Monday Poster Session
Category: GI Bleeding
P3100 - When the SVC Blocks the Way: A Rare Route to Esophageal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ade Waterman, MBChB (he/him/his)
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Award: ACG Presidential Poster Award
Ade Waterman, MBChB1, Adam Khalaf, MD1, Ahmad Abdulraheem, MD2, Michael Tseng, MD1, Ghassan Alzayer, MD3
1MedStar Georgetown University Hospital, Washington, DC; 2MedStar Washington Hospital Center, Washington, DC; 3MedStar Health, Washington, DC
Introduction: This case highlights the presentation and management of "downhill" esophageal varices, a rare cause of upper GI bleeding resulting from superior vena cava (SVC) obstruction. These varices, distinct from portal hypertension-related "uphill" varices, are confined to the upper esophagus and occur in the absence of liver disease.
Case Description/
Methods: A 71-year-old male with a distant history of colon cancer and underwent resection and chemotherapy presented with hematemesis. CT angiography revealed dilated gastroesophageal varices without cirrhosis or signs of portal hypertension, but demonstrated focal SVC narrowing associated with a left subclavian Port-A-Cath and chest wall collaterals. EGD identified grade III varices with spurting blood, which were treated with banding; and Port-A-Cath was removed by Interventional Radiology.
Patient had recurrent hematemesis. EGD showed non-bleeding grade I varices with stigmata of recent bleeding however not amenable to banding. Venography confirmed SVC stenosis, which was treated with venoplasty and stenting. Post-procedure, the patient recovered without further bleeding and was discharged.
Discussion: "Downhill" esophageal varices account for less than 1% of variceal bleeds. Unlike portal hypertension related "uphill" varices, "downhill" varices arise from retrograde venous pressure due to SVC obstruction. This condition is most commonly associated with malignancy (60%), thrombosis, or the use of central venous catheters. The pathophysiology involves increased venous pressures in the azygos and esophageal plexuses, leading to variceal dilation in the upper esophagus. SVC obstruction is a recognized complication of long-term central venous devices, occurring in 30-50% of patients with