Monday Poster Session
Category: IBD
P3188 - Adherence to a Mediterranean Diet is Not Associated With Reduced Risk of Development of Microscopic Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rachel Zhang, BS (she/her/hers)
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Rachel Zhang, BS1, Kristin Burke, MD, MPH1, Ashwin Ananthakrishnan, 2, Emily Lopes, MD, MPH1, James M. Richter, MD, MA3, Andrew Chan, MD, MPH1, Hamed Khalili, MD, MPH1
1Massachusetts General Hospital, Boston, MA; 2Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA; 3Mass General Brigham, Boston, MA
Introduction: The pathogenesis of microscopic colitis (MC) has been attributed to an immune response to changes in the gut microenvironment. Diet is the single largest contributor to the gut microenvironment through its influence on microbiome composition/function and epithelial barrier function. Following a Mediterranean diet has been shown to alter gut microbiome composition, reduce inflammatory mediators, and positively impact intestinal epithelial permeability. Nevertheless, the impact of following a Mediterranean diet on risk of MC development has never been studied. In two nationwide prospective cohorts we analyzed the association between Mediterranean diet adherence and risk of developing MC.
Methods: We performed a prospective cohort study including 169,343 women without a baseline diagnosis of MC in the Nurses’ Health Study (NHS) and NHS II. Through validated semiquantitative food frequency questionnaires ascertained every 4 years beginning in 1990 in NHS and 1991 in NHSII, we derived alternate Mediterranean diet (aMED) scores based on intake of vegetables, fruit, nuts, whole grains, legumes, fish, red/processed meat, alcohol, and monosaturated-to-saturated-fat ratio. Higher scores indicated increased Mediterranean diet adherence. MC diagnoses were confirmed through review of histopathology. Using Cox proportional hazards modeling, we estimated the multivariable-adjusted hazard ratios (aHR) and their respective 95% confidence intervals (CI) for development of MC according to quartiles of aMED score while adjusting for potential confounders.
Results: Between 1990 and 2015, we confirmed 213 incident MC cases over 2,959,527 person-years. There was no association between aMED score and risk of developing MC. The aHR of MC was 1.23 (95% CI 0.85 - 1.78) in the highest quartile of aMED score as compared to the lowest (ptrend = 0.21, table 1). The results did not vary based on MC subtype (pheterogeneity = 0.83). We also analyzed the association between the individual aMED components and risk of MC. A positive association was identified between alcohol intake and risk of MC with an aHR of MC of 1.30 (95% CI 1.13-1.49) for each drink of alcohol consumed per day.
Discussion: In 2 large prospective cohorts of US women, there was no association between Mediterranean diet adherence and risk of development of MC. Alcohol intake is associated with MC development. Further studies should address the role of alcohol avoidance in mitigating MC.
