Monday Poster Session
Category: GI Bleeding
P3109 - Uncommon and Unrelenting: Gastric Amyloidosis as a Rare but Problematic Cause of GI Bleeding in AL Amyloidosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Meeta Bhardwaj, DO, MPH (she/her/hers)
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Meeta Bhardwaj, DO, MPH1, Nakul Bhardwaj, DO, MPH2, Mina Awadallah, MD, MSc2, Gillian Hale, MD, MPH2, John Erikson Yap, MD, MBA, FACG3
1Cleveland Clinic Foundation, Cleveland, OH; 2University of Utah, Salt Lake City, UT; 3University of Utah Health, Salt Lake City, UT
Introduction: Gastric amyloidosis is a rare manifestation of systemic amyloidosis that results from the deposition of amyloid fibrils within gastric tissue, leading to impaired gastrointestinal (GI) function. Symptoms ranging from non-specific dyspepsia to life-threatening GI bleed have been reported. Despite advances in diagnostics and biopsy techniques, early recognition of gastric amyloidosis remains difficult, often due to nonspecific presenting symptoms that may overlap with other GI disorders. This case describes a patient who presented with active GI bleeding due to gastric amyloidosis confirmed by endoscopic biopsy.
Case Description/
Methods: This is a 57-year-old female with multiple myeloma and recently diagnosed systemic AL-kappa light chain amyloidosis biopsy proven in GI tract with suspected cardiac, renal, and lingual involvement who was admitted for induction of multiple myeloma therapy. During admission, patient developed hypotension and lactic acidosis while admitted concerning for shock and requiring transfer to ICU. Shock etiology concerning for mixed obstructive-hypovolemic-cardiogenic shock due to cardiac tamponade and concern for GI bleed with hematochezia noted while inpatient. Patient underwent EGD showing active oozing of a nodular mucosa in the gastric antrum. The area was biopsied and came back consistent with gastric amyloid and the area was sprayed with hemostatic powder given the limited options for hemostasis. Other interventions, such as albumin supplementation, did not improve her hypovolemia and patient remained in shock. Patient elected for a comfort-based approach to care. She transitioned to comfort measures only and passed shortly after.
Discussion: Gastric amyloidosis is an uncommon but clinically significant cause of gastrointestinal bleeding, particularly in patients with systemic AL amyloidosis. Amyloid deposition in the gastric mucosa can lead to vascular fragility and mucosal disruption, predisposing patients to spontaneous bleeding. Endoscopic findings are often subtle or nonspecific, including erythema, nodularity, or mass-like lesions that may mimic malignancy. Diagnosis relies on histologic confirmation with Congo red staining. This case highlights the importance of considering gastric amyloidosis in patients with unexplained GI bleeding and known or suspected systemic amyloidosis, as timely recognition can guide appropriate therapy and improve outcomes.
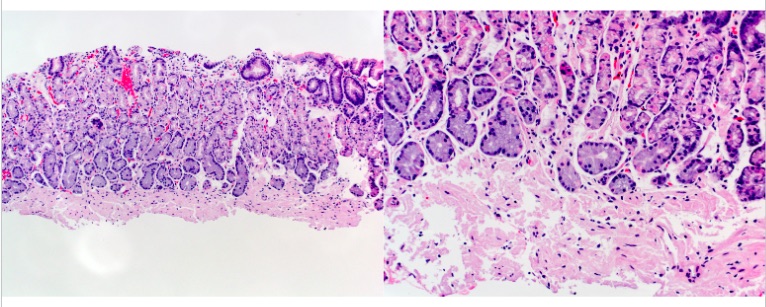
Figure: Gastric amyloidosis. Left: Gastric mucosa with prominent expanded muscularis mucosae by amorphous pink material (H+E stain, 10X). Right: Amorphous pink material appears to disrupt the muscularis mucosae on higher power (H+E stain, 20X). The amorphous, eosinophilic proteinaceous deposits expanding the interstitial spaces can often surround blood vessels and glandular structures. These deposits can lead to impaired gastric function and potential bleeding.
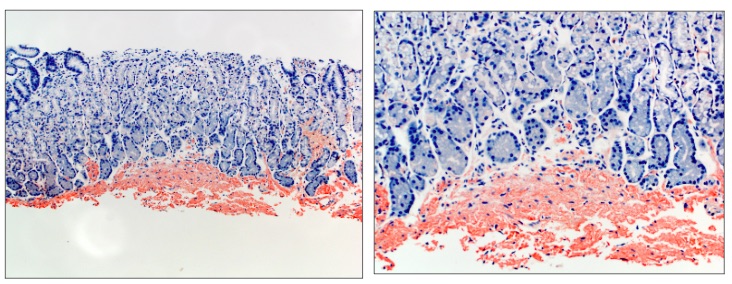
Figure: Gastric amyloidosis. Characteristic extracellular, amorphous eosinophilic deposits within the gastric wall, consistent with amyloid deposition. The material of interest is diffusely highlighted by a Congo red special stain (left, 10X; right, 20X) and shows apple-green birefringence under polarized light.
Disclosures:
Meeta Bhardwaj indicated no relevant financial relationships.
