Monday Poster Session
Category: IBD
P3157 - Cardiovascular Risk Factors Drive Mortality in Patients With Inflammatory Bowel Disease - A Propensity-Matched US National Database Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Preetika Sinh, MD
University of California San Diego
San Diego, CA
Presenting Author(s)
Paraj Patel, MD1, Omar Iqbal, MD1, Divyanshu Mohananey, MD1, Saffia Bajwa, DO1, Masoud Khani, MS1, Jake Lou, PhD2, Daniel J. Stein, MD3, Jana G. Hashash, MD, MSc, FACG4, Emad Mansoor, MD5, Raymond K. Cross, MD, MS, FACG6, Gursimran Kochhar, MD7, Preetika Sinh, MD8
1Medical College of Wisconsin, Milwaukee, WI; 2University of Wisconsin, Milwaukee, WI; 3Medical College of Wisconsin, Wauwatosa, WI; 4Mayo Clinic, Jacksonville, FL; 5University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 6The Melissa L. Posner Institute for Digestive Health & Liver Disease, Mercy Medical Center, Baltimore, MD; 7Allegheny Health Network, Pittsburgh, PA; 8University of California San Diego, San Diego, CA
Introduction: Inflammatory bowel disease (IBD) is associated with an increased risk of adverse cardiovascular (CV) events and venous thromboembolism (VTE), though its impact on mortality remains debatable. The ORAL Surveillance study [NEJM 2022] found that tofacitinib, a Janus kinase inhibitor approved for ulcerative colitis (UC), was linked to increased mortality in rheumatoid arthritis patients, particularly those with CV risk factors (RFs) [Ann Rheum 2023]. We aimed to determine all-cause mortality in IBD patients and assess the role of CV and VTE RFs.
Methods: We performed a retrospective cohort study using multi-institutional database TriNetX. IBD patients [UC and Crohn’s Disease (CD)] were identified between 2015 to 2023 with the presence of LOINC codes for IBD medications (to increase the validity of diagnosis codes). Data was collected for demographics, IBD medications, CV RFs, VTE RFs and history of coronary artery disease (CAD). We compared IBD patients to 1:1 propensity score matched non IBD controls for age, gender, race, and ethnicity for outcome of all-cause mortality [specific CV mortality data is not validated in TriNetx]. Patients with other chronic inflammatory disorders, celiac disease, and malignancy were excluded. All outcomes were assessed after the IBD index date. Odds Ratios (OR) was used to assess association between IBD and mortality. Logistic regression was used to evaluate the impact of individual RFs in the IBD cohort.
Results: We identified 110,116 IBD patients (49% UC, 51% CD) and propensity matched non-IBD controls. Even though, IBD patients had a higher prevalence of CV RFs, VTE RFs, and CAD [Table 1] IBD was associated with overall lower all-cause mortality compared to controls (OR 0.89, 95% CI 0.85–0.91, p < 0.001) [Table 2]. On further analysis of the IBD cohort with logistic regression, IBD patients with CV RFs, especially CAD had increased mortality as compared to IBD patients without CV RFs (IBD only OR 0.88, 95% CI 0.84–0.91 vs. IBD + CAD OR 4.41, 95% CI 4.18–4.65). Prior VTE was not associated with increased mortality.
Discussion: IBD patients have lower all-cause mortality compared to matched non-IBD controls. However, the presence of CV RFs—particularly CAD—significantly increases mortality risk. Identifying and managing CV comorbidities in IBD patients is essential to improving long-term outcomes.
