Monday Poster Session
Category: IBD
P3162 - Gastroenterologist Follow-Up Is Associated With Reduced Readmission Compared to Primary Care After Hospitalization for Severe Ulcerative Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GB
Grant Barber, MD, MS
Stanford Health Care
Stanford, CA
Presenting Author(s)
Ola Selnes, BSc1, Justin Zhuo, MD2, Sarah Streett, MD1, Grant Barber, MD, MS1
1Stanford Health Care, Stanford, CA; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Patients hospitalized for severe ulcerative colitis (UC) flares are at high risk of readmission, yet guidelines offer limited direction for post-discharge care. Prior studies suggest timely outpatient follow-up with a gastroenterology (GI) specialist may reduce readmission risk, but the impact of provider type remains unclear. We aimed to determine whether post-discharge follow-up with a primary care provider (PCP) influences readmission risk.
Methods: We conducted a retrospective cohort study of patients hospitalized for UC flare at Stanford University Hospital between 2010 and 2021. The primary outcome was time to a GI-related readmission. The primary exposure was provider type at first follow-up visit (GI vs PCP vs no follow-up), modeled as a time-dependent covariate in Cox proportional hazards regression. Models were adjusted for age, sex, and albumin at admission. Kaplan-Meier and log-rank tests compared cumulative readmission risk between PCP follow-up and no follow-up.
Results: Of the 223 patients included for analysis, 156 (70.0%) had follow-up with a GI specialist, 28 (12.3%) had PCP follow-up, and 39 (17.4%) had no follow-up during the study period. Median time to follow-up was shorter in the PCP group (5 days, IQR 6 days) than in the GI specialist group (10 days, IQR 14 days). PCP follow-up was not associated with reduced readmission compared to no follow-up (adjusted HR 1.40; 95%-CI, 0.63-3.15; p=0.41). Follow-up with a GI specialist was associated with a significantly lower readmission risk (adjusted HR 0.46; 95%-CI, 0.24-0.87; p=0.016).
