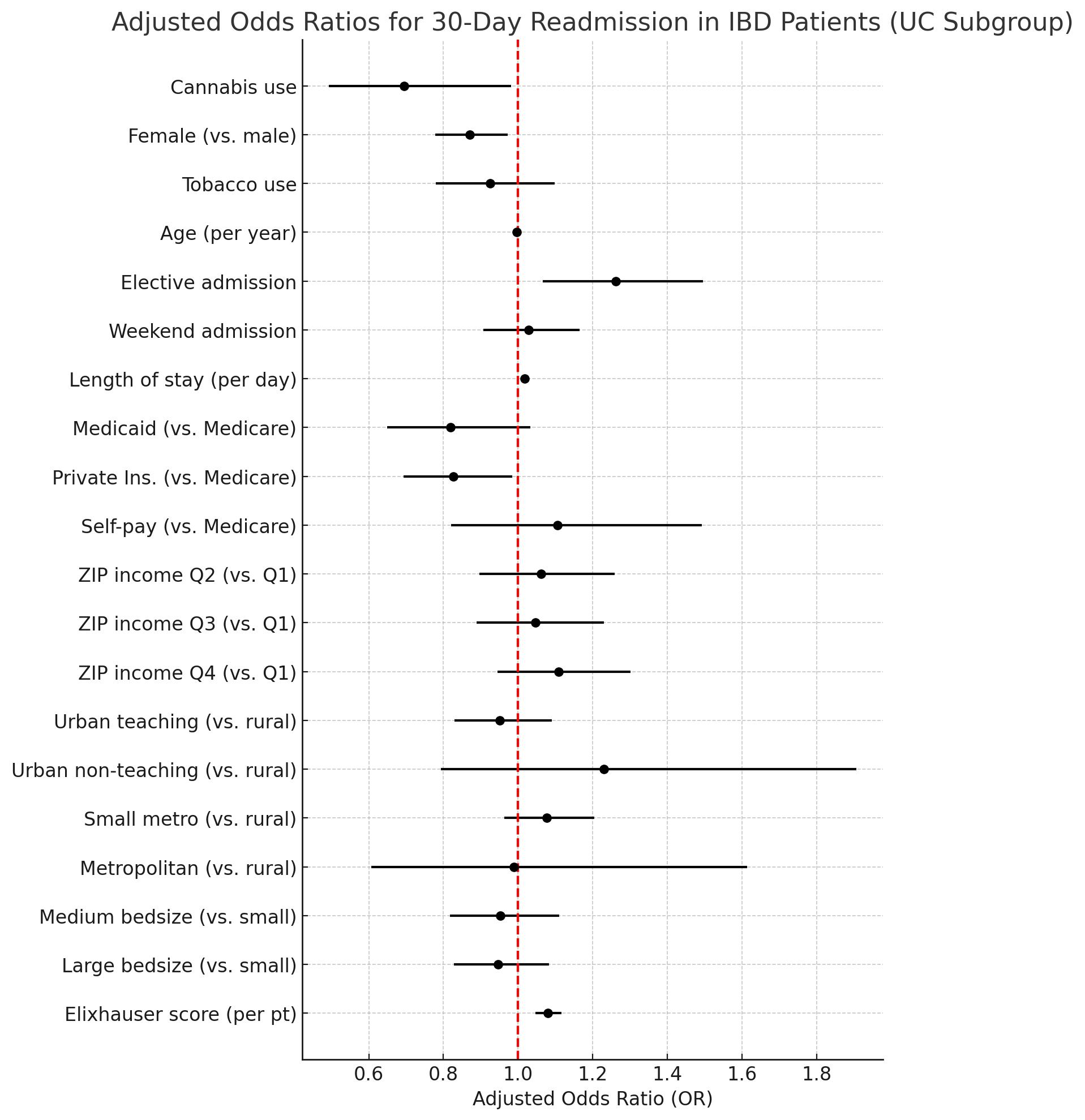
Figure: Figure 1. Forest plot showing adjusted odds ratios for 30-day readmission among hospitalized ulcerative colitis (UC) patients.
Cannabis use was associated with a significant 30% reduction in readmission risk. Estimates are adjusted for age, sex, tobacco use, payer type, income quartile, hospital characteristics, length of stay, admission type, and comorbidity burden using survey-weighted logistic regression.
