Monday Poster Session
Category: IBD
P3184 - Real-World Comparative Outcomes of Intestinal Ultrasound versus Colonoscopy in Monitoring Inflammatory Bowel Disease: A TriNetX-Based Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Ariana R. Tagliaferri, MD2, Pir Shah, MD3, Wael Youssef, MD2, Dalbir Sandhu, MD2, Indu Srinivasan, MD2, Divyesh Sejpal, MD, MS2
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3Creighton University Medical Center, Phoenix, AZ
Introduction: Intestinal ultrasound (IUS) is an emerging non-invasive tool for monitoring inflammatory bowel disease (IBD), but its comparative utility against colonoscopy in real-world clinical practice remains underexplored. This study aimed to evaluate clinical outcomes associated with IUS versus colonoscopy in patients with IBD.
Methods: Using the TriNetX US Collaborative Network, we identified adult patients (≥18 years) with Crohn’s disease or ulcerative colitis who underwent either IUS (Cohort 1) or colonoscopy (Cohort 2), excluding those who received both tests. Propensity score matching was performed 1:1 based on demographics, comorbidities, and baseline medications. Outcomes assessed over a 1-year period included corticosteroid use, biologic escalation, IBD flares, surgery, fistula, stricture/obstruction, and need for endoscopic reevaluation. Hazard ratios (HRs) were calculated using Kaplan-Meier survival analysis.
Results: After matching, 806 patients were included in each cohort. Patients in the IUS group had a significantly lower risk of biologic therapy escalation (HR 0.504; 95% CI: 0.363–0.702; p < 0.001) and experienced fewer IBD flares (HR 0.478; 95% CI: 0.301–0.757; p = 0.001) compared to those in the colonoscopy group. However, the IUS group showed a higher risk of corticosteroid use (HR 1.732; 95% CI: 1.178–2.547; p = 0.005) and obstruction or stricture (HR 2.083; 95% CI: 1.316–3.297; p = 0.001). No significant differences were observed between the two groups in rates of IBD-related surgery, fistula formation, or the need for repeat endoscopic evaluation.
