Monday Poster Session
Category: IBD
P3199 - Can an IBD Polygenic Risk Score Function as an IBD Polygenic Prognosis Score? Modeling Genetic Biomarkers for Prognostic Insight in Established IBD
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rohit Aita, BA
University of Pittsburgh School of Medicine
Pittsburgh, PA
Presenting Author(s)
Rohit Aita, BA1, Claudia Ramos-Rivers, MD2, David Binion, MD2
1University of Pittsburgh School of Medicine, Pittsburgh, PA; 2University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: With over 240 polymorphisms identified, the genetic architecture underlying risk of developing IBD is well characterized, but the prognostic potential of polygenic risk polymorphisms to predict future IBD disease trajectory remains unclear. We hypothesized that multiyear patterns of healthcare utilization, organized as mean annual healthcare charges ≥ 3 years, would serve as a proxy for multiyear IBD severity, facilitating identification of genetic polymorphisms associated with more severe disease trajectories.
Methods: Models for genomic severity biomarker identification were generated from consented IBD patients (Figure 1A), followed over multiple years, with multiyear mean healthcare charges as a severity phenotype. The genomic model for a Polygenic Prognosis Score repurposed a Polygenic Risk Score (PRS) based on leveraging 2 different datasets as base data (Liu et al, Nature Genetics, 2015 and De Lange et al, Nature Genetics, 2017). PLINK v1.90b7 and R version 4.4.0-4.4.1 packages were employed to plot single nucleotide polymorphisms (SNPs) per 4 high risk genes (ATG16L1, NOD2, IRGM, IL23) against mean healthcare charges, and downstream statistical analyses.
Results: Among the 868 IBD patients (male 53%; Crohn’s disease 55%), IBD risk polymorphisms occurred in most patients, with IL23R polymorphisms being most common (Figure 2A). We observe a scattered distribution of SNPs across the mean multiyear healthcare charge spectrum, supporting no association with charge severity and explaining lack of correlation between PRS and healthcare charges (Figure 1B). We only find a weak, yet significant positive correlation (Spearman’s rank: ρ = 0.08, P < 0.05) between the burden of NOD2 SNPs and multiyear health charges as supported by the Kruskal-Wallis test P < 0.05, Dunn’s post-hoc testing showing P < 0.05 between (1) 1-2 NOD2 SNPs vs 3-4 NOD2 SNPs and (2) 3-4 NOD2 SNPs vs No NOD2 SNPs. This finding is similarly seen in all four genes when combined, yet the group with at least 13 SNPs is not in any significant Dunn’s post-hoc pairwise comparison (Figure 2B).
Discussion: An increased burden of high-risk alleles is not associated with increasing multiyear healthcare charges in established IBD patients. However, an increased burden of up to 3-4 NOD2 SNPs may be correlated with higher multiyear healthcare charges. This study confirms that genetics may offer only limited prognostic value for prediction of disease severity in established IBD.