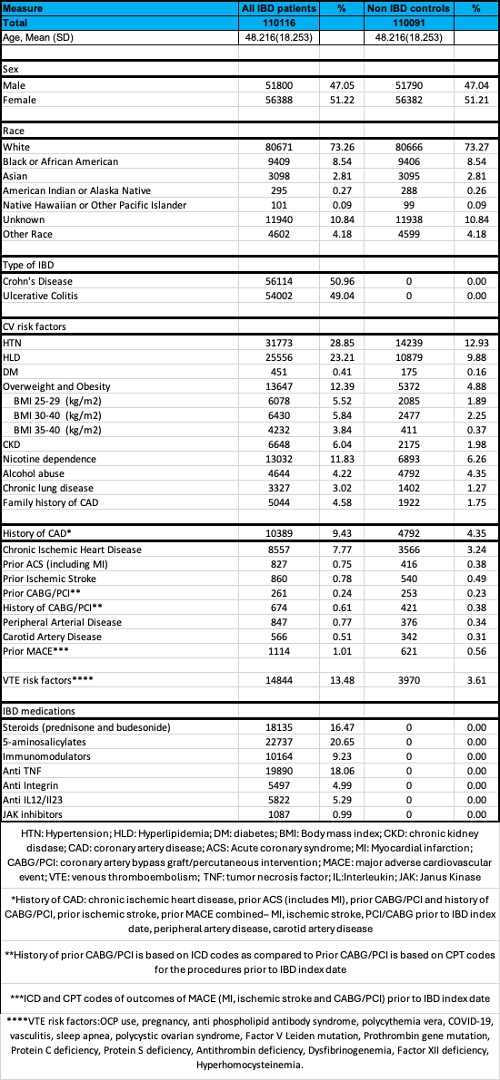
Figure: Table 1: DEMOGRAPHICS AND RISK FACTORS OF INFLAMMATORY BOWEL DISEASE PATIENTS AND CONTROLS
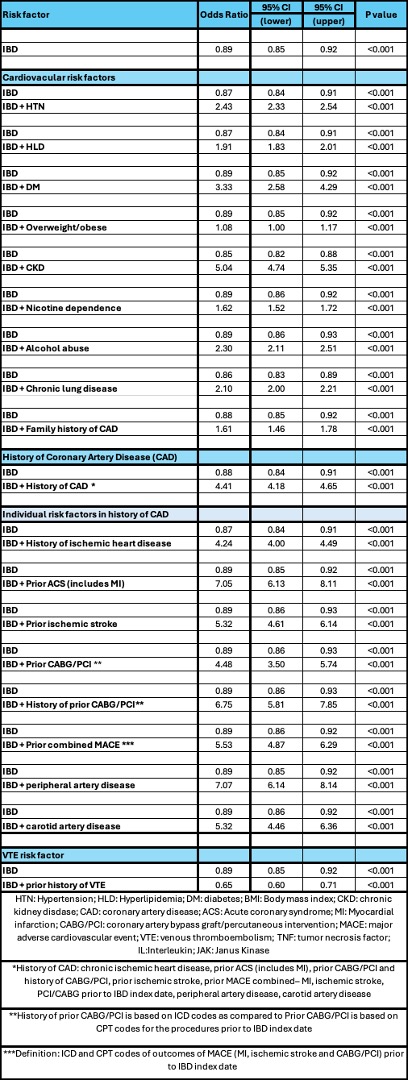
Figure: Table 2: ALL CAUSE MORTALITY IN PATIENTS WITH INFLAMMATORY BOWEL DISEASE (IBD), WITH AND WITHOUT CARDIOVASCULAR RISK FACTORS.
Disclosures:
Paraj Patel indicated no relevant financial relationships.
Omar Iqbal indicated no relevant financial relationships.
Divyanshu Mohananey indicated no relevant financial relationships.
Saffia Bajwa indicated no relevant financial relationships.
Masoud Khani indicated no relevant financial relationships.
Jake Lou indicated no relevant financial relationships.
Daniel Stein: Abbvie – Advisory Committee/Board Member. Abbvie – Speakers Bureau. BMS – Speakers Bureau. Lilly – Speakers Bureau.
Jana Hashash: BMS – Ad Board.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Raymond K. Cross: Abbvie – Advisor or Review Panel Member, Consultant, Speakers Bureau. BMS – Advisor or Review Panel Member, Consultant, Speakers Bureau. CorEvitas – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member, Consultant. Genetech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. IBD Education Group – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Advisory Committee/Board Member, Consultant. Option Care – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pharmacosmos – Advisory Committee/Board Member, Consultant. Samsung Bioepis – Advisory Committee/Board Member, Consultant. Sandoz – Advisory Committee/Board Member, Consultant. Takeda – Grant/Research Support.
Gursimran Kochhar indicated no relevant financial relationships.
Preetika Sinh: Advisory board BMS – Advisor or Review Panel Member.