Discussion: Our results highlight the importance of provider type in post-discharge care after hospitalization for severe UC. Despite earlier follow-up, PCP evaluation did not reduce readmissions, while follow-up with a GI specialist was significantly associated with reduced readmission rates. This suggests that GI-specific care in the post-discharge phase is important for recognizing early relapse, optimizing therapies, and preventing readmissions. Thus, ensuring access to GI should be prioritized in care pathways for post-discharge UC management. To further elucidate this, future studies should evaluate whether follow-up with GI-specific advanced practice providers confers a similar reduction of readmissions.
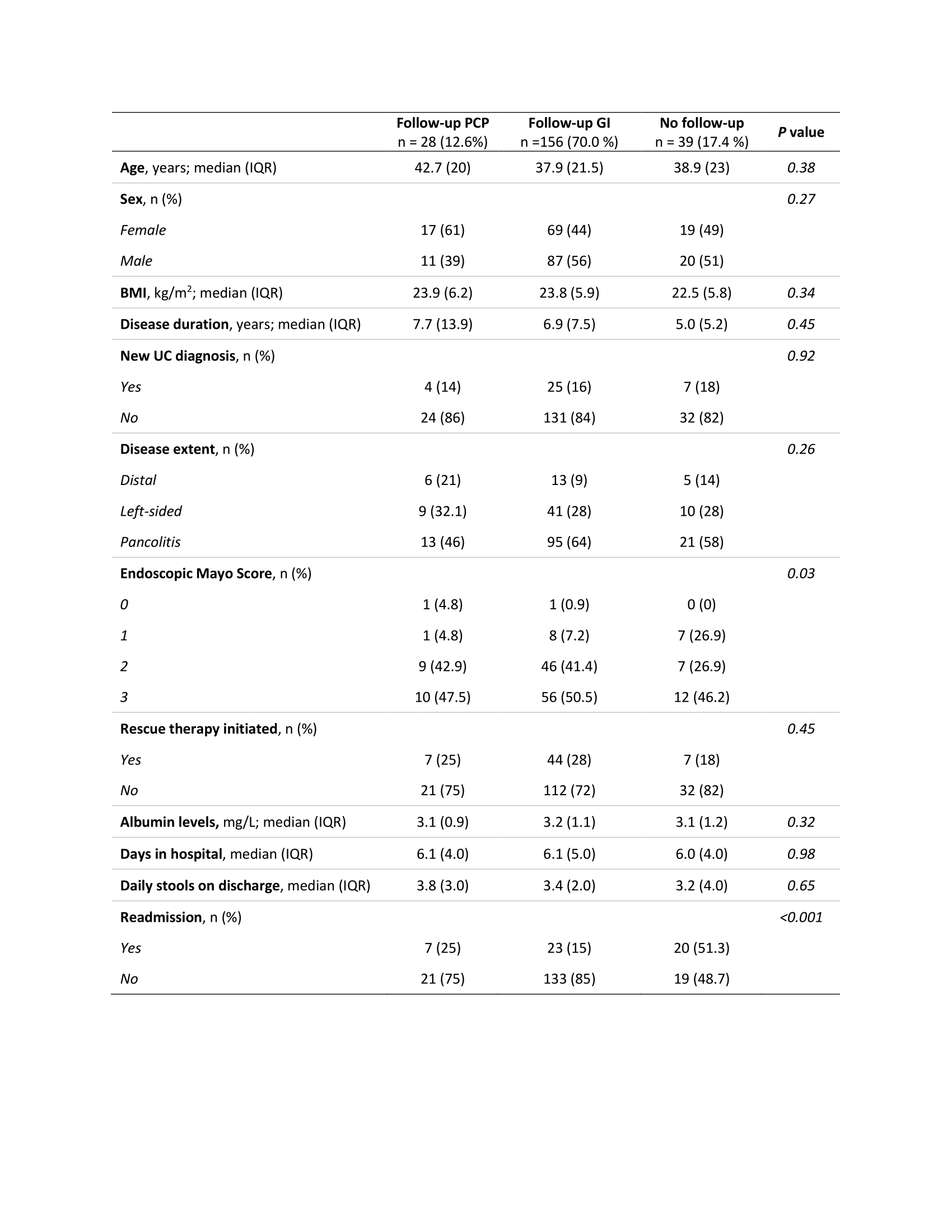
Figure: Table 1. Characteristics of study participants stratified by follow-up with PCP, GI specialist, or no follow-up.
Abbreviations: BMI, body mass index; UC, ulcerative colitis.
P values are generated by chi-squared-test and Fisher’s exact test (if <5 observation in ≥1 cell for a variable) for categorical variables, and ANOVA for continuous variables.
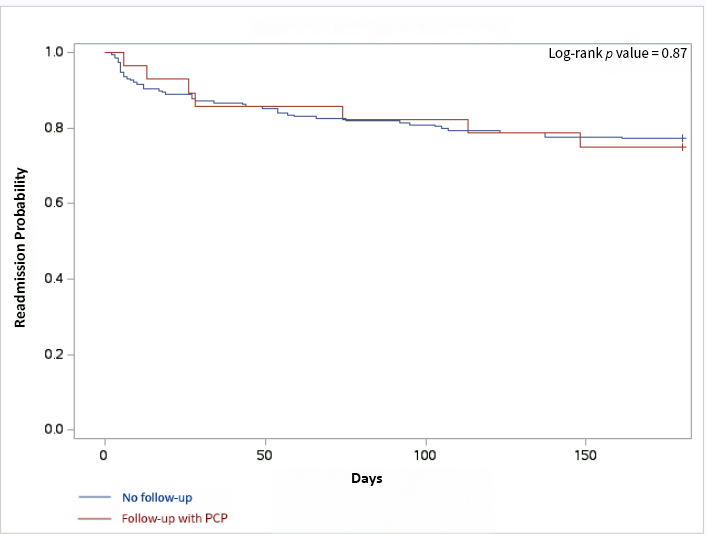
Figure: Figure 1. Kaplan-Meyer curve. Readmission probability following 180 days after discharge with PCP follow-up versus no follow-up.
Disclosures:
Ola Selnes indicated no relevant financial relationships.
Justin Zhuo indicated no relevant financial relationships.
Sarah Streett: Bristol Myers Squibb – Advisory Committee/Board Member. Direct Biologics – Advisory Committee/Board Member. gilead – Consultant. janssen – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member.
Grant Barber indicated no relevant financial relationships.