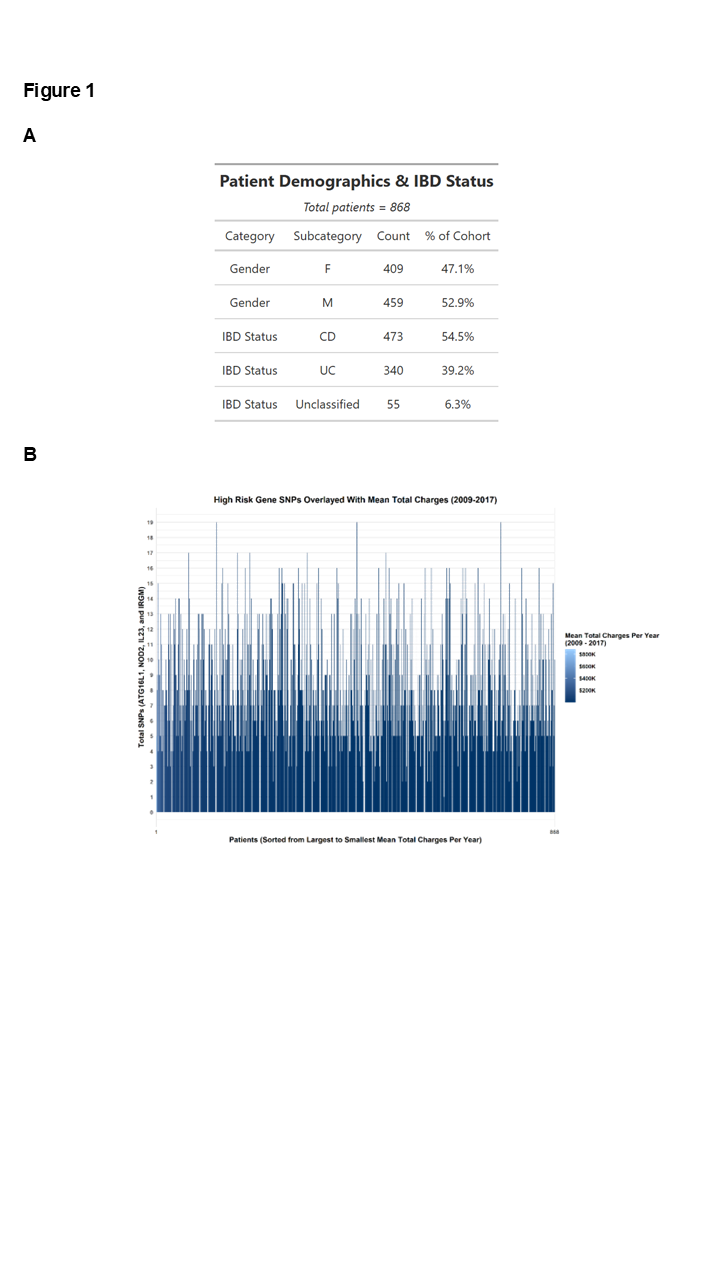
Figure: Figure 1. A. Patient Demographics B. High Risk Gene SNPs Overlayed with Mean Total Charges
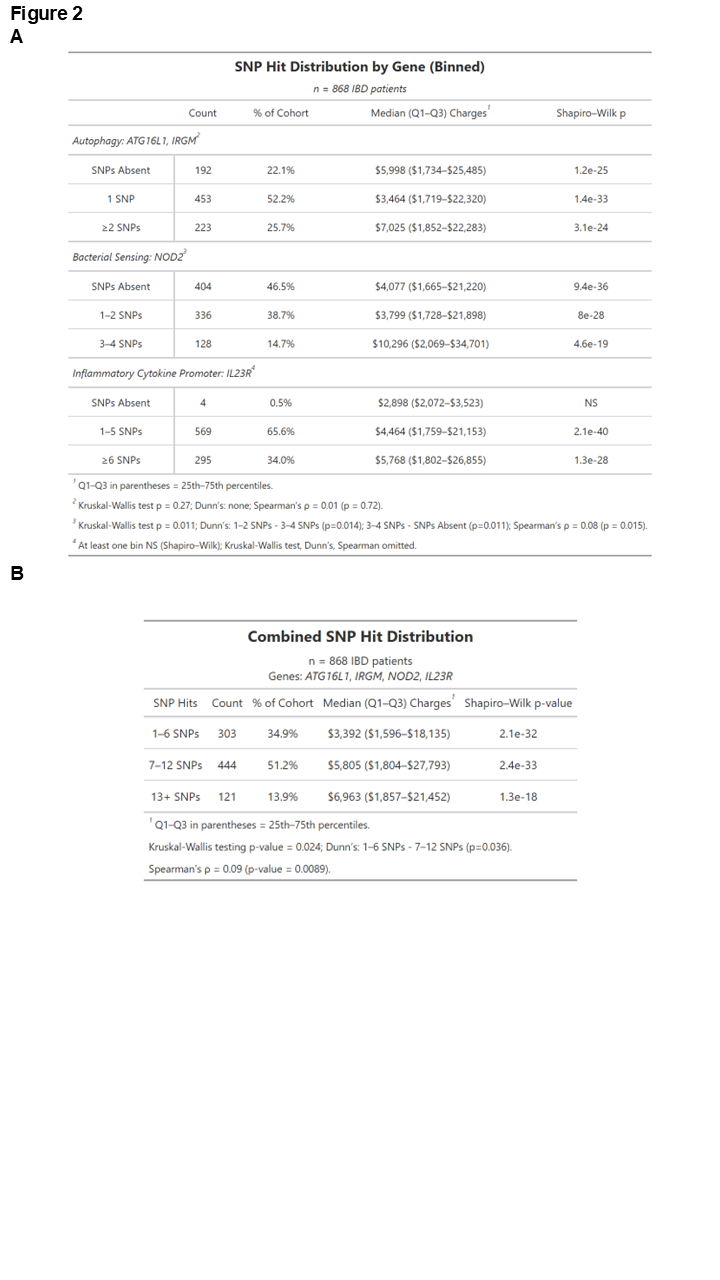
Figure: Figure 2. A. Multiyear Health Charges Separated by High Risk Variants involved in Autophagy, Bacterial Sensing, and Inflammatory Pathways B. Multiyear Health Charges in all High Risk Variants involved in Autophagy, Bacterial Sensing, and Inflammatory Pathways
Disclosures:
Rohit Aita: Abbvie – Besides stock options, Abbvie Immunology scholarship, Stock-publicly held company(excluding mutual/index funds). EveryLife Foundation for Rare Diseases – Scholarship. Health Catalyst – Stock-publicly held company(excluding mutual/index funds). Microsoft – Stock-publicly held company(excluding mutual/index funds). Safety Shot – Stock-publicly held company(excluding mutual/index funds). Salix Pharmaceuticals – Gastrointestinal Health Scholars Graduate Student Scholarship. South Asian IBD Alliance – Honorarium.
Claudia Ramos-Rivers indicated no relevant financial relationships.
David Binion: Blueprint Medicines – Grant/Research Support. Mirador Therapeutics – Grant/Research Support. Takeda – Grant/Research Support.
Rohit Aita, BA1, Claudia Ramos-Rivers, MD2, David Binion, MD2. P3199 - Can an IBD Polygenic Risk Score Function as an IBD Polygenic Prognosis Score? Modeling Genetic Biomarkers for Prognostic Insight in Established IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh School of Medicine, Pittsburgh, PA; 2University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: With over 240 polymorphisms identified, the genetic architecture underlying risk of developing IBD is well characterized, but the prognostic potential of polygenic risk polymorphisms to predict future IBD disease trajectory remains unclear. We hypothesized that multiyear patterns of healthcare utilization, organized as mean annual healthcare charges ≥ 3 years, would serve as a proxy for multiyear IBD severity, facilitating identification of genetic polymorphisms associated with more severe disease trajectories.
