Monday Poster Session
Category: IBD
P3185 - Diverging Trajectories: Trends in Intestinal Ultrasound Utilization for IBD Across Academic and Non-Academic Institutions (2017–2024)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Silpa Choday, MD2, Khyati Bidani, MD3, Indu Srinivasan, MD2, Wael Youssef, MD2
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Intestinal ultrasound (IUS) has emerged as a valuable, non-invasive tool for real-time assessment of disease activity in patients with inflammatory bowel disease (IBD). While widely adopted in European clinical practice, IUS implementation in the United States has been slower and potentially uneven across healthcare settings. Academic centers, often at the forefront of adopting novel technologies, may integrate IUS more readily than non-academic institutions. Understanding this differential uptake is crucial to ensuring equitable access to advanced diagnostics. This study evaluates temporal trends in IUS utilization among IBD patients at academic vs non-academic centers in a large, multi-institutional real-world dataset.
Methods: We queried the TriNetX US Collaborative Network for adult IBD patients (ICD-10: K50, K51) between 2017 and 2024. IUS procedures were identified using CPT and ICD-10-PCS codes. The incidence proportion of IUS was calculated annually. Patients were stratified by institution type (academic vs. non-academic), age, sex, race, and ethnicity.
Results: Among 488,673 patients in academic centers and 196,051 in non-academic centers, IUS use increased in both groups over the 8 years. In academic centers, IUS incidence rose from 1.9% in 2017 to 3.03% in 2024, showing a steeper increase. In non-academic centers, the increase was slower, from 1.75% to 2.76%. Hispanic patients had the highest rise in IUS use in both settings, peaking at 4.26% (academic) vs 5.77% (non-academic) in 2024. Additionally, Female patients demonstrated slightly higher IUS use in both cohorts. Furthermore, Peak use occurred in the 30–59 age range, steadily increasing across all groups. Use was highest among Asian and White patients in academic centers; in non-academic centers, disparities were more evident with lower rates in Black patients.
Discussion: Over eight years, IUS utilization in IBD care has significantly increased across both academic and non-academic institutions, with academic centers demonstrating a more consistent rise. Disparities in adoption by institution type, race, ethnicity, and sex were evident, with Hispanic and female patients showing higher rates of IUS use. These findings underscore the growing integration of IUS into IBD care pathways but also highlight gaps in uniform access. Targeted dissemination strategies, broader provider education, and infrastructure support are needed to bridge these disparities and promote equitable adoption of IUS across all clinical settings.

Figure: Figure 2: Line graph showing the trends of IUS based on age, gender and ethinicity amongst academic centers