Ola Selnes, BSc1, Justin Zhuo, MD2, Sarah Streett, MD1, Grant Barber, MD, MS1. P3162 - Gastroenterologist Follow-Up Is Associated With Reduced Readmission Compared to Primary Care After Hospitalization for Severe Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Stanford Health Care, Stanford, CA; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Patients hospitalized for severe ulcerative colitis (UC) flares are at high risk of readmission, yet guidelines offer limited direction for post-discharge care. Prior studies suggest timely outpatient follow-up with a gastroenterology (GI) specialist may reduce readmission risk, but the impact of provider type remains unclear. We aimed to determine whether post-discharge follow-up with a primary care provider (PCP) influences readmission risk.
Methods: We conducted a retrospective cohort study of patients hospitalized for UC flare at Stanford University Hospital between 2010 and 2021. The primary outcome was time to a GI-related readmission. The primary exposure was provider type at first follow-up visit (GI vs PCP vs no follow-up), modeled as a time-dependent covariate in Cox proportional hazards regression. Models were adjusted for age, sex, and albumin at admission. Kaplan-Meier and log-rank tests compared cumulative readmission risk between PCP follow-up and no follow-up.
Results: Of the 223 patients included for analysis, 156 (70.0%) had follow-up with a GI specialist, 28 (12.3%) had PCP follow-up, and 39 (17.4%) had no follow-up during the study period. Median time to follow-up was shorter in the PCP group (5 days, IQR 6 days) than in the GI specialist group (10 days, IQR 14 days). PCP follow-up was not associated with reduced readmission compared to no follow-up (adjusted HR 1.40; 95%-CI, 0.63-3.15; p=0.41). Follow-up with a GI specialist was associated with a significantly lower readmission risk (adjusted HR 0.46; 95%-CI, 0.24-0.87; p=0.016).
