Monday Poster Session
Category: GI Bleeding
P3107 - Hidden Hemorrhage: A Case of Jejunal Diverticular Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jake MacDonald, MD (he/him/his)
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Jake MacDonald, MD1, Bernard Evenhuis, MD1, Aaron Hein, MD1, Steven Keilin, MD2
1Emory University School of Medicine, Atlanta, GA; 2Emory University Hospital, Atlanta, GA
Introduction: Small bowel diverticula (SBD) are rare, accounting for 0.9-2.3% of gastrointestinal (GI) diverticula. SBD are often asymptomatic but can lead to significant complications, including diverticulitis, perforation, and hemorrhage. Bleeding from jejunal diverticula (JD) is difficult to diagnose given the location, and delays in diagnosis may lead to complications such as life-threatening bleed. We present a case of acute hypotensive hematochezia due to a JD bleed, successfully managed with double balloon enteroscopy (DBE) and hemostatic clipping.
Case Description/
Methods: A 76-year-old female with peripheral artery disease, atrial fibrillation, and multiple prior GI bleeds presumed due to erosive gastropathy and small bowel angioectasias on video capsule endoscopy (VCE) 5 months prior initially presented with limb ischemia due to thrombosis of a right femoral artery graft. Hospital course was complicated by myocardial infarction, requiring stent placement and anti-thrombotic therapy. She then developed recurrent melena leading to hemorrhagic shock and intensive care admission. CT angiography failed to localize the bleed. DBE revealed an actively bleeding large mid-jejunal diverticulum (Fig. 1). She underwent injection of epinephrine and hemostatic clip placement. Anti-thrombotics were resumed, and no further bleeding was noted.
Discussion: JD form due to mucosal herniation at vasa recta sites, likely driven by dyskinesia, elevated intraluminal pressure, and chronic inflammation. Visceral neuropathy may also play a role in pathogenesis. While duodenal diverticula are more common and present with hematemesis, JD more often cause hematochezia, as in this case.
JD bleeding is difficult to diagnose due to its location and frequent obscuration by mesenteric folds. CT angiography is the most effective modality in acute settings, as it may rapidly localize active bleeding. VCE, device-assisted enteroscopy, or tagged RBC scans may be useful in cases of chronic or intermittent bleeding. Management varies by clinical stability: supportive care may suffice for mild bleeding, however definitive control for persistent bleeds may require angiographic embolization or, if refractory, surgical resection.
This case highlights the importance of considering JD bleeding in obscure GI bleeds. Early imaging and timely intervention may prevent severe complications and improve outcomes.
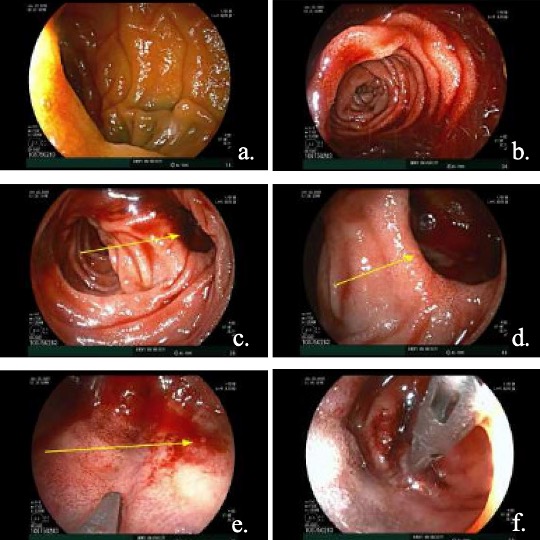
Figure: Figure 1. DBE Findings a. Tattoo of proximal jejunum evaluated on prior push enteroscopy. b. Fresh blood in the mid-jejunum. c-d. Mid-jejunal diverticulum with active bleeding. e. Active oozing of blood within mid-jejunal diverticulum. f. Cessation of bleeding after hemostatic clip placement.
Disclosures:
Jake MacDonald indicated no relevant financial relationships.
Bernard Evenhuis indicated no relevant financial relationships.
Aaron Hein indicated no relevant financial relationships.
Steven Keilin indicated no relevant financial relationships.