Methods: Models for genomic severity biomarker identification were generated from consented IBD patients (Figure 1A), followed over multiple years, with multiyear mean healthcare charges as a severity phenotype. The genomic model for a Polygenic Prognosis Score repurposed a Polygenic Risk Score (PRS) based on leveraging 2 different datasets as base data (Liu et al, Nature Genetics, 2015 and De Lange et al, Nature Genetics, 2017). PLINK v1.90b7 and R version 4.4.0-4.4.1 packages were employed to plot single nucleotide polymorphisms (SNPs) per 4 high risk genes (ATG16L1, NOD2, IRGM, IL23) against mean healthcare charges, and downstream statistical analyses.
Results: Among the 868 IBD patients (male 53%; Crohn’s disease 55%), IBD risk polymorphisms occurred in most patients, with IL23R polymorphisms being most common (Figure 2A). We observe a scattered distribution of SNPs across the mean multiyear healthcare charge spectrum, supporting no association with charge severity and explaining lack of correlation between PRS and healthcare charges (Figure 1B). We only find a weak, yet significant positive correlation (Spearman’s rank: ρ = 0.08, P < 0.05) between the burden of NOD2 SNPs and multiyear health charges as supported by the Kruskal-Wallis test P < 0.05, Dunn’s post-hoc testing showing P < 0.05 between (1) 1-2 NOD2 SNPs vs 3-4 NOD2 SNPs and (2) 3-4 NOD2 SNPs vs No NOD2 SNPs. This finding is similarly seen in all four genes when combined, yet the group with at least 13 SNPs is not in any significant Dunn’s post-hoc pairwise comparison (Figure 2B).
