Monday Poster Session
Category: GI Bleeding
P3102 - A Rare Double Complication: Gastroduodenal Artery Pseudoaneurysm and Intraductal Air Secondary to Duodenal Ulcer Without Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Priya Kumari Maheshwari, MD (she/her/hers)
University of Central Florida, HCA Healthcare GME
Pensacola, FL
Presenting Author(s)
Priya Kumari Maheshwari, MD1, Temitope Omoladun-Tijani, MD, MPH2, Andrew L. Petrou, MD2, John Paul Nsubuga, MD2, Amer B. Malik, MD3
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Brown University / Rhode Island Hospital, Providence, RI; 3Warren Alpert Medical School of Brown University, Providence, RI
Introduction: Duodenal ulcers are common gastrointestinal lesions typically associated with Helicobacter pylori infection or chronic nonsteroidal anti-inflammatory drug (NSAID) use. While bleeding and perforation are well-known complications, vascular involvement such as gastroduodenal artery (GDA) pseudoaneurysm is rare, especially in the absence of pancreatitis. Additionally, intraductal air in the pancreatic duct is an uncommon radiologic finding, usually linked to trauma, instrumentation, fistula, or malignancy. We describe a rare case of a duodenal ulcer complicated by both GDA pseudoaneurysm and intraductal air, without evidence of pancreatitis, malignancy, or prior intervention.
Case Description/
Methods: An 82-year-old woman with chronic NSAID use for back pain presented with sudden-onset epigastric pain. She was hemodynamically stable, but labs showed a hemoglobin of 6.7 g/dL, down from 8.0 g/dL the prior week. Computed tomography (CT) of the abdomen and pelvis revealed duodenitis and intraductal air, later confirmed by magnetic resonance cholangiopancreatography (MRCP) without obstruction or mass. She received intravenous proton pump inhibitors and two units of packed red blood cells.