Jake MacDonald, MD1, Bernard Evenhuis, MD1, Aaron Hein, MD1, Steven Keilin, MD2. P3107 - Hidden Hemorrhage: A Case of Jejunal Diverticular Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Emory University School of Medicine, Atlanta, GA; 2Emory University Hospital, Atlanta, GA
Introduction: Small bowel diverticula (SBD) are rare, accounting for 0.9-2.3% of gastrointestinal (GI) diverticula. SBD are often asymptomatic but can lead to significant complications, including diverticulitis, perforation, and hemorrhage. Bleeding from jejunal diverticula (JD) is difficult to diagnose given the location, and delays in diagnosis may lead to complications such as life-threatening bleed. We present a case of acute hypotensive hematochezia due to a JD bleed, successfully managed with double balloon enteroscopy (DBE) and hemostatic clipping.
Case Description/
Methods: A 76-year-old female with peripheral artery disease, atrial fibrillation, and multiple prior GI bleeds presumed due to erosive gastropathy and small bowel angioectasias on video capsule endoscopy (VCE) 5 months prior initially presented with limb ischemia due to thrombosis of a right femoral artery graft. Hospital course was complicated by myocardial infarction, requiring stent placement and anti-thrombotic therapy. She then developed recurrent melena leading to hemorrhagic shock and intensive care admission. CT angiography failed to localize the bleed. DBE revealed an actively bleeding large mid-jejunal diverticulum (Fig. 1). She underwent injection of epinephrine and hemostatic clip placement. Anti-thrombotics were resumed, and no further bleeding was noted.
Discussion: JD form due to mucosal herniation at vasa recta sites, likely driven by dyskinesia, elevated intraluminal pressure, and chronic inflammation. Visceral neuropathy may also play a role in pathogenesis. While duodenal diverticula are more common and present with hematemesis, JD more often cause hematochezia, as in this case.
JD bleeding is difficult to diagnose due to its location and frequent obscuration by mesenteric folds. CT angiography is the most effective modality in acute settings, as it may rapidly localize active bleeding. VCE, device-assisted enteroscopy, or tagged RBC scans may be useful in cases of chronic or intermittent bleeding. Management varies by clinical stability: supportive care may suffice for mild bleeding, however definitive control for persistent bleeds may require angiographic embolization or, if refractory, surgical resection.
This case highlights the importance of considering JD bleeding in obscure GI bleeds. Early imaging and timely intervention may prevent severe complications and improve outcomes.
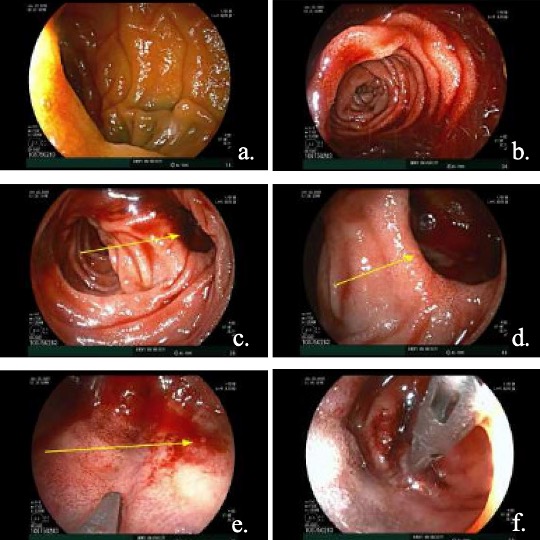
Figure: Figure 1. DBE Findings a. Tattoo of proximal jejunum evaluated on prior push enteroscopy. b. Fresh blood in the mid-jejunum. c-d. Mid-jejunal diverticulum with active bleeding. e. Active oozing of blood within mid-jejunal diverticulum. f. Cessation of bleeding after hemostatic clip placement.
Disclosures:
Jake MacDonald indicated no relevant financial relationships.
Bernard Evenhuis indicated no relevant financial relationships.
Aaron Hein indicated no relevant financial relationships.
Steven Keilin indicated no relevant financial relationships.
Jake MacDonald, MD1, Bernard Evenhuis, MD1, Aaron Hein, MD1, Steven Keilin, MD2. P3107 - Hidden Hemorrhage: A Case of Jejunal Diverticular Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