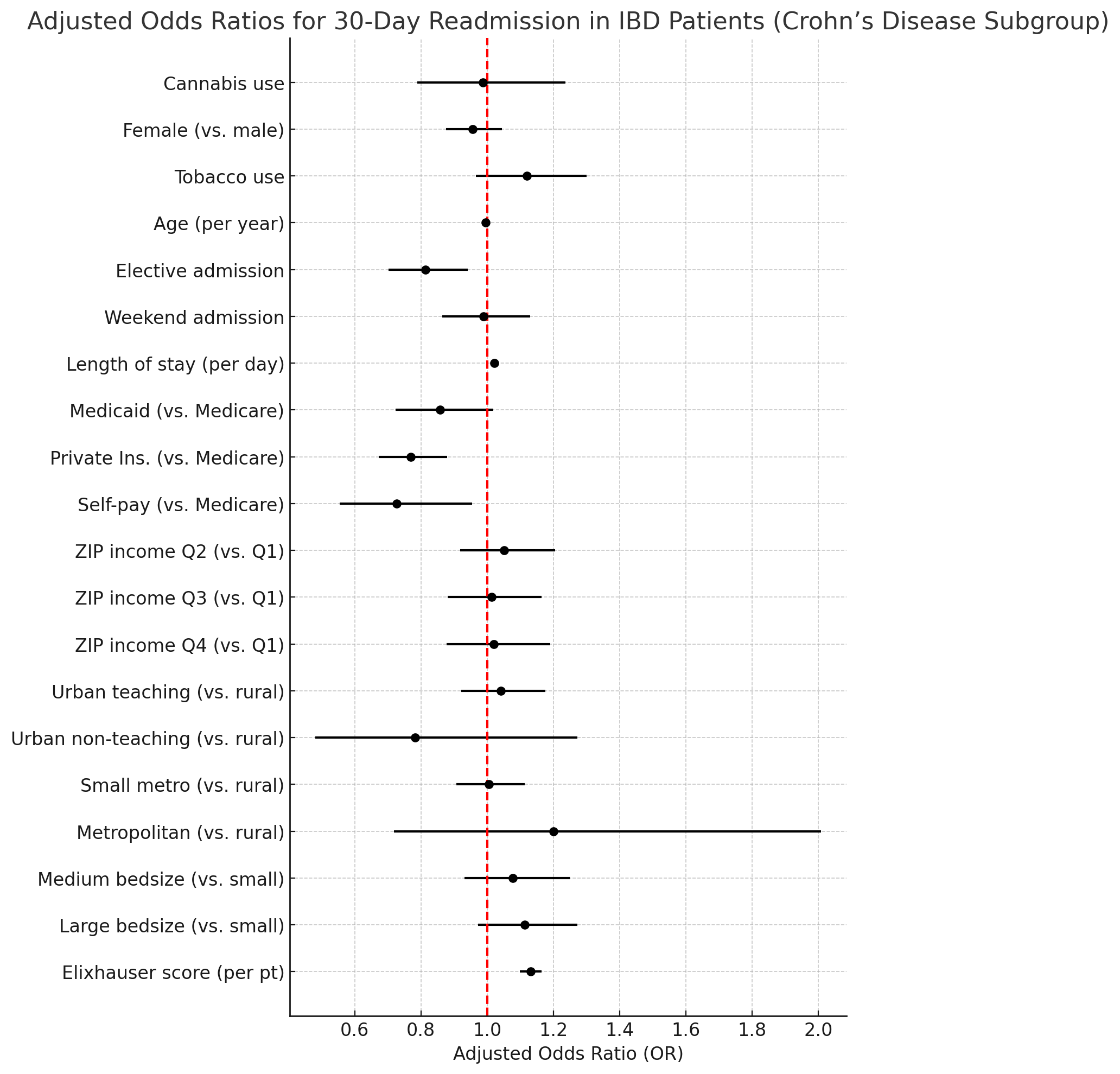
Figure: Figure 2. Forest plot showing adjusted odds ratios for 30-day readmission among hospitalized Crohn’s disease patients.
Cannabis use was not significantly associated with readmission risk. Estimates are adjusted for age, sex, tobacco use, payer type, income quartile, hospital characteristics, length of stay, admission type, and comorbidity burden using survey-weighted logistic regression.
Disclosures:
Bhargav Koyani indicated no relevant financial relationships.
Vikram Kotwal indicated no relevant financial relationships.
Rajvi Pathak indicated no relevant financial relationships.
Bhargav Koyani, MD1, Vikram Kotwal, MD2, Rajvi Pathak, MBBS3. P3223 - Cannabis Use and 30-Day Readmission in Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