Esophagogastroduodenoscopy (EGD) showed a duodenal bulb ulcer with an adherent clot treated with argon plasma coagulation (APC), and multiple oozing ulcers in the second portion of the duodenum treated with epinephrine injection, APC, and hemostatic spray. Post-procedure, she developed melena and hemodynamic instability, requiring additional transfusions. CT angiography (CTA) revealed a new GDA pseudoaneurysm, likely from ulcer erosion. Embolization was performed successfully, and her condition stabilized. Repeat imaging showed no active bleeding. She was discharged in stable condition with plans for outpatient follow-up and repeat MRCP.
Discussion: GDA pseudoaneurysms are rare and typically associated with chronic pancreatitis. In this case, there was no history or imaging evidence of pancreatitis, and prior scans showed no vascular abnormalities. The pseudoaneurysm likely resulted from ulcer-related erosion and adjacent inflammation. Intraductal air was present without biliary involvement, raising concern for mucosal breach or direct ulcer penetration. Although pancreatic malignancy is a differential in such cases, it was not supported by MRCP or endoscopic findings. This case highlights the need to consider rare vascular and structural complications in duodenal ulcers with atypical imaging features.
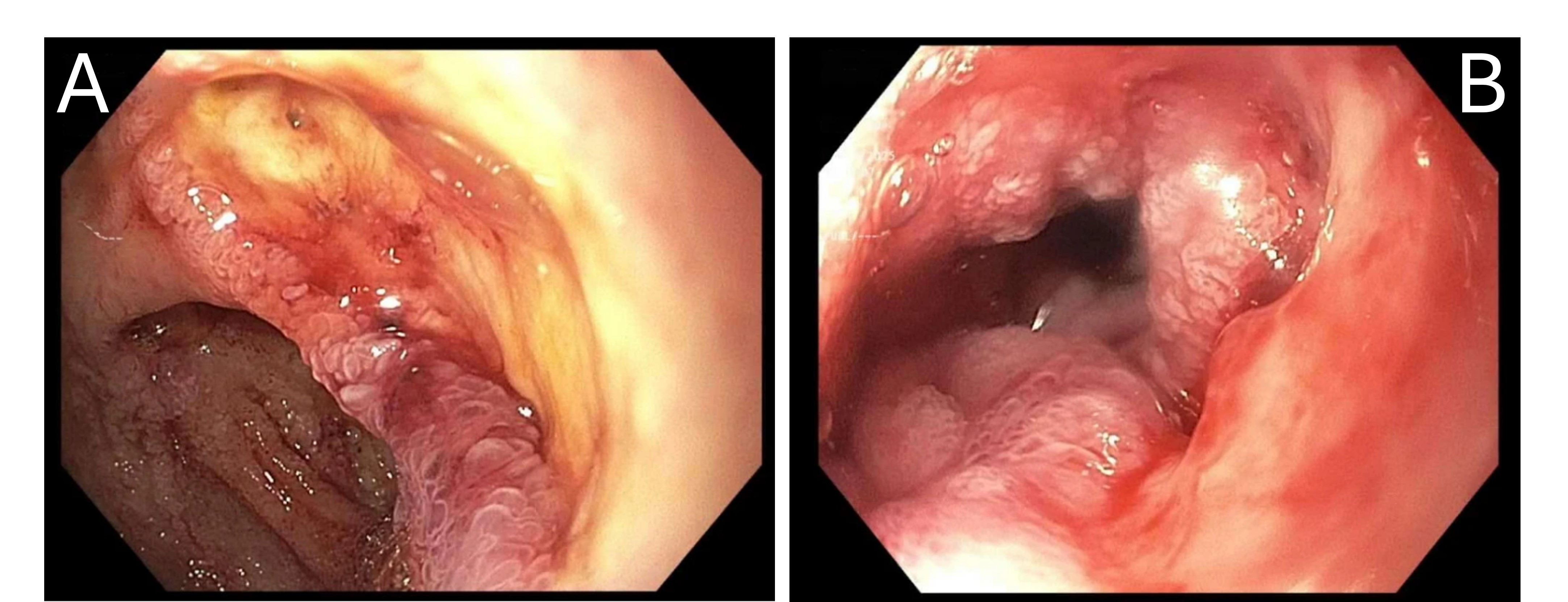
Figure: Figure 1A: Endoscopic image of the duodenal bulb showing a deep ulcer and surrounding erythema. Figure 1B: Endoscopic view of the duodenum demonstrating multiple oozing ulcers with friable, inflamed mucosa.
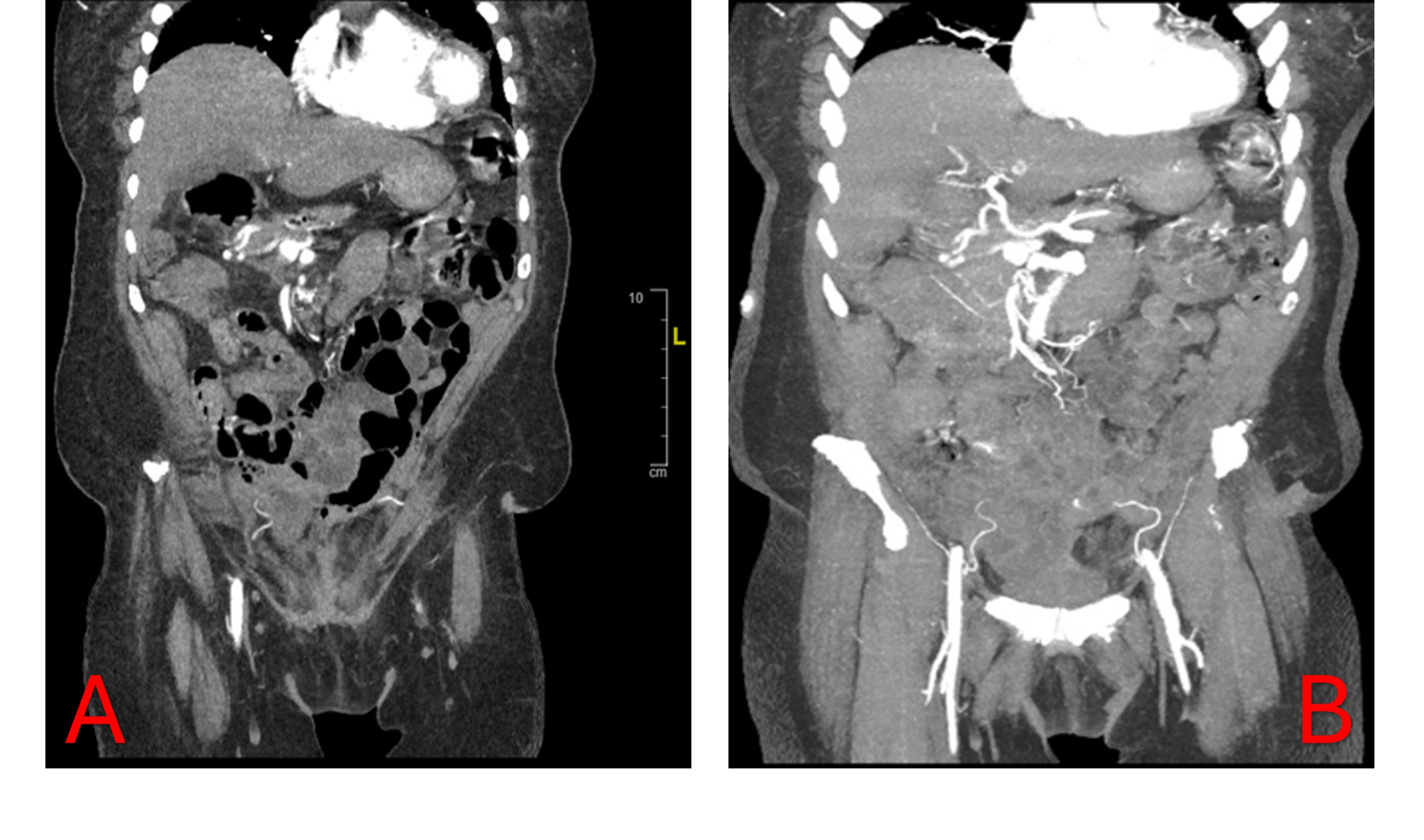
Figure: Figure 2A: Coronal contrast-enhanced CT showing intraductal air within the pancreatic duct without evidence of pancreatitis. Figure 2B: CT angiography revealing a gastroduodenal artery pseudoaneurysm adjacent to the duodenum, consistent with vascular erosion from ulceration.
Disclosures:
Priya Kumari Maheshwari indicated no relevant financial relationships.
Temitope Omoladun-Tijani indicated no relevant financial relationships.
Andrew Petrou indicated no relevant financial relationships.
John Paul Nsubuga indicated no relevant financial relationships.
Amer Malik indicated no relevant financial relationships.