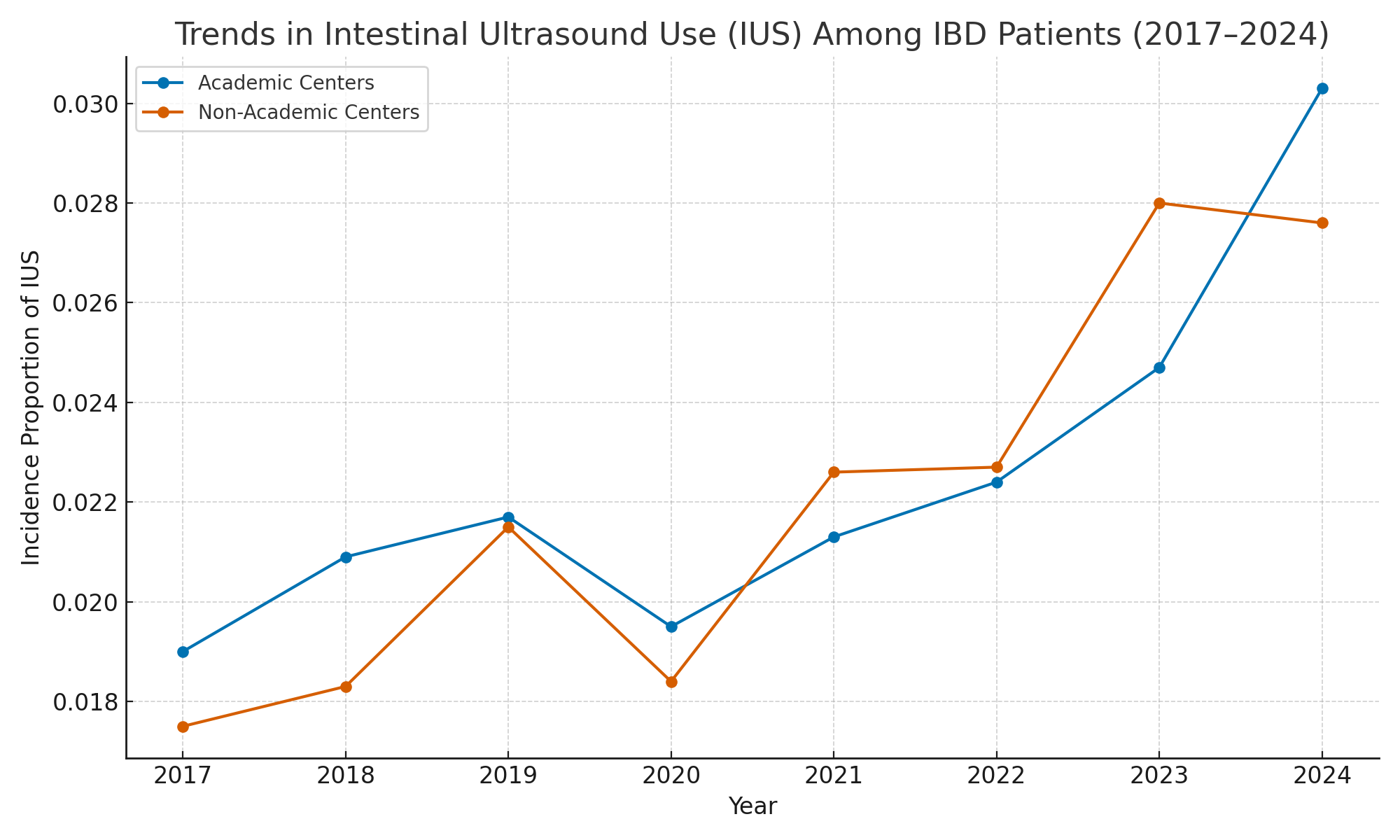
Figure: Figure 1: Trends of IUS untilization at Academic vs Non-academic centers
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Khyati Bidani indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Silpa Choday, MD2, Khyati Bidani, MD3, Indu Srinivasan, MD2, Wael Youssef, MD2. P3185 - Diverging Trajectories: Trends in Intestinal Ultrasound Utilization for IBD Across Academic and Non-Academic Institutions (2017–2024), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Intestinal ultrasound (IUS) has emerged as a valuable, non-invasive tool for real-time assessment of disease activity in patients with inflammatory bowel disease (IBD). While widely adopted in European clinical practice, IUS implementation in the United States has been slower and potentially uneven across healthcare settings. Academic centers, often at the forefront of adopting novel technologies, may integrate IUS more readily than non-academic institutions. Understanding this differential uptake is crucial to ensuring equitable access to advanced diagnostics. This study evaluates temporal trends in IUS utilization among IBD patients at academic vs non-academic centers in a large, multi-institutional real-world dataset.
Methods: We queried the TriNetX US Collaborative Network for adult IBD patients (ICD-10: K50, K51) between 2017 and 2024. IUS procedures were identified using CPT and ICD-10-PCS codes. The incidence proportion of IUS was calculated annually. Patients were stratified by institution type (academic vs. non-academic), age, sex, race, and ethnicity.
Results: Among 488,673 patients in academic centers and 196,051 in non-academic centers, IUS use increased in both groups over the 8 years. In academic centers, IUS incidence rose from 1.9% in 2017 to 3.03% in 2024, showing a steeper increase. In non-academic centers, the increase was slower, from 1.75% to 2.76%. Hispanic patients had the highest rise in IUS use in both settings, peaking at 4.26% (academic) vs 5.77% (non-academic) in 2024. Additionally, Female patients demonstrated slightly higher IUS use in both cohorts. Furthermore, Peak use occurred in the 30–59 age range, steadily increasing across all groups. Use was highest among Asian and White patients in academic centers; in non-academic centers, disparities were more evident with lower rates in Black patients.
Discussion: Over eight years, IUS utilization in IBD care has significantly increased across both academic and non-academic institutions, with academic centers demonstrating a more consistent rise. Disparities in adoption by institution type, race, ethnicity, and sex were evident, with Hispanic and female patients showing higher rates of IUS use. These findings underscore the growing integration of IUS into IBD care pathways but also highlight gaps in uniform access. Targeted dissemination strategies, broader provider education, and infrastructure support are needed to bridge these disparities and promote equitable adoption of IUS across all clinical settings.