indwelling catheters. In this case, the prolonged presence of a Port-A-Cath likely precipitated the stenosis. Clinically, downhill varices are often asymptomatic until bleeding occurs. The risk of hemorrhage is significant, with reported rates of 10-15% in patients with severe SVC obstruction. While downhill varices are less prone to rupture compared to portal hypertension-related varices, their management presents unique challenges. Definitive treatment often requires addressing the underlying SVC obstruction to prevent recurrence where venoplasty and stenting have demonstrated >90%success in restoring vascular patency and reducing recurrence of bleeding. Our case emphasizes the attention to downhill varices as a potential complication of central venous devices.
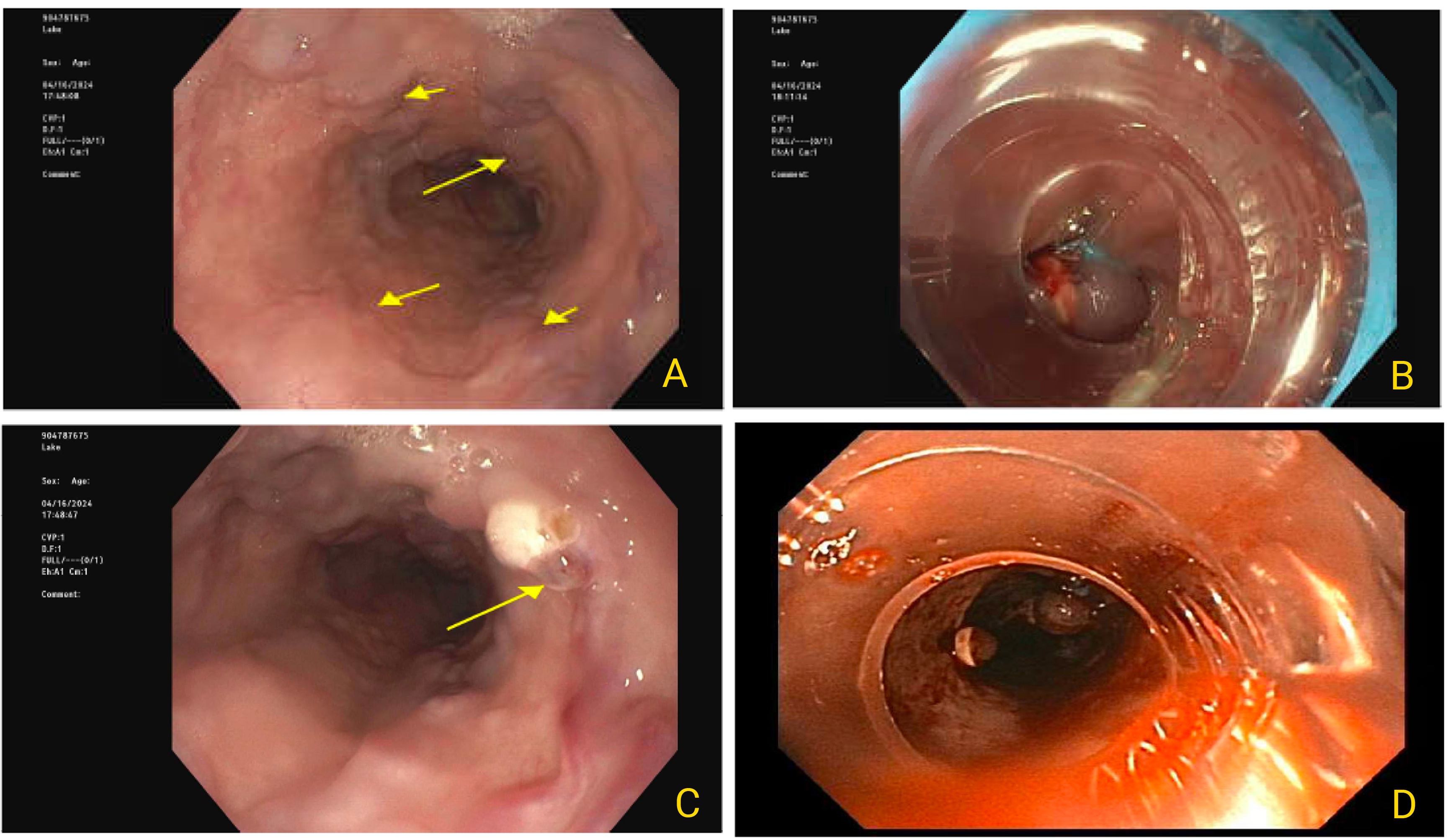
Figure: Endoscopic Images: A) Grade III esophageal varices (>5 mm) from initial endoscopy; B) Varices post-banding during first EGD; C) Slow oozing from varix at 30 cm after distal band placement during first EGD; D) Grade I esophageal varices with stigmata of recent bleeding post-banding during third endoscopy.
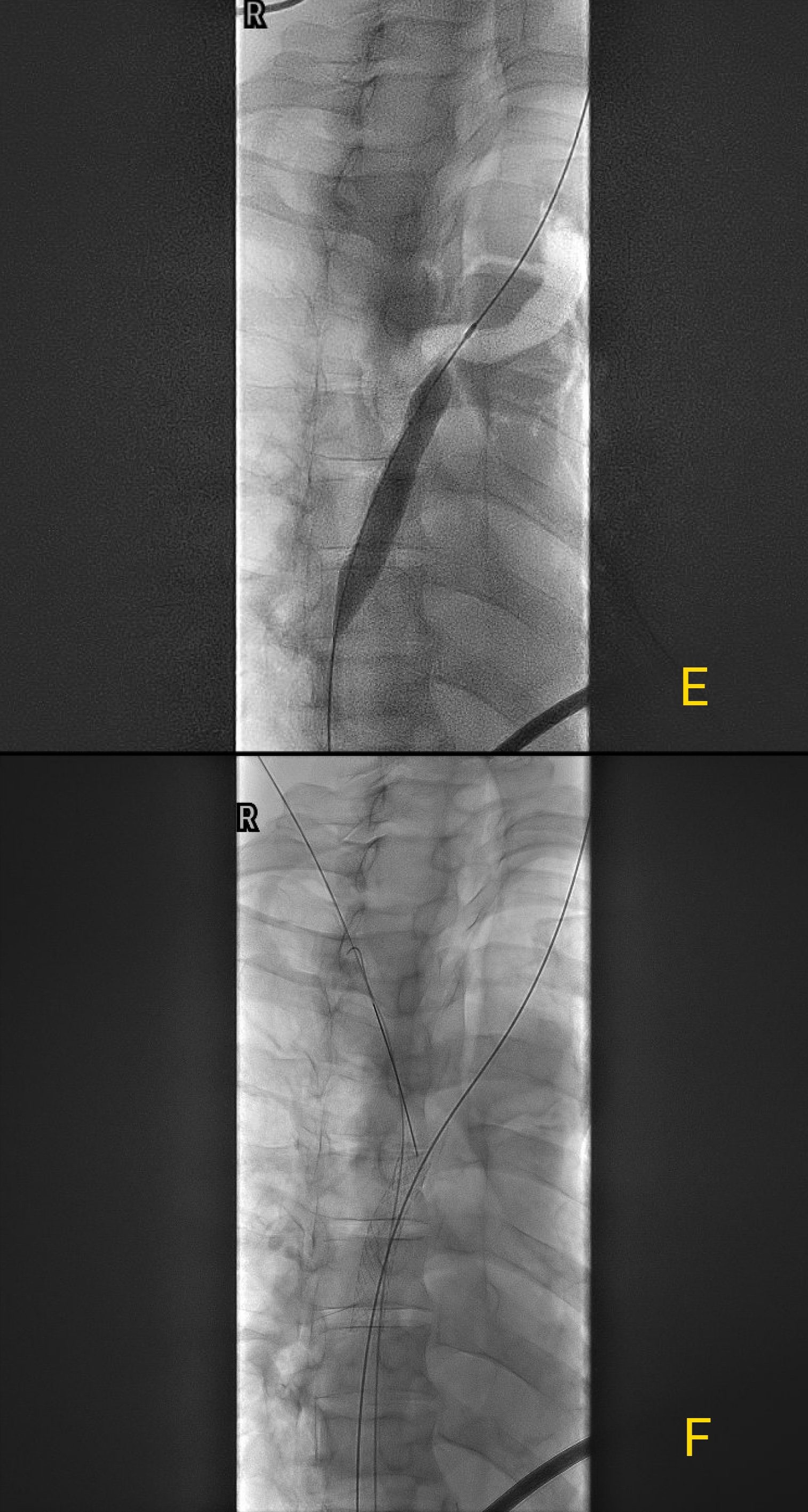
Figure: Venogram Images: E) Severe stenosis of the superior vena cava (SVC) pre-intervention; F) SVC post-stent placement with visible stent in place.
Disclosures:
Ade Waterman indicated no relevant financial relationships.
Adam Khalaf indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Michael Tseng indicated no relevant financial relationships.
Ghassan Alzayer indicated no relevant financial relationships.
Ade Waterman, MBChB1, Adam Khalaf, MD1, Ahmad Abdulraheem, MD2, Michael Tseng, MD1, Ghassan Alzayer, MD3. P3100 - When the SVC Blocks the Way: A Rare Route to Esophageal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ade Waterman, MBChB1, Adam Khalaf, MD1, Ahmad Abdulraheem, MD2, Michael Tseng, MD1, Ghassan Alzayer, MD3
1MedStar Georgetown University Hospital, Washington, DC; 2MedStar Washington Hospital Center, Washington, DC; 3MedStar Health, Washington, DC
Introduction: This case highlights the presentation and management of "downhill" esophageal varices, a rare cause of upper GI bleeding resulting from superior vena cava (SVC) obstruction. These varices, distinct from portal hypertension-related "uphill" varices, are confined to the upper esophagus and occur in the absence of liver disease.
