Monday Poster Session
Category: IBD
P3179 - Conjugal Inflammatory Bowel Disease: A Case Series
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JC
Justin Chuang, MD
Mather Hospital, Northwell Health
Port Jefferson, NY
Presenting Author(s)
Justin Chuang, MD, Toby Bradford, MD, Monica Arora, DO, Lindsey Donnelly, MD, Ramona Rajapakse, MD, FACG
Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Cohabitation may play a significant role in inflammatory bowel disease (IBD) pathogenesis and disease progression in unaffected spouses. Prior studies have demonstrated an increase frequency of new IBD in previously unaffected individuals after marriage to a patient with IBD. It’s unclear what factors of cohabitation may contribute to IBD pathogenesis. We evaluated couples with IBD in an effort to better characterize conjugal IBD.
Methods: We examined adult patients at a single-center academic outpatient setting with biopsy confirmed IBD in both spouses from 2018 to 2025. IBD diagnosis was confirmed by chart review and patient confirmation. Observed and expected frequencies were calculated using Pearson’s chi square analysis. Institutional review board approval was obtained prior to study initiation.
Results: We identified 6 patients (3 couples) with conjugal IBD. Most patients were on biologic therapy (66%), in clinical remission (66%), without prior IBD related surgery (83%), and without extraintestinal manifestations (100%). There was no family history or clinical symptoms of IBD in the initially unaffected partners. The IBD diagnosis was concordant in 66% (Crohn’s) of cases. All cases were diagnosed after cohabitation. The average length of cohabitation was 34 years. The time to conjugal IBD diagnosis was 49 years and 19 years for Crohn’s disease and ulcerative colitis, respectively. Couples with a longer duration of cohabitation prior to conjugal IBD diagnosis were less likely to be in endoscopic remission. The relationship between duration of cohabitation prior to conjugal IBD diagnosis and endoscopic remission was statistically significant (Pearson X2(2) = 6, p = 0.050).
Discussion: In this case series, conjugal IBD was most often concordant and occurred decades after cohabitation in partners without any obvious risk factors for IBD. Additionally, couples with longer durations of cohabitation were less likely to be in endoscopic remission. Prior studies have demonstrated that cohabitation may enable dysbiosis of the microbiome accelerating IBD pathogenies in susceptible individuals. Additional prospective studies are warranted to better characterize the various factors associated with conjugal IBD.
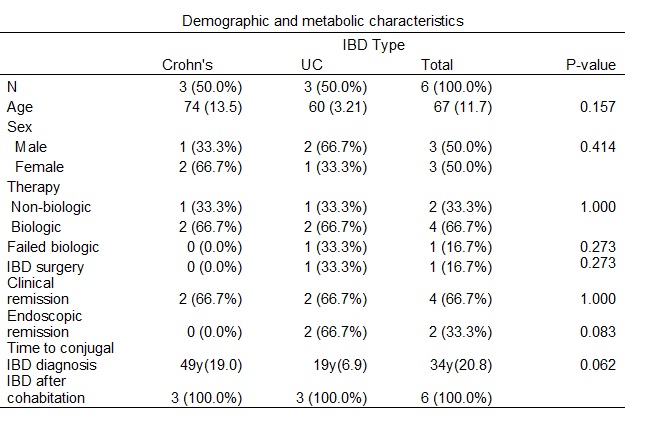
Figure: Table 1: Demographic and metabolic characteristics
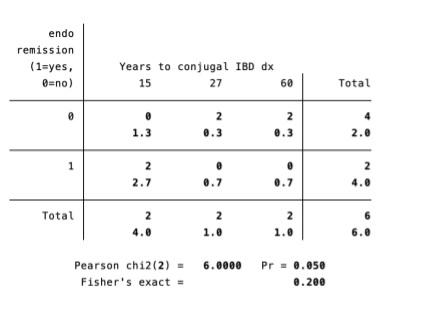
Figure: The relationship between duration of cohabitation prior to conjugal IBD diagnosis and endoscopic remission was statistically significant (Pearson X2(2) = 6, p = 0.050).
Disclosures:
Justin Chuang indicated no relevant financial relationships.
Toby Bradford indicated no relevant financial relationships.
Monica Arora indicated no relevant financial relationships.