Figure: Figure 2: Line graph showing the trends of IUS based on age, gender and ethinicity amongst academic centers
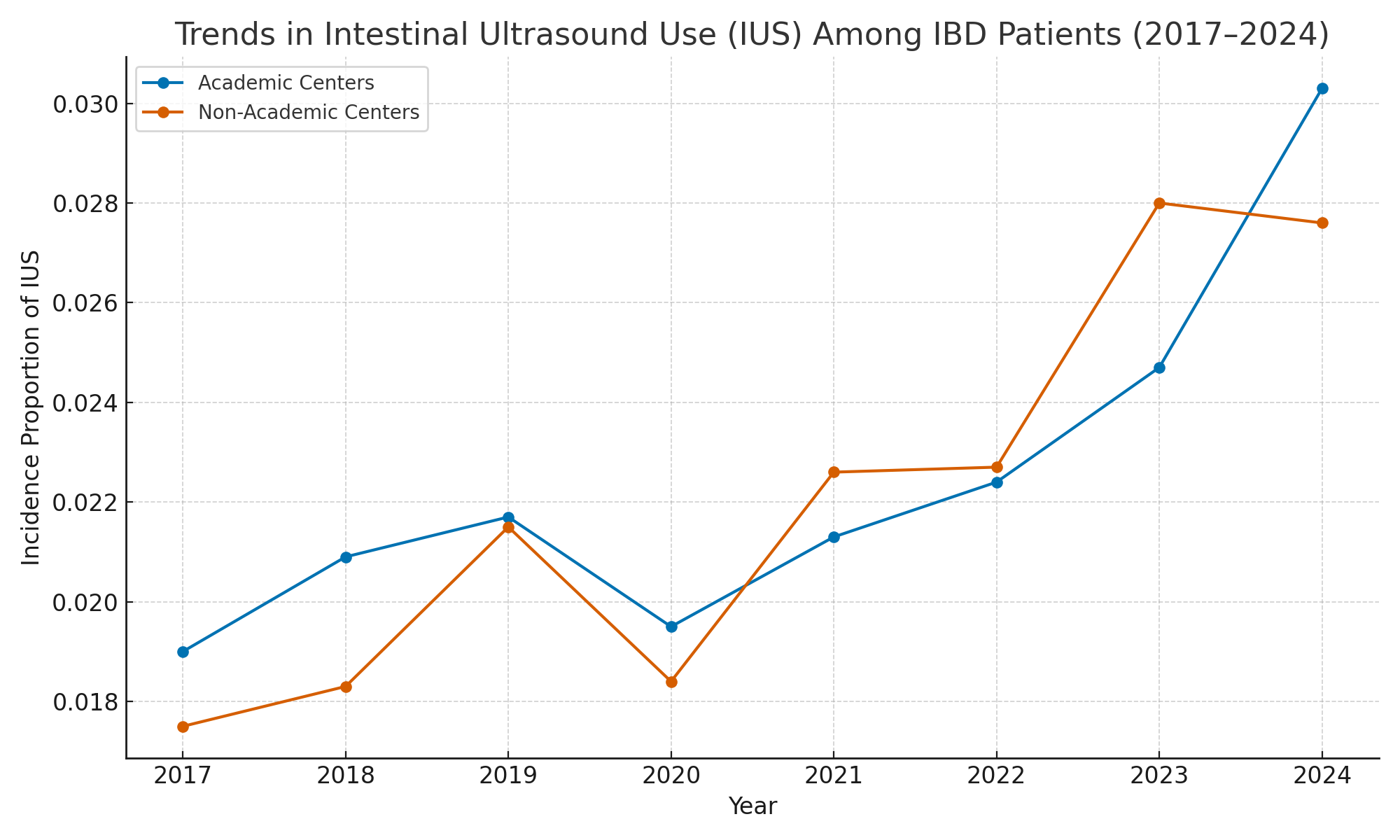
Figure: Figure 1: Trends of IUS untilization at Academic vs Non-academic centers
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Khyati Bidani indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Silpa Choday, MD2, Khyati Bidani, MD3, Indu Srinivasan, MD2, Wael Youssef, MD2. P3185 - Diverging Trajectories: Trends in Intestinal Ultrasound Utilization for IBD Across Academic and Non-Academic Institutions (2017–2024), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