Discussion: Our results highlight the importance of provider type in post-discharge care after hospitalization for severe UC. Despite earlier follow-up, PCP evaluation did not reduce readmissions, while follow-up with a GI specialist was significantly associated with reduced readmission rates. This suggests that GI-specific care in the post-discharge phase is important for recognizing early relapse, optimizing therapies, and preventing readmissions. Thus, ensuring access to GI should be prioritized in care pathways for post-discharge UC management. To further elucidate this, future studies should evaluate whether follow-up with GI-specific advanced practice providers confers a similar reduction of readmissions.
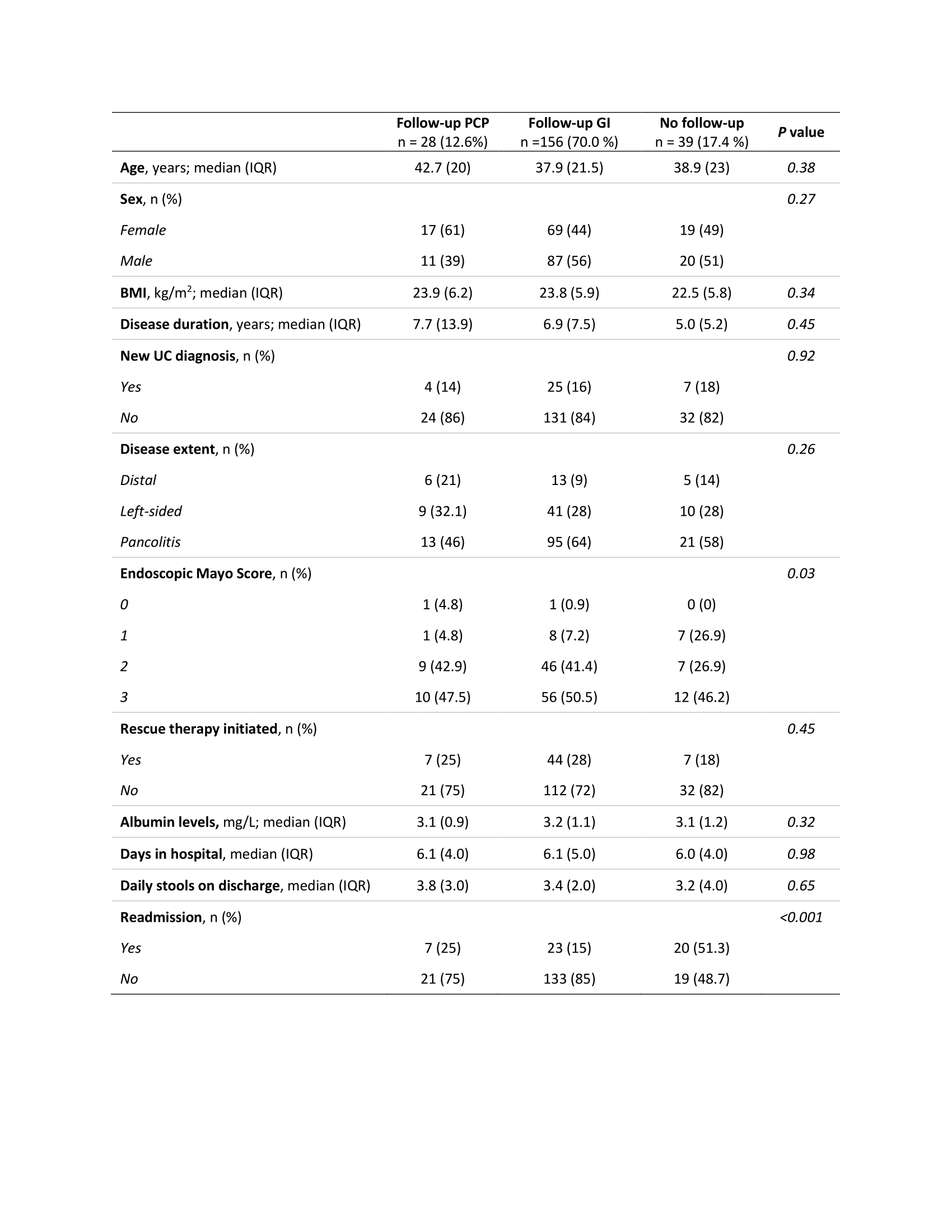
Figure: Table 1. Characteristics of study participants stratified by follow-up with PCP, GI specialist, or no follow-up.
Abbreviations: BMI, body mass index; UC, ulcerative colitis.
P values are generated by chi-squared-test and Fisher’s exact test (if <5 observation in ≥1 cell for a variable) for categorical variables, and ANOVA for continuous variables.
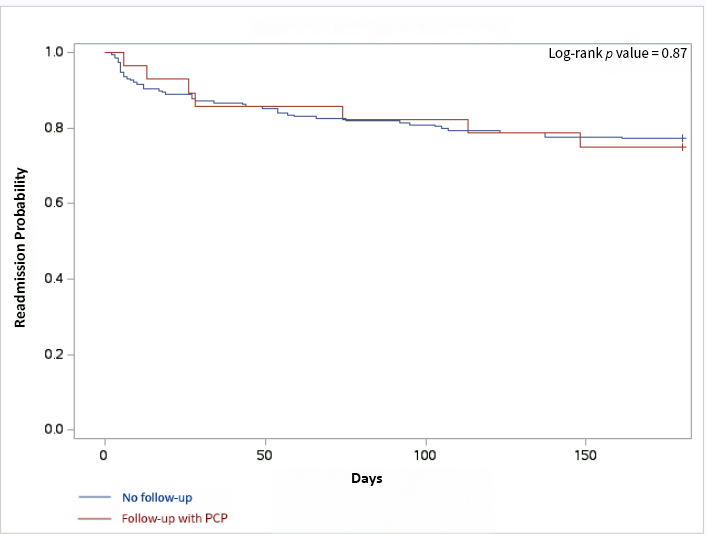
Figure: Figure 1. Kaplan-Meyer curve. Readmission probability following 180 days after discharge with PCP follow-up versus no follow-up.
Disclosures:
Ola Selnes indicated no relevant financial relationships.
Justin Zhuo indicated no relevant financial relationships.
Sarah Streett: Bristol Myers Squibb – Advisory Committee/Board Member. Direct Biologics – Advisory Committee/Board Member. gilead – Consultant. janssen – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member.
Grant Barber indicated no relevant financial relationships.
Ola Selnes, BSc1, Justin Zhuo, MD2, Sarah Streett, MD1, Grant Barber, MD, MS1. P3162 - Gastroenterologist Follow-Up Is Associated With Reduced Readmission Compared to Primary Care After Hospitalization for Severe Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