Lindsey Donnelly indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Justin Chuang, MD, Toby Bradford, MD, Monica Arora, DO, Lindsey Donnelly, MD, Ramona Rajapakse, MD, FACG. P3179 - Conjugal Inflammatory Bowel Disease: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mather Hospital, Northwell Health, Port Jefferson, NY
Introduction: Cohabitation may play a significant role in inflammatory bowel disease (IBD) pathogenesis and disease progression in unaffected spouses. Prior studies have demonstrated an increase frequency of new IBD in previously unaffected individuals after marriage to a patient with IBD. It’s unclear what factors of cohabitation may contribute to IBD pathogenesis. We evaluated couples with IBD in an effort to better characterize conjugal IBD.
Methods: We examined adult patients at a single-center academic outpatient setting with biopsy confirmed IBD in both spouses from 2018 to 2025. IBD diagnosis was confirmed by chart review and patient confirmation. Observed and expected frequencies were calculated using Pearson’s chi square analysis. Institutional review board approval was obtained prior to study initiation.
Results: We identified 6 patients (3 couples) with conjugal IBD. Most patients were on biologic therapy (66%), in clinical remission (66%), without prior IBD related surgery (83%), and without extraintestinal manifestations (100%). There was no family history or clinical symptoms of IBD in the initially unaffected partners. The IBD diagnosis was concordant in 66% (Crohn’s) of cases. All cases were diagnosed after cohabitation. The average length of cohabitation was 34 years. The time to conjugal IBD diagnosis was 49 years and 19 years for Crohn’s disease and ulcerative colitis, respectively. Couples with a longer duration of cohabitation prior to conjugal IBD diagnosis were less likely to be in endoscopic remission. The relationship between duration of cohabitation prior to conjugal IBD diagnosis and endoscopic remission was statistically significant (Pearson X2(2) = 6, p = 0.050).
Discussion: In this case series, conjugal IBD was most often concordant and occurred decades after cohabitation in partners without any obvious risk factors for IBD. Additionally, couples with longer durations of cohabitation were less likely to be in endoscopic remission. Prior studies have demonstrated that cohabitation may enable dysbiosis of the microbiome accelerating IBD pathogenies in susceptible individuals. Additional prospective studies are warranted to better characterize the various factors associated with conjugal IBD.
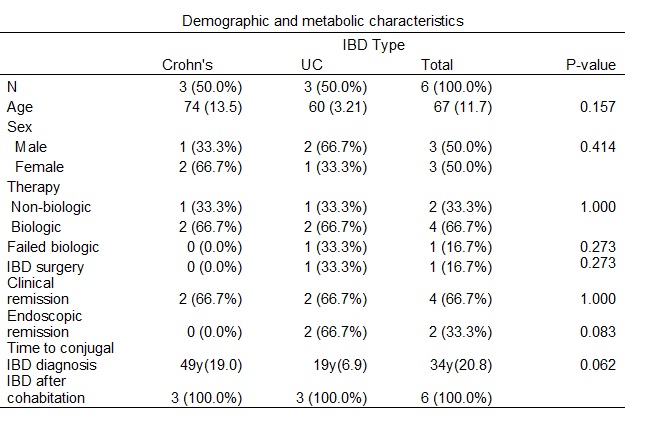
Figure: Table 1: Demographic and metabolic characteristics
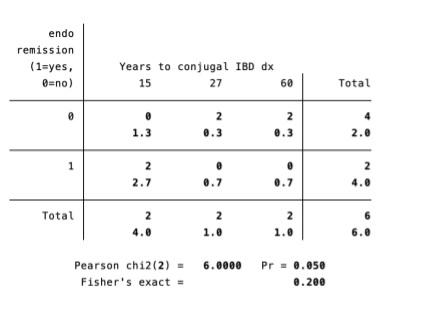
Figure: The relationship between duration of cohabitation prior to conjugal IBD diagnosis and endoscopic remission was statistically significant (Pearson X2(2) = 6, p = 0.050).
Disclosures:
Justin Chuang indicated no relevant financial relationships.
Toby Bradford indicated no relevant financial relationships.
Monica Arora indicated no relevant financial relationships.
Lindsey Donnelly indicated no relevant financial relationships.
Ramona Rajapakse indicated no relevant financial relationships.
Justin Chuang, MD, Toby Bradford, MD, Monica Arora, DO, Lindsey Donnelly, MD, Ramona Rajapakse, MD, FACG. P3179 - Conjugal Inflammatory Bowel Disease: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