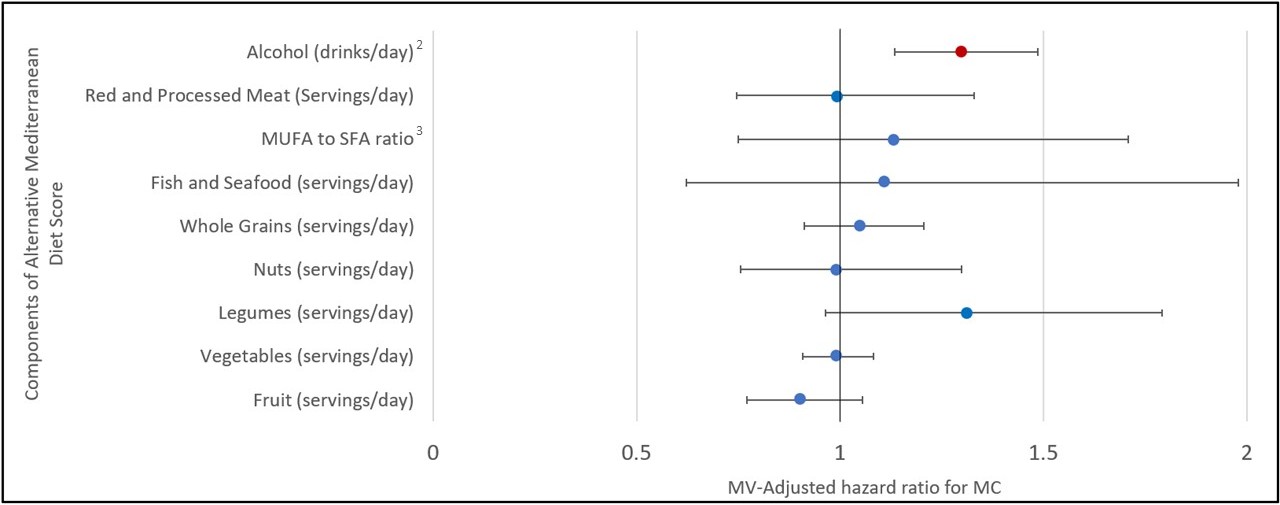
Figure: Table 1: Age-adjusted and multivariable-adjusted risk of microscopic colitis by aMED quartile in the Nurses’ Health Study I and II
1Uses aMED score from most recent cycle before diagnosis; Adjusted for age (months), cohort (NHS 1, NHS2), total calories (kcal per day), physical activity (MET-hr/week), body mass index ( <20, 20-24.9, 25-29.9, ≥30), smoking (never, past, current), menopausal status and menopausal hormone therapy (MHT) use (pre-menopausal, post-menopausal never-MHT use, post-menopausal past MHT use, post-menopausal current MHT use), and NSAID use
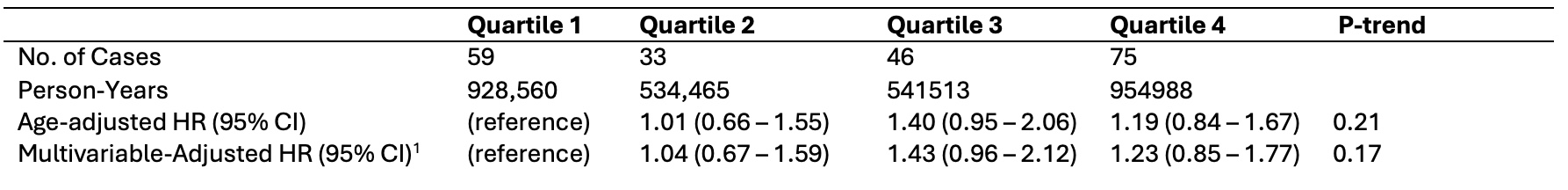
Figure: Figure 1: Multivariable-adjusted risk of microscopic colitis by intake of individual components of the Alternative Mediterranean Diet Score
1Adjusted for other aMED components, age (months), cohort (NHS 1, NHS2), total calories (kcal per day), physical activity (MET-hr/week), body mass index ( <20, 20-24.9, 25-29.9, ≥30), smoking (never, past, current), menopausal status and menopausal hormone therapy (MHT) use (pre-menopausal, post-menopausal never-MHT use, post-menopausal past MHT use, post-menopausal current MHT use), and NSAID use
2One standard drink = 14 grams of alcohol
3The ratio of MonoUnsaturated Fatty Acids to Saturated Fatty Acids
Disclosures:
Rachel Zhang indicated no relevant financial relationships.
Kristin Burke: Janssen – Advisor or Review Panel Member.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Emily Lopes indicated no relevant financial relationships.
James M. Richter indicated no relevant financial relationships.
Andrew Chan: Pfizer – Consultant.
Hamed Khalili: Abbvie – Grant/Research Support.