Discussion: IUS was associated with fewer flares and reduced need for biologic escalation compared to colonoscopy, suggesting it may be a valuable alternative for routine IBD monitoring. These advantages may stem from IUS's ability to provide direct visualization of bowel wall inflammation and real-time feedback during clinical visits, allowing for earlier therapeutic adjustments. However, the higher incidence of corticosteroid use and stricturing events in the IUS group warrants further investigation. These findings support the expanded use of IUS in clinical practice, with careful patient selection and ongoing monitoring for potential complications.
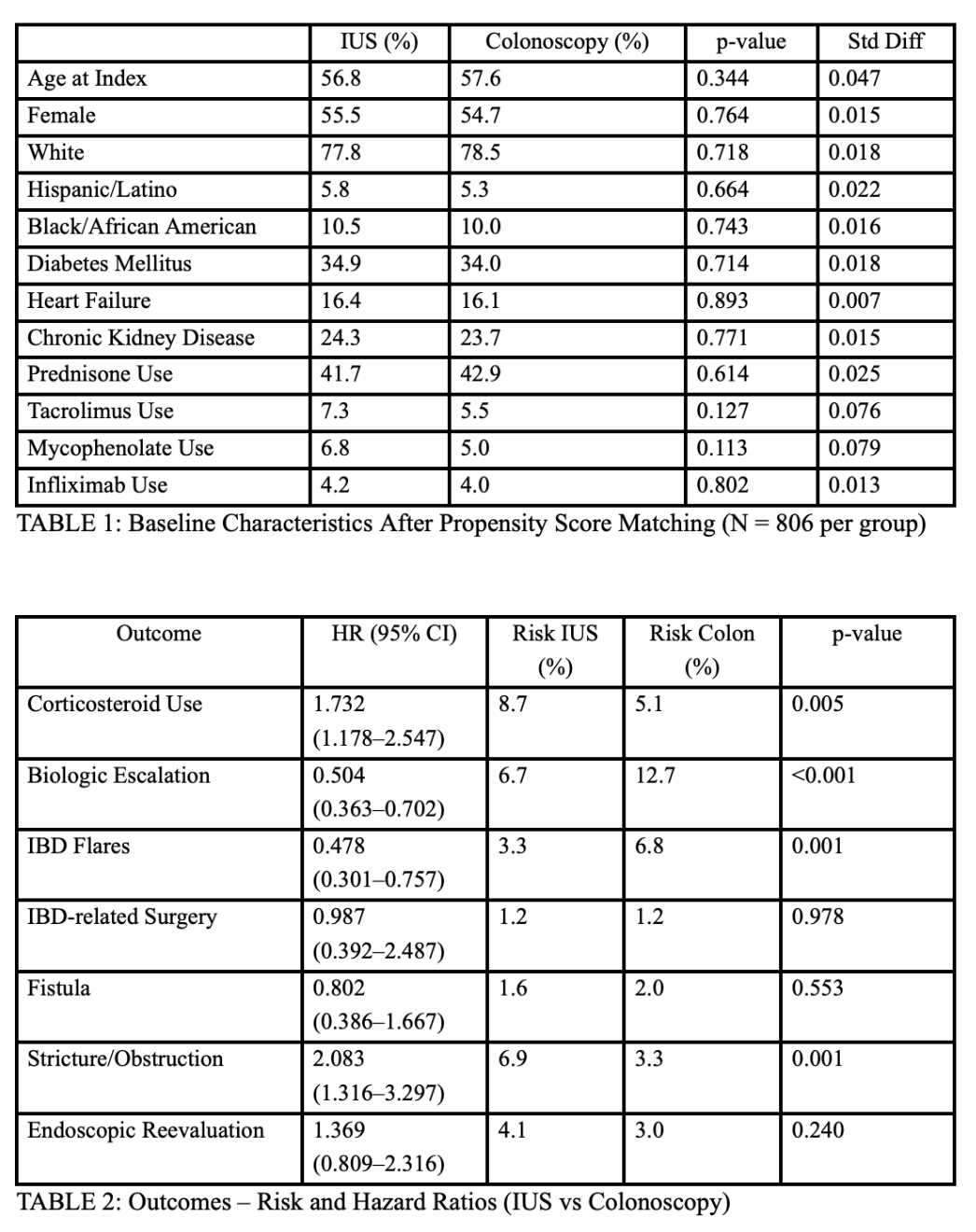
Figure: Hazard ratios comparing IBD outcomes in IUS vs colonoscopy patients
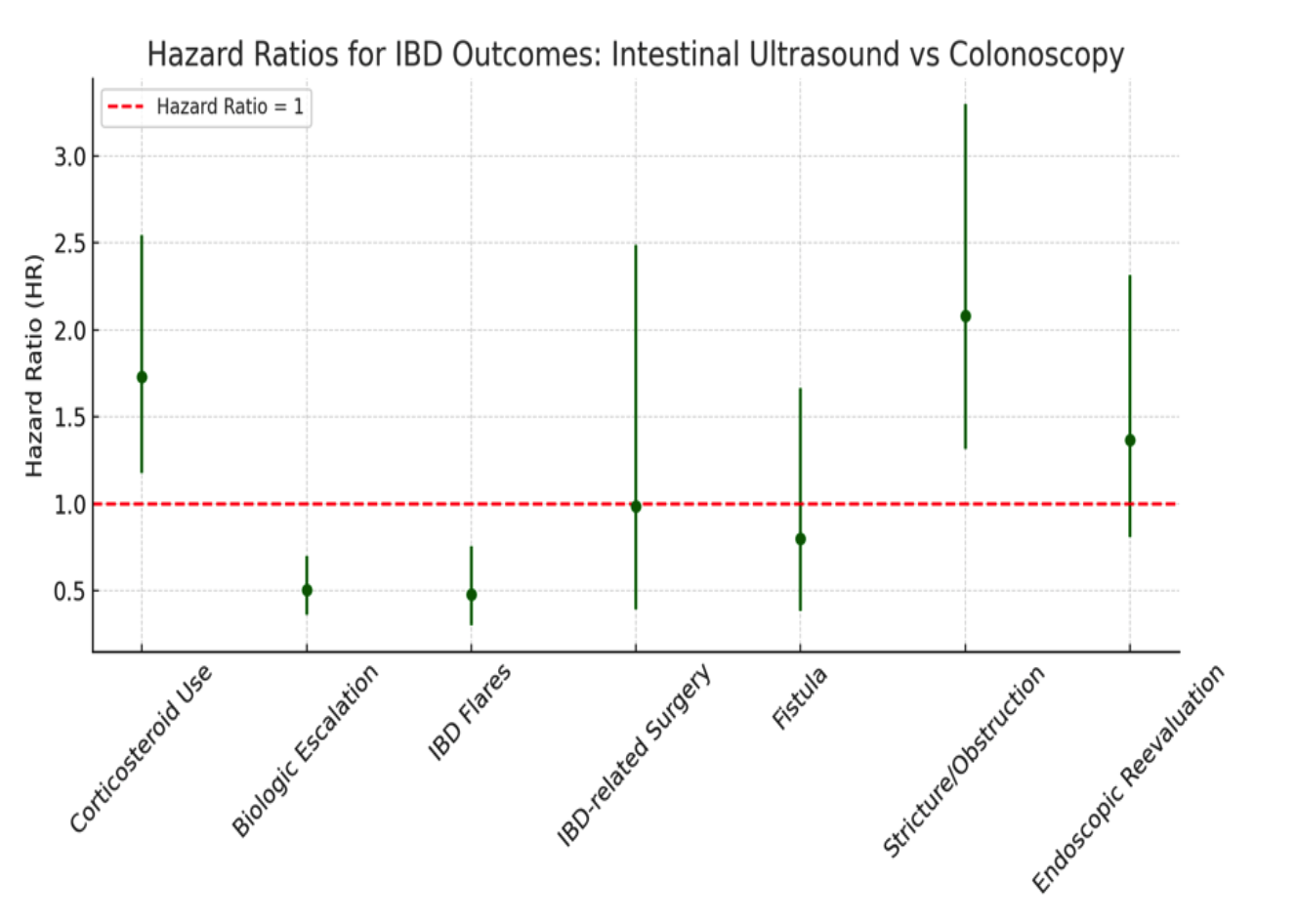
Figure: Table 1: Baseline Characteristics After Propensity Score Matching (N = 806 per group)
Table 2: Outcomes – Risk and Hazard Ratios (IUS vs Colonoscopy)
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Ariana Tagliaferri indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Divyesh Sejpal: Boston Scientific – Consultant. Olympus – Grant/Research Support.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Ariana R. Tagliaferri, MD2, Pir Shah, MD3, Wael Youssef, MD2, Dalbir Sandhu, MD2, Indu Srinivasan, MD2, Divyesh Sejpal, MD, MS2. P3184 - Real-World Comparative Outcomes of Intestinal Ultrasound versus Colonoscopy in Monitoring Inflammatory Bowel Disease: A TriNetX-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3Creighton University Medical Center, Phoenix, AZ
Introduction: Intestinal ultrasound (IUS) is an emerging non-invasive tool for monitoring inflammatory bowel disease (IBD), but its comparative utility against colonoscopy in real-world clinical practice remains underexplored. This study aimed to evaluate clinical outcomes associated with IUS versus colonoscopy in patients with IBD.