Priya Kumari Maheshwari, MD1, Temitope Omoladun-Tijani, MD, MPH2, Andrew L. Petrou, MD2, John Paul Nsubuga, MD2, Amer B. Malik, MD3. P3102 - A Rare Double Complication: Gastroduodenal Artery Pseudoaneurysm and Intraductal Air Secondary to Duodenal Ulcer Without Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Pensacola, FL; 2Brown University / Rhode Island Hospital, Providence, RI; 3Warren Alpert Medical School of Brown University, Providence, RI
Introduction: Duodenal ulcers are common gastrointestinal lesions typically associated with Helicobacter pylori infection or chronic nonsteroidal anti-inflammatory drug (NSAID) use. While bleeding and perforation are well-known complications, vascular involvement such as gastroduodenal artery (GDA) pseudoaneurysm is rare, especially in the absence of pancreatitis. Additionally, intraductal air in the pancreatic duct is an uncommon radiologic finding, usually linked to trauma, instrumentation, fistula, or malignancy. We describe a rare case of a duodenal ulcer complicated by both GDA pseudoaneurysm and intraductal air, without evidence of pancreatitis, malignancy, or prior intervention.
Case Description/
Methods: An 82-year-old woman with chronic NSAID use for back pain presented with sudden-onset epigastric pain. She was hemodynamically stable, but labs showed a hemoglobin of 6.7 g/dL, down from 8.0 g/dL the prior week. Computed tomography (CT) of the abdomen and pelvis revealed duodenitis and intraductal air, later confirmed by magnetic resonance cholangiopancreatography (MRCP) without obstruction or mass. She received intravenous proton pump inhibitors and two units of packed red blood cells.
Esophagogastroduodenoscopy (EGD) showed a duodenal bulb ulcer with an adherent clot treated with argon plasma coagulation (APC), and multiple oozing ulcers in the second portion of the duodenum treated with epinephrine injection, APC, and hemostatic spray. Post-procedure, she developed melena and hemodynamic instability, requiring additional transfusions. CT angiography (CTA) revealed a new GDA pseudoaneurysm, likely from ulcer erosion. Embolization was performed successfully, and her condition stabilized. Repeat imaging showed no active bleeding. She was discharged in stable condition with plans for outpatient follow-up and repeat MRCP.