Rachel Zhang, BS1, Kristin Burke, MD, MPH1, Ashwin Ananthakrishnan, 2, Emily Lopes, MD, MPH1, James M. Richter, MD, MA3, Andrew Chan, MD, MPH1, Hamed Khalili, MD, MPH1. P3188 - Adherence to a Mediterranean Diet is Not Associated With Reduced Risk of Development of Microscopic Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA; 3Mass General Brigham, Boston, MA
Introduction: The pathogenesis of microscopic colitis (MC) has been attributed to an immune response to changes in the gut microenvironment. Diet is the single largest contributor to the gut microenvironment through its influence on microbiome composition/function and epithelial barrier function. Following a Mediterranean diet has been shown to alter gut microbiome composition, reduce inflammatory mediators, and positively impact intestinal epithelial permeability. Nevertheless, the impact of following a Mediterranean diet on risk of MC development has never been studied. In two nationwide prospective cohorts we analyzed the association between Mediterranean diet adherence and risk of developing MC.
Methods: We performed a prospective cohort study including 169,343 women without a baseline diagnosis of MC in the Nurses’ Health Study (NHS) and NHS II. Through validated semiquantitative food frequency questionnaires ascertained every 4 years beginning in 1990 in NHS and 1991 in NHSII, we derived alternate Mediterranean diet (aMED) scores based on intake of vegetables, fruit, nuts, whole grains, legumes, fish, red/processed meat, alcohol, and monosaturated-to-saturated-fat ratio. Higher scores indicated increased Mediterranean diet adherence. MC diagnoses were confirmed through review of histopathology. Using Cox proportional hazards modeling, we estimated the multivariable-adjusted hazard ratios (aHR) and their respective 95% confidence intervals (CI) for development of MC according to quartiles of aMED score while adjusting for potential confounders.
Results: Between 1990 and 2015, we confirmed 213 incident MC cases over 2,959,527 person-years. There was no association between aMED score and risk of developing MC. The aHR of MC was 1.23 (95% CI 0.85 - 1.78) in the highest quartile of aMED score as compared to the lowest (ptrend = 0.21, table 1). The results did not vary based on MC subtype (pheterogeneity = 0.83). We also analyzed the association between the individual aMED components and risk of MC. A positive association was identified between alcohol intake and risk of MC with an aHR of MC of 1.30 (95% CI 1.13-1.49) for each drink of alcohol consumed per day.
