Monday Poster Session
Category: IBD
P3181 - Association Between Appendectomy and Ulcerative Colitis Risk: A Real-World, Propensity-Matched Analysis from a Multicenter Cohort
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Gautam Maddineni, MD2, Fnu Aakash, MD2, Osama Abdur Rehman, MD2, Silpa Choday, MD3, Sri Harsha Boppana, MBBS, MD4, Connor Mccaskey, MS5, Clive J. Miranda, DO, MSc6, Bhaumik Brahmbhatt, MBBS, MD7
1University of California Riverside School of Medicine, Riverside, CA; 2Florida State University, Cape Coral, FL; 3Creighton University School of Medicine, Phoenix, AZ; 4Nassau University Medical Center, East Meadow, NY; 5LECOM, Bradenton, FL; 6CHI Health Creighton University Medical Center, Omaha, NE; 7Mayo Clinic, Jacksonville, FL
Introduction: Ulcerative colitis (UC) is a chronic, immune-mediated inflammatory bowel disease (IBD) affecting the colon, with increasing prevalence worldwide. Although its pathogenesis remains incompletely understood, it is believed to result from a complex interplay of genetic, environmental, microbial, and immune factors. The role of the appendix in gut immunity and microbial homeostasis has led researchers to investigate whether appendectomy influences UC risk. While earlier studies suggested a potential protective association, results have varied, and robust evidence from large, diverse patient populations is lacking.
Methods: We performed a retrospective cohort study utilizing the TriNetX US Collaborative Network, a federated database of electronic medical records from 66 healthcare organizations. We identified adults (≥18 years) with a history of appendectomy (CPT codes: 1014622, 44950, 44960, 44970) and no prior diagnosis of IBD or pregnancy. These patients were compared to a control cohort with no history of appendectomy or IBD. Propensity score matching (1:1) was used to balance demographics and comorbidities, resulting in two cohorts of 266,715 patients each. The primary outcome was the incidence of UC, identified using ICD-10 codes following the index date. Statistical analyses included risk ratio calculations and Kaplan-Meier survival analysis.
Results: Post-matching, patients with prior appendectomy had a significantly lower risk of developing UC compared to the control group (4.4% vs. 5.7%; Risk Ratio 0.779; 95% CI: 0.760–0.798; p< 0.001). Kaplan-Meier analysis showed a modest but statistically significant improvement in UC-free survival in the appendectomy cohort (78.54% vs. 77.93%; HR 0.887, p< 0.001). Furthermore, among those who developed UC, patients in the appendectomy group had lower rates of corticosteroid use, biologic therapy escalation, and IBD-related surgeries, suggesting a milder disease course.
Discussion: In this large, real-world cohort study, prior appendectomy was associated with a statistically significant reduction in the risk of developing UC. These findings support the hypothesis that the appendix may play a role in immune regulation relevant to UC pathogenesis. While causality cannot be established, our results align with prior observational studies and underscore the need for mechanistic research into the immunologic and microbial consequences of appendectomy. Understanding these interactions may inform future strategies for UC risk prediction and prevention.