Discussion: GDA pseudoaneurysms are rare and typically associated with chronic pancreatitis. In this case, there was no history or imaging evidence of pancreatitis, and prior scans showed no vascular abnormalities. The pseudoaneurysm likely resulted from ulcer-related erosion and adjacent inflammation. Intraductal air was present without biliary involvement, raising concern for mucosal breach or direct ulcer penetration. Although pancreatic malignancy is a differential in such cases, it was not supported by MRCP or endoscopic findings. This case highlights the need to consider rare vascular and structural complications in duodenal ulcers with atypical imaging features.
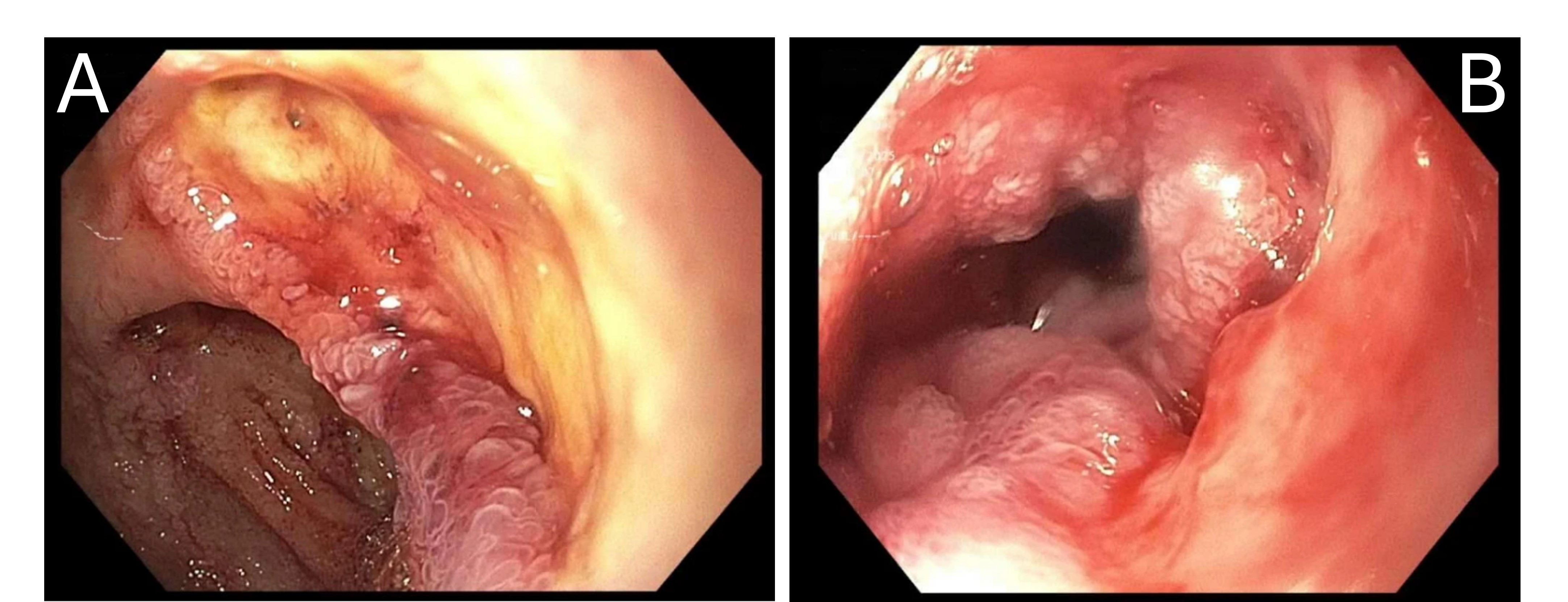
Figure: Figure 1A: Endoscopic image of the duodenal bulb showing a deep ulcer and surrounding erythema. Figure 1B: Endoscopic view of the duodenum demonstrating multiple oozing ulcers with friable, inflamed mucosa.