Discussion: In 2 large prospective cohorts of US women, there was no association between Mediterranean diet adherence and risk of development of MC. Alcohol intake is associated with MC development. Further studies should address the role of alcohol avoidance in mitigating MC.
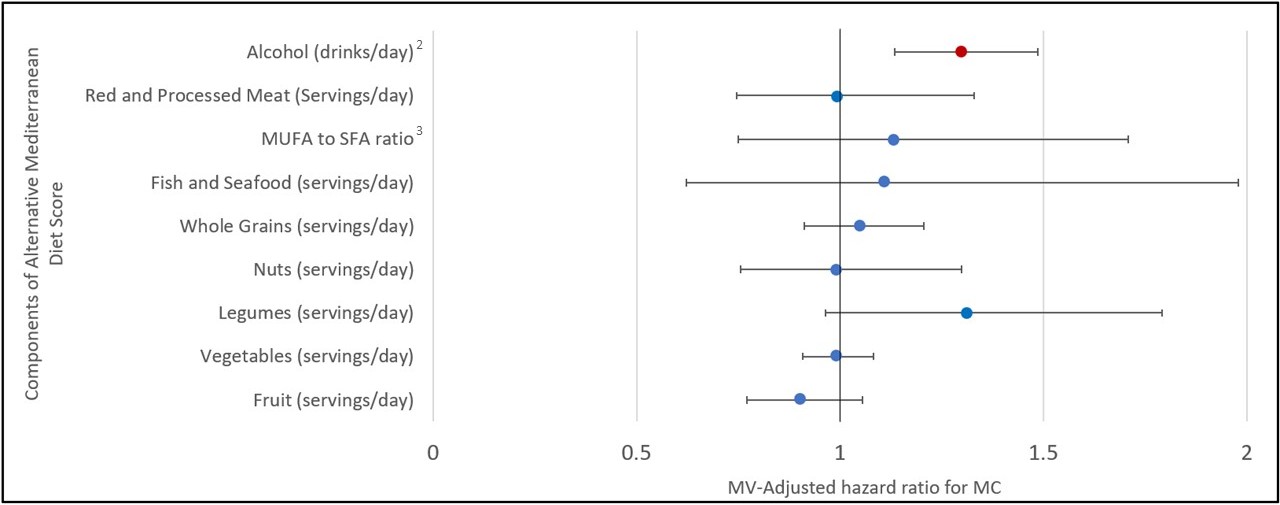
Figure: Table 1: Age-adjusted and multivariable-adjusted risk of microscopic colitis by aMED quartile in the Nurses’ Health Study I and II
1Uses aMED score from most recent cycle before diagnosis; Adjusted for age (months), cohort (NHS 1, NHS2), total calories (kcal per day), physical activity (MET-hr/week), body mass index ( <20, 20-24.9, 25-29.9, ≥30), smoking (never, past, current), menopausal status and menopausal hormone therapy (MHT) use (pre-menopausal, post-menopausal never-MHT use, post-menopausal past MHT use, post-menopausal current MHT use), and NSAID use
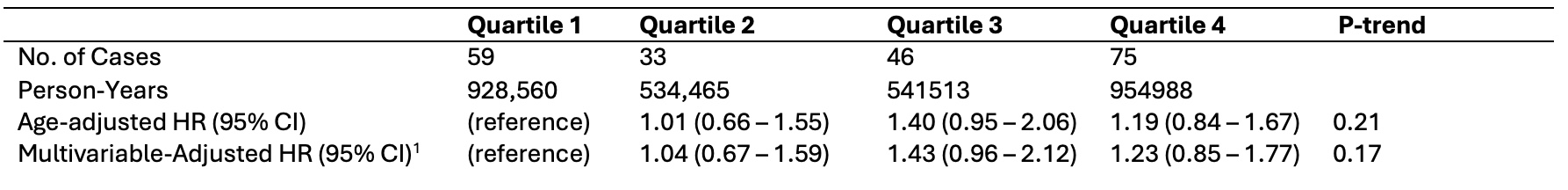
Figure: Figure 1: Multivariable-adjusted risk of microscopic colitis by intake of individual components of the Alternative Mediterranean Diet Score
1Adjusted for other aMED components, age (months), cohort (NHS 1, NHS2), total calories (kcal per day), physical activity (MET-hr/week), body mass index ( <20, 20-24.9, 25-29.9, ≥30), smoking (never, past, current), menopausal status and menopausal hormone therapy (MHT) use (pre-menopausal, post-menopausal never-MHT use, post-menopausal past MHT use, post-menopausal current MHT use), and NSAID use
2One standard drink = 14 grams of alcohol
3The ratio of MonoUnsaturated Fatty Acids to Saturated Fatty Acids
Disclosures:
Rachel Zhang indicated no relevant financial relationships.
Kristin Burke: Janssen – Advisor or Review Panel Member.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Emily Lopes indicated no relevant financial relationships.
James M. Richter indicated no relevant financial relationships.
Andrew Chan: Pfizer – Consultant.
Hamed Khalili: Abbvie – Grant/Research Support.
Rachel Zhang, BS1, Kristin Burke, MD, MPH1, Ashwin Ananthakrishnan, 2, Emily Lopes, MD, MPH1, James M. Richter, MD, MA3, Andrew Chan, MD, MPH1, Hamed Khalili, MD, MPH1. P3188 - Adherence to a Mediterranean Diet is Not Associated With Reduced Risk of Development of Microscopic Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