Figure: Table 1: Comparison of Patient Demographics and comorbid conditions in both cohorts with and without prior appendectomy
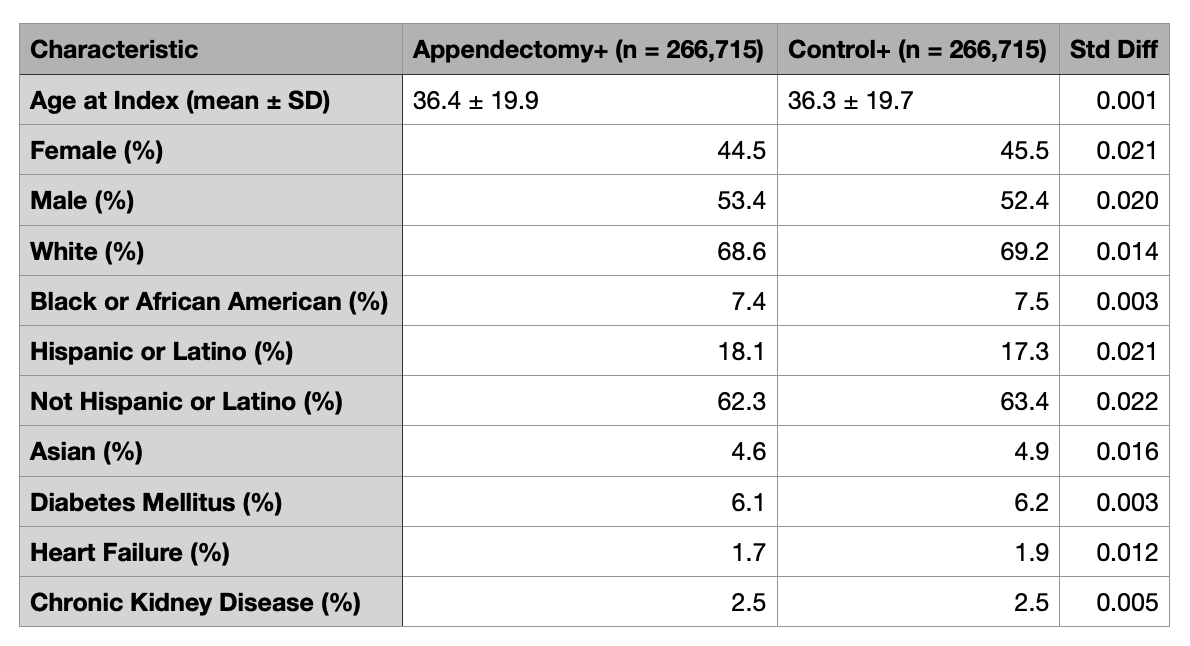
Figure: Figure 1: Outcomes tables with the risk ratio, odds ratio, and hazard ratios with confidence intervals and p-values. Images depicting a graphical representation of the outcomes.
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Connor Mccaskey indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Bhaumik Brahmbhatt indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Gautam Maddineni, MD2, Fnu Aakash, MD2, Osama Abdur Rehman, MD2, Silpa Choday, MD3, Sri Harsha Boppana, MBBS, MD4, Connor Mccaskey, MS5, Clive J. Miranda, DO, MSc6, Bhaumik Brahmbhatt, MBBS, MD7. P3181 - Association Between Appendectomy and Ulcerative Colitis Risk: A Real-World, Propensity-Matched Analysis from a Multicenter Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Florida State University, Cape Coral, FL; 3Creighton University School of Medicine, Phoenix, AZ; 4Nassau University Medical Center, East Meadow, NY; 5LECOM, Bradenton, FL; 6CHI Health Creighton University Medical Center, Omaha, NE; 7Mayo Clinic, Jacksonville, FL
Introduction: Ulcerative colitis (UC) is a chronic, immune-mediated inflammatory bowel disease (IBD) affecting the colon, with increasing prevalence worldwide. Although its pathogenesis remains incompletely understood, it is believed to result from a complex interplay of genetic, environmental, microbial, and immune factors. The role of the appendix in gut immunity and microbial homeostasis has led researchers to investigate whether appendectomy influences UC risk. While earlier studies suggested a potential protective association, results have varied, and robust evidence from large, diverse patient populations is lacking.
Methods: We performed a retrospective cohort study utilizing the TriNetX US Collaborative Network, a federated database of electronic medical records from 66 healthcare organizations. We identified adults (≥18 years) with a history of appendectomy (CPT codes: 1014622, 44950, 44960, 44970) and no prior diagnosis of IBD or pregnancy. These patients were compared to a control cohort with no history of appendectomy or IBD. Propensity score matching (1:1) was used to balance demographics and comorbidities, resulting in two cohorts of 266,715 patients each. The primary outcome was the incidence of UC, identified using ICD-10 codes following the index date. Statistical analyses included risk ratio calculations and Kaplan-Meier survival analysis.
Results: Post-matching, patients with prior appendectomy had a significantly lower risk of developing UC compared to the control group (4.4% vs. 5.7%; Risk Ratio 0.779; 95% CI: 0.760–0.798; p< 0.001). Kaplan-Meier analysis showed a modest but statistically significant improvement in UC-free survival in the appendectomy cohort (78.54% vs. 77.93%; HR 0.887, p< 0.001). Furthermore, among those who developed UC, patients in the appendectomy group had lower rates of corticosteroid use, biologic therapy escalation, and IBD-related surgeries, suggesting a milder disease course.