Methods: Using the TriNetX US Collaborative Network, we identified adult patients (≥18 years) with Crohn’s disease or ulcerative colitis who underwent either IUS (Cohort 1) or colonoscopy (Cohort 2), excluding those who received both tests. Propensity score matching was performed 1:1 based on demographics, comorbidities, and baseline medications. Outcomes assessed over a 1-year period included corticosteroid use, biologic escalation, IBD flares, surgery, fistula, stricture/obstruction, and need for endoscopic reevaluation. Hazard ratios (HRs) were calculated using Kaplan-Meier survival analysis.
Results: After matching, 806 patients were included in each cohort. Patients in the IUS group had a significantly lower risk of biologic therapy escalation (HR 0.504; 95% CI: 0.363–0.702; p < 0.001) and experienced fewer IBD flares (HR 0.478; 95% CI: 0.301–0.757; p = 0.001) compared to those in the colonoscopy group. However, the IUS group showed a higher risk of corticosteroid use (HR 1.732; 95% CI: 1.178–2.547; p = 0.005) and obstruction or stricture (HR 2.083; 95% CI: 1.316–3.297; p = 0.001). No significant differences were observed between the two groups in rates of IBD-related surgery, fistula formation, or the need for repeat endoscopic evaluation.
Discussion: IUS was associated with fewer flares and reduced need for biologic escalation compared to colonoscopy, suggesting it may be a valuable alternative for routine IBD monitoring. These advantages may stem from IUS's ability to provide direct visualization of bowel wall inflammation and real-time feedback during clinical visits, allowing for earlier therapeutic adjustments. However, the higher incidence of corticosteroid use and stricturing events in the IUS group warrants further investigation. These findings support the expanded use of IUS in clinical practice, with careful patient selection and ongoing monitoring for potential complications.