Discussion: An increased burden of high-risk alleles is not associated with increasing multiyear healthcare charges in established IBD patients. However, an increased burden of up to 3-4 NOD2 SNPs may be correlated with higher multiyear healthcare charges. This study confirms that genetics may offer only limited prognostic value for prediction of disease severity in established IBD.
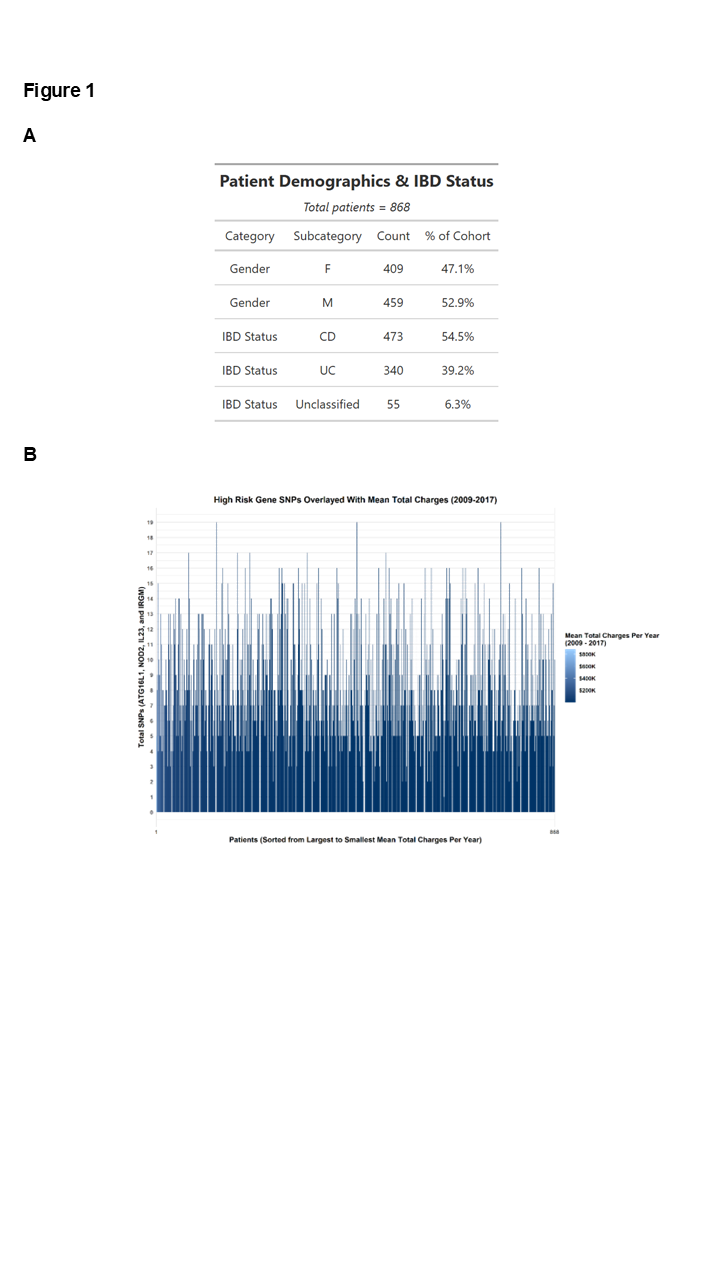
Figure: Figure 1. A. Patient Demographics B. High Risk Gene SNPs Overlayed with Mean Total Charges
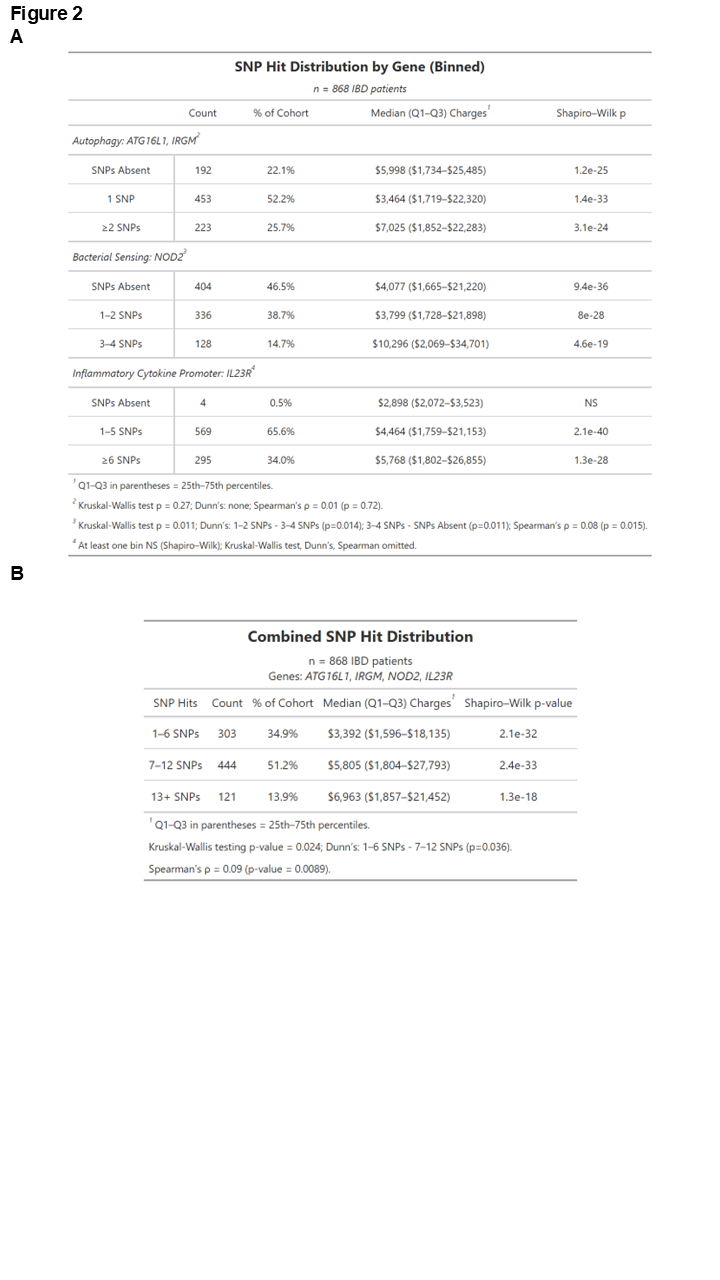
Figure: Figure 2. A. Multiyear Health Charges Separated by High Risk Variants involved in Autophagy, Bacterial Sensing, and Inflammatory Pathways B. Multiyear Health Charges in all High Risk Variants involved in Autophagy, Bacterial Sensing, and Inflammatory Pathways
Disclosures:
Rohit Aita: Abbvie – Besides stock options, Abbvie Immunology scholarship, Stock-publicly held company(excluding mutual/index funds). EveryLife Foundation for Rare Diseases – Scholarship. Health Catalyst – Stock-publicly held company(excluding mutual/index funds). Microsoft – Stock-publicly held company(excluding mutual/index funds). Safety Shot – Stock-publicly held company(excluding mutual/index funds). Salix Pharmaceuticals – Gastrointestinal Health Scholars Graduate Student Scholarship. South Asian IBD Alliance – Honorarium.
Claudia Ramos-Rivers indicated no relevant financial relationships.
David Binion: Blueprint Medicines – Grant/Research Support. Mirador Therapeutics – Grant/Research Support. Takeda – Grant/Research Support.
Rohit Aita, BA1, Claudia Ramos-Rivers, MD2, David Binion, MD2. P3199 - Can an IBD Polygenic Risk Score Function as an IBD Polygenic Prognosis Score? Modeling Genetic Biomarkers for Prognostic Insight in Established IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