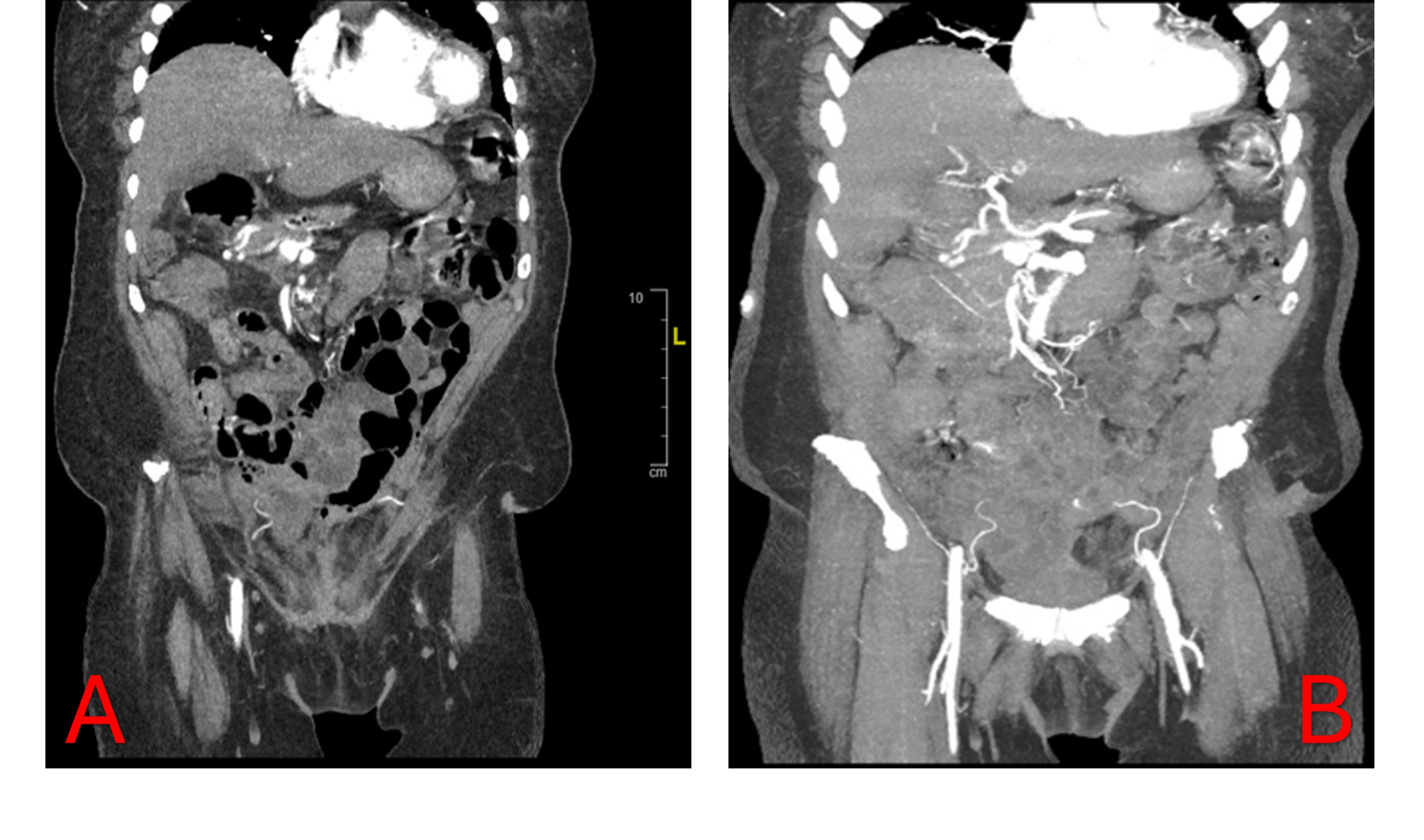
Figure: Figure 2A: Coronal contrast-enhanced CT showing intraductal air within the pancreatic duct without evidence of pancreatitis. Figure 2B: CT angiography revealing a gastroduodenal artery pseudoaneurysm adjacent to the duodenum, consistent with vascular erosion from ulceration.
Disclosures:
Priya Kumari Maheshwari indicated no relevant financial relationships.
Temitope Omoladun-Tijani indicated no relevant financial relationships.
Andrew Petrou indicated no relevant financial relationships.
John Paul Nsubuga indicated no relevant financial relationships.
Amer Malik indicated no relevant financial relationships.
Priya Kumari Maheshwari, MD1, Temitope Omoladun-Tijani, MD, MPH2, Andrew L. Petrou, MD2, John Paul Nsubuga, MD2, Amer B. Malik, MD3. P3102 - A Rare Double Complication: Gastroduodenal Artery Pseudoaneurysm and Intraductal Air Secondary to Duodenal Ulcer Without Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