Paraj Patel, MD1, Omar Iqbal, MD1, Divyanshu Mohananey, MD1, Saffia Bajwa, DO1, Masoud Khani, MS1, Jake Lou, PhD2, Daniel J. Stein, MD3, Jana G. Hashash, MD, MSc, FACG4, Emad Mansoor, MD5, Raymond K. Cross, MD, MS, FACG6, Gursimran Kochhar, MD7, Preetika Sinh, MD8. P3157 - Cardiovascular Risk Factors Drive Mortality in Patients With Inflammatory Bowel Disease - A Propensity-Matched US National Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical College of Wisconsin, Milwaukee, WI; 2University of Wisconsin, Milwaukee, WI; 3Medical College of Wisconsin, Wauwatosa, WI; 4Mayo Clinic, Jacksonville, FL; 5University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 6The Melissa L. Posner Institute for Digestive Health & Liver Disease, Mercy Medical Center, Baltimore, MD; 7Allegheny Health Network, Pittsburgh, PA; 8University of California San Diego, San Diego, CA
Introduction: Inflammatory bowel disease (IBD) is associated with an increased risk of adverse cardiovascular (CV) events and venous thromboembolism (VTE), though its impact on mortality remains debatable. The ORAL Surveillance study [NEJM 2022] found that tofacitinib, a Janus kinase inhibitor approved for ulcerative colitis (UC), was linked to increased mortality in rheumatoid arthritis patients, particularly those with CV risk factors (RFs) [Ann Rheum 2023]. We aimed to determine all-cause mortality in IBD patients and assess the role of CV and VTE RFs.
Methods: We performed a retrospective cohort study using multi-institutional database TriNetX. IBD patients [UC and Crohn’s Disease (CD)] were identified between 2015 to 2023 with the presence of LOINC codes for IBD medications (to increase the validity of diagnosis codes). Data was collected for demographics, IBD medications, CV RFs, VTE RFs and history of coronary artery disease (CAD). We compared IBD patients to 1:1 propensity score matched non IBD controls for age, gender, race, and ethnicity for outcome of all-cause mortality [specific CV mortality data is not validated in TriNetx]. Patients with other chronic inflammatory disorders, celiac disease, and malignancy were excluded. All outcomes were assessed after the IBD index date. Odds Ratios (OR) was used to assess association between IBD and mortality. Logistic regression was used to evaluate the impact of individual RFs in the IBD cohort.
Results: We identified 110,116 IBD patients (49% UC, 51% CD) and propensity matched non-IBD controls. Even though, IBD patients had a higher prevalence of CV RFs, VTE RFs, and CAD [Table 1] IBD was associated with overall lower all-cause mortality compared to controls (OR 0.89, 95% CI 0.85–0.91, p < 0.001) [Table 2]. On further analysis of the IBD cohort with logistic regression, IBD patients with CV RFs, especially CAD had increased mortality as compared to IBD patients without CV RFs (IBD only OR 0.88, 95% CI 0.84–0.91 vs. IBD + CAD OR 4.41, 95% CI 4.18–4.65). Prior VTE was not associated with increased mortality.
Discussion: IBD patients have lower all-cause mortality compared to matched non-IBD controls. However, the presence of CV RFs—particularly CAD—significantly increases mortality risk. Identifying and managing CV comorbidities in IBD patients is essential to improving long-term outcomes.