Nakul Bhardwaj indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
Gillian Hale indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Meeta Bhardwaj, DO, MPH1, Nakul Bhardwaj, DO, MPH2, Mina Awadallah, MD, MSc2, Gillian Hale, MD, MPH2, John Erikson Yap, MD, MBA, FACG3. P3109 - Uncommon and Unrelenting: Gastric Amyloidosis as a Rare but Problematic Cause of GI Bleeding in AL Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2University of Utah, Salt Lake City, UT; 3University of Utah Health, Salt Lake City, UT
Introduction: Gastric amyloidosis is a rare manifestation of systemic amyloidosis that results from the deposition of amyloid fibrils within gastric tissue, leading to impaired gastrointestinal (GI) function. Symptoms ranging from non-specific dyspepsia to life-threatening GI bleed have been reported. Despite advances in diagnostics and biopsy techniques, early recognition of gastric amyloidosis remains difficult, often due to nonspecific presenting symptoms that may overlap with other GI disorders. This case describes a patient who presented with active GI bleeding due to gastric amyloidosis confirmed by endoscopic biopsy.
Case Description/
Methods: This is a 57-year-old female with multiple myeloma and recently diagnosed systemic AL-kappa light chain amyloidosis biopsy proven in GI tract with suspected cardiac, renal, and lingual involvement who was admitted for induction of multiple myeloma therapy. During admission, patient developed hypotension and lactic acidosis while admitted concerning for shock and requiring transfer to ICU. Shock etiology concerning for mixed obstructive-hypovolemic-cardiogenic shock due to cardiac tamponade and concern for GI bleed with hematochezia noted while inpatient. Patient underwent EGD showing active oozing of a nodular mucosa in the gastric antrum. The area was biopsied and came back consistent with gastric amyloid and the area was sprayed with hemostatic powder given the limited options for hemostasis. Other interventions, such as albumin supplementation, did not improve her hypovolemia and patient remained in shock. Patient elected for a comfort-based approach to care. She transitioned to comfort measures only and passed shortly after.
Discussion: Gastric amyloidosis is an uncommon but clinically significant cause of gastrointestinal bleeding, particularly in patients with systemic AL amyloidosis. Amyloid deposition in the gastric mucosa can lead to vascular fragility and mucosal disruption, predisposing patients to spontaneous bleeding. Endoscopic findings are often subtle or nonspecific, including erythema, nodularity, or mass-like lesions that may mimic malignancy. Diagnosis relies on histologic confirmation with Congo red staining. This case highlights the importance of considering gastric amyloidosis in patients with unexplained GI bleeding and known or suspected systemic amyloidosis, as timely recognition can guide appropriate therapy and improve outcomes.
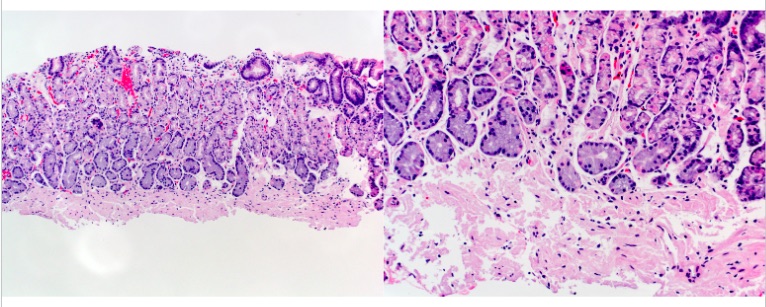
Figure: Gastric amyloidosis. Left: Gastric mucosa with prominent expanded muscularis mucosae by amorphous pink material (H+E stain, 10X). Right: Amorphous pink material appears to disrupt the muscularis mucosae on higher power (H+E stain, 20X). The amorphous, eosinophilic proteinaceous deposits expanding the interstitial spaces can often surround blood vessels and glandular structures. These deposits can lead to impaired gastric function and potential bleeding.
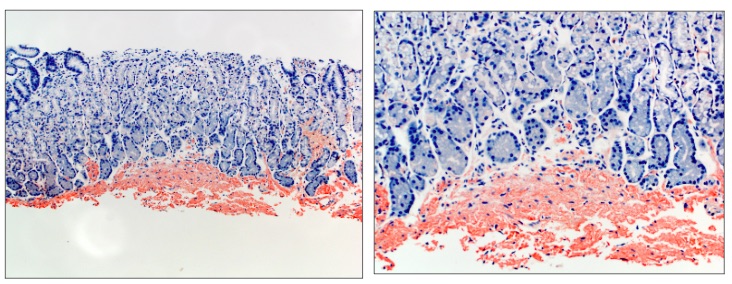
Figure: Gastric amyloidosis. Characteristic extracellular, amorphous eosinophilic deposits within the gastric wall, consistent with amyloid deposition. The material of interest is diffusely highlighted by a Congo red special stain (left, 10X; right, 20X) and shows apple-green birefringence under polarized light.
Disclosures:
Meeta Bhardwaj indicated no relevant financial relationships.
Nakul Bhardwaj indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
Gillian Hale indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Meeta Bhardwaj, DO, MPH1, Nakul Bhardwaj, DO, MPH2, Mina Awadallah, MD, MSc2, Gillian Hale, MD, MPH2, John Erikson Yap, MD, MBA, FACG3. P3109 - Uncommon and Unrelenting: Gastric Amyloidosis as a Rare but Problematic Cause of GI Bleeding in AL Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