Discussion: In this large, real-world cohort study, prior appendectomy was associated with a statistically significant reduction in the risk of developing UC. These findings support the hypothesis that the appendix may play a role in immune regulation relevant to UC pathogenesis. While causality cannot be established, our results align with prior observational studies and underscore the need for mechanistic research into the immunologic and microbial consequences of appendectomy. Understanding these interactions may inform future strategies for UC risk prediction and prevention.

Figure: Table 1: Comparison of Patient Demographics and comorbid conditions in both cohorts with and without prior appendectomy
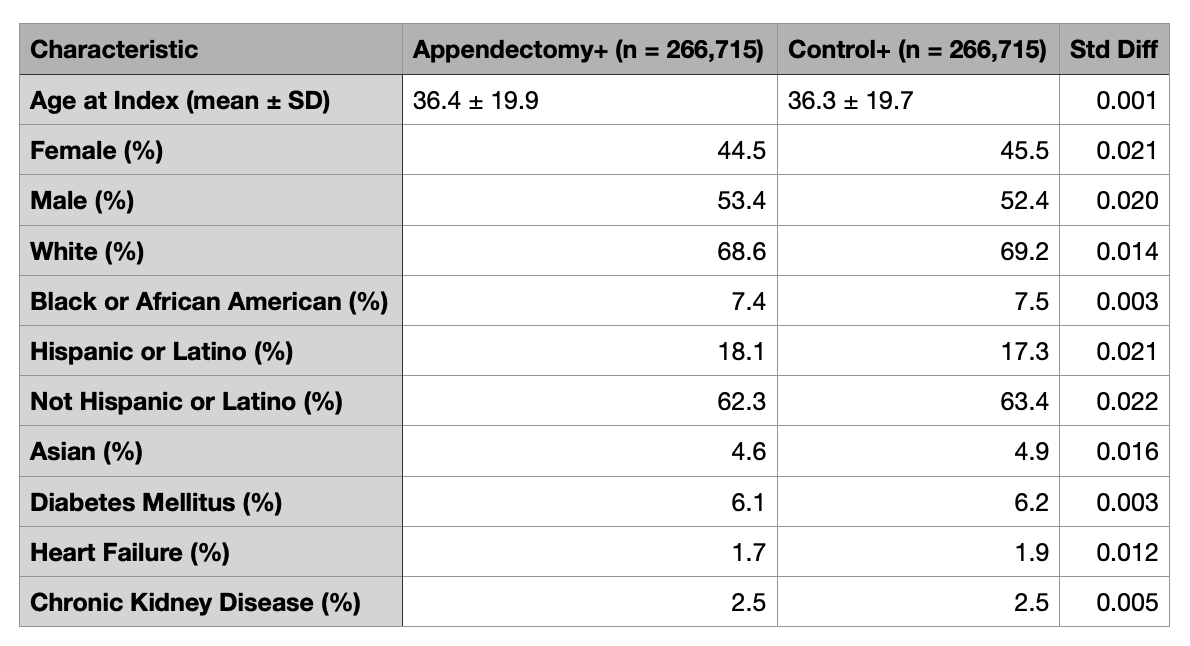
Figure: Figure 1: Outcomes tables with the risk ratio, odds ratio, and hazard ratios with confidence intervals and p-values. Images depicting a graphical representation of the outcomes.
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Fnu Aakash indicated no relevant financial relationships.
Osama Abdur Rehman indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Connor Mccaskey indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Bhaumik Brahmbhatt indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Gautam Maddineni, MD2, Fnu Aakash, MD2, Osama Abdur Rehman, MD2, Silpa Choday, MD3, Sri Harsha Boppana, MBBS, MD4, Connor Mccaskey, MS5, Clive J. Miranda, DO, MSc6, Bhaumik Brahmbhatt, MBBS, MD7. P3181 - Association Between Appendectomy and Ulcerative Colitis Risk: A Real-World, Propensity-Matched Analysis from a Multicenter Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