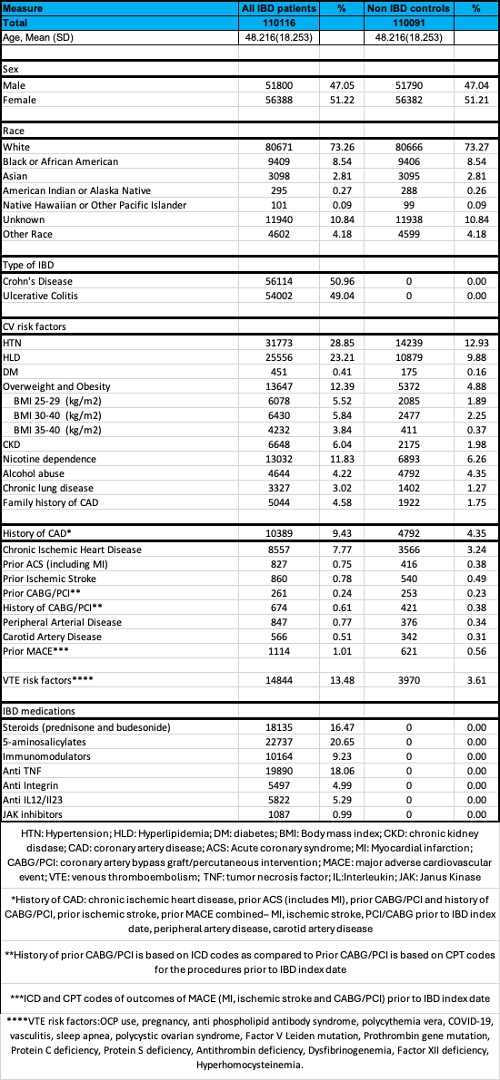
Figure: Table 1: DEMOGRAPHICS AND RISK FACTORS OF INFLAMMATORY BOWEL DISEASE PATIENTS AND CONTROLS
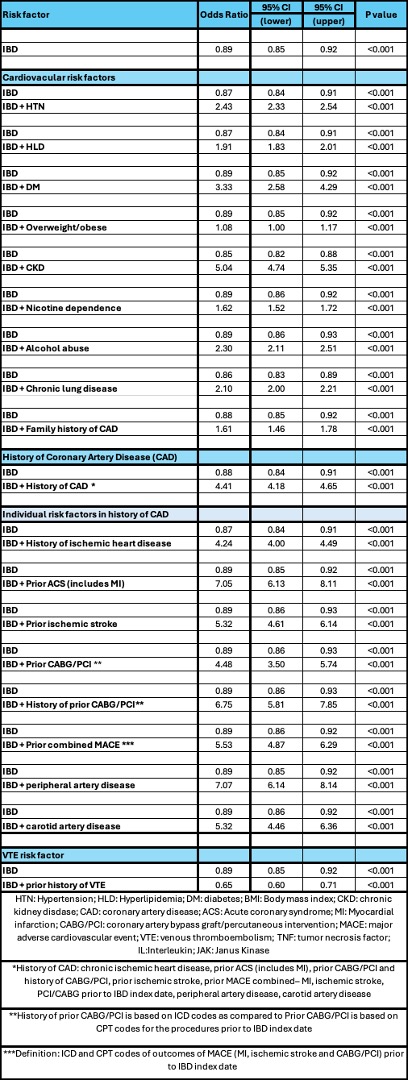
Figure: Table 2: ALL CAUSE MORTALITY IN PATIENTS WITH INFLAMMATORY BOWEL DISEASE (IBD), WITH AND WITHOUT CARDIOVASCULAR RISK FACTORS.
Disclosures:
Paraj Patel indicated no relevant financial relationships.
Omar Iqbal indicated no relevant financial relationships.
Divyanshu Mohananey indicated no relevant financial relationships.
Saffia Bajwa indicated no relevant financial relationships.
Masoud Khani indicated no relevant financial relationships.
Jake Lou indicated no relevant financial relationships.
Daniel Stein: Abbvie – Advisory Committee/Board Member. Abbvie – Speakers Bureau. BMS – Speakers Bureau. Lilly – Speakers Bureau.
Jana Hashash: BMS – Ad Board.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Raymond K. Cross: Abbvie – Advisor or Review Panel Member, Consultant, Speakers Bureau. BMS – Advisor or Review Panel Member, Consultant, Speakers Bureau. CorEvitas – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member, Consultant. Genetech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. IBD Education Group – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Advisory Committee/Board Member, Consultant. Option Care – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speakers Bureau. Pharmacosmos – Advisory Committee/Board Member, Consultant. Samsung Bioepis – Advisory Committee/Board Member, Consultant. Sandoz – Advisory Committee/Board Member, Consultant. Takeda – Grant/Research Support.
Gursimran Kochhar indicated no relevant financial relationships.
Preetika Sinh: Advisory board BMS – Advisor or Review Panel Member.
Paraj Patel, MD1, Omar Iqbal, MD1, Divyanshu Mohananey, MD1, Saffia Bajwa, DO1, Masoud Khani, MS1, Jake Lou, PhD2, Daniel J. Stein, MD3, Jana G. Hashash, MD, MSc, FACG4, Emad Mansoor, MD5, Raymond K. Cross, MD, MS, FACG6, Gursimran Kochhar, MD7, Preetika Sinh, MD8. P3157 - Cardiovascular Risk Factors Drive Mortality in Patients With Inflammatory Bowel Disease - A Propensity-Matched US National Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