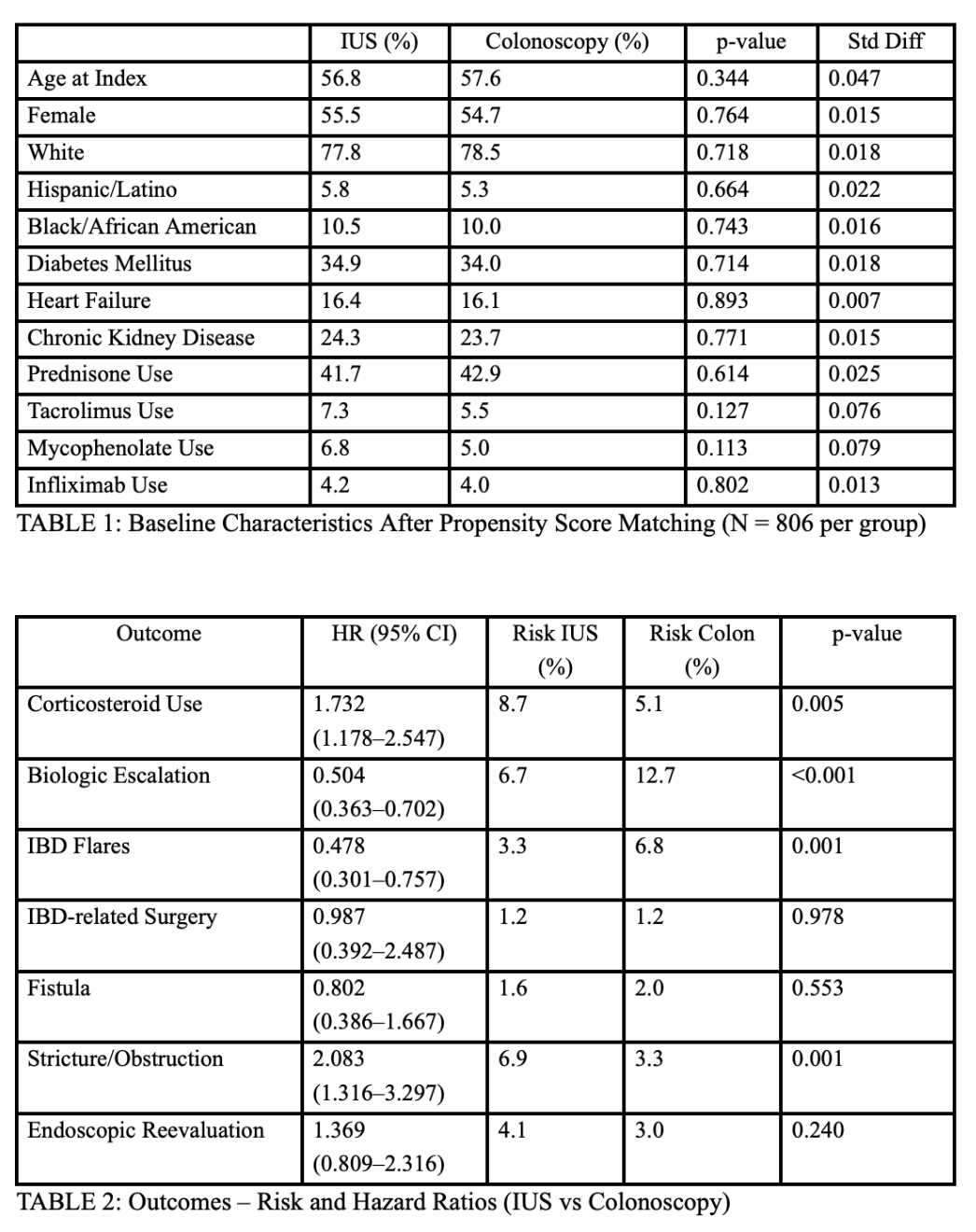
Figure: Hazard ratios comparing IBD outcomes in IUS vs colonoscopy patients
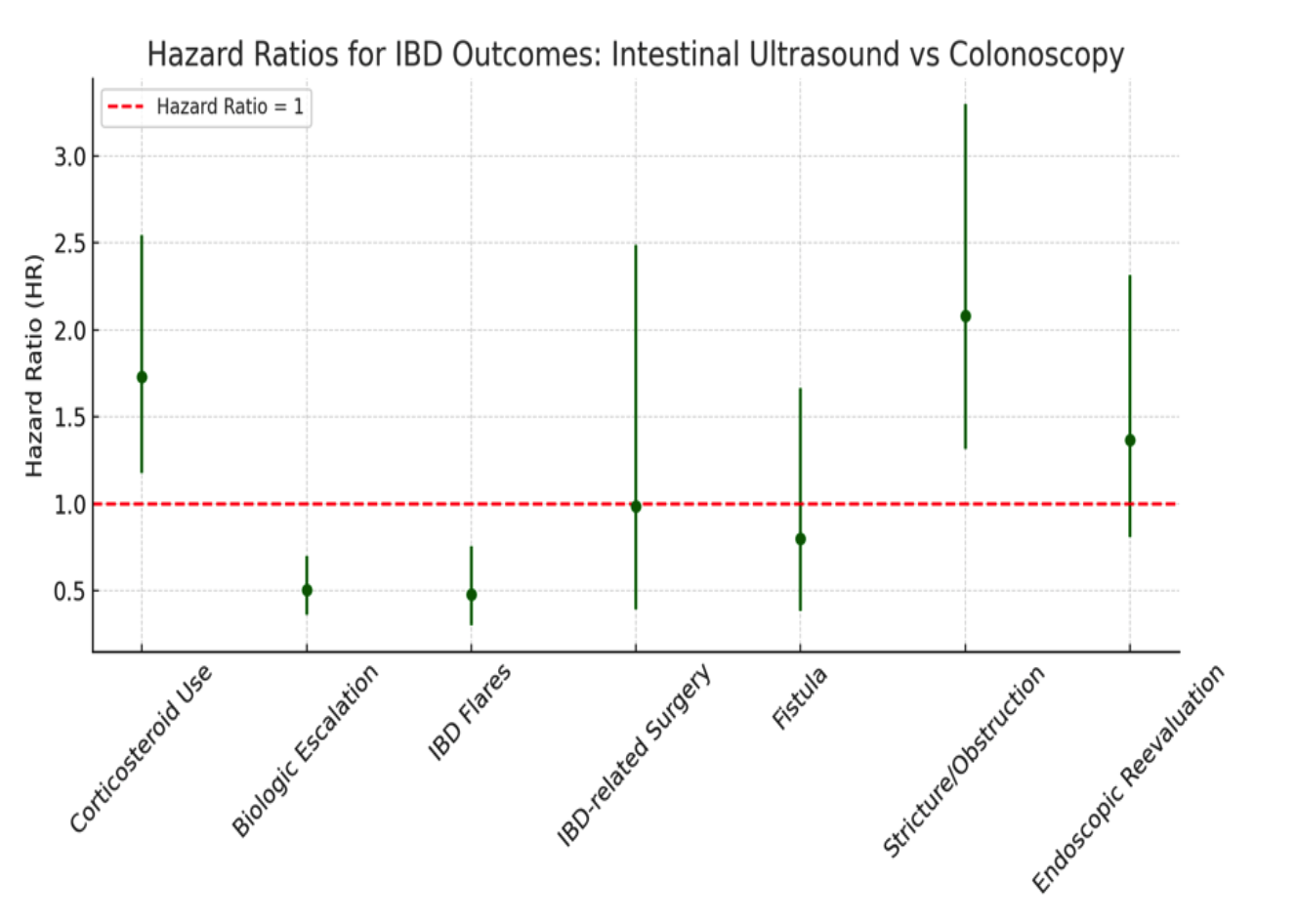
Figure: Table 1: Baseline Characteristics After Propensity Score Matching (N = 806 per group)
Table 2: Outcomes – Risk and Hazard Ratios (IUS vs Colonoscopy)
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Ariana Tagliaferri indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Divyesh Sejpal: Boston Scientific – Consultant. Olympus – Grant/Research Support.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Ariana R. Tagliaferri, MD2, Pir Shah, MD3, Wael Youssef, MD2, Dalbir Sandhu, MD2, Indu Srinivasan, MD2, Divyesh Sejpal, MD, MS2. P3184 - Real-World Comparative Outcomes of Intestinal Ultrasound versus Colonoscopy in Monitoring Inflammatory Bowel Disease: A TriNetX-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