Case Description/
Methods: A 71-year-old male with a distant history of colon cancer and underwent resection and chemotherapy presented with hematemesis. CT angiography revealed dilated gastroesophageal varices without cirrhosis or signs of portal hypertension, but demonstrated focal SVC narrowing associated with a left subclavian Port-A-Cath and chest wall collaterals. EGD identified grade III varices with spurting blood, which were treated with banding; and Port-A-Cath was removed by Interventional Radiology.
Patient had recurrent hematemesis. EGD showed non-bleeding grade I varices with stigmata of recent bleeding however not amenable to banding. Venography confirmed SVC stenosis, which was treated with venoplasty and stenting. Post-procedure, the patient recovered without further bleeding and was discharged.
Discussion: "Downhill" esophageal varices account for less than 1% of variceal bleeds. Unlike portal hypertension related "uphill" varices, "downhill" varices arise from retrograde venous pressure due to SVC obstruction. This condition is most commonly associated with malignancy (60%), thrombosis, or the use of central venous catheters. The pathophysiology involves increased venous pressures in the azygos and esophageal plexuses, leading to variceal dilation in the upper esophagus. SVC obstruction is a recognized complication of long-term central venous devices, occurring in 30-50% of patients with indwelling catheters. In this case, the prolonged presence of a Port-A-Cath likely precipitated the stenosis. Clinically, downhill varices are often asymptomatic until bleeding occurs. The risk of hemorrhage is significant, with reported rates of 10-15% in patients with severe SVC obstruction. While downhill varices are less prone to rupture compared to portal hypertension-related varices, their management presents unique challenges. Definitive treatment often requires addressing the underlying SVC obstruction to prevent recurrence where venoplasty and stenting have demonstrated >90%success in restoring vascular patency and reducing recurrence of bleeding. Our case emphasizes the attention to downhill varices as a potential complication of central venous devices.
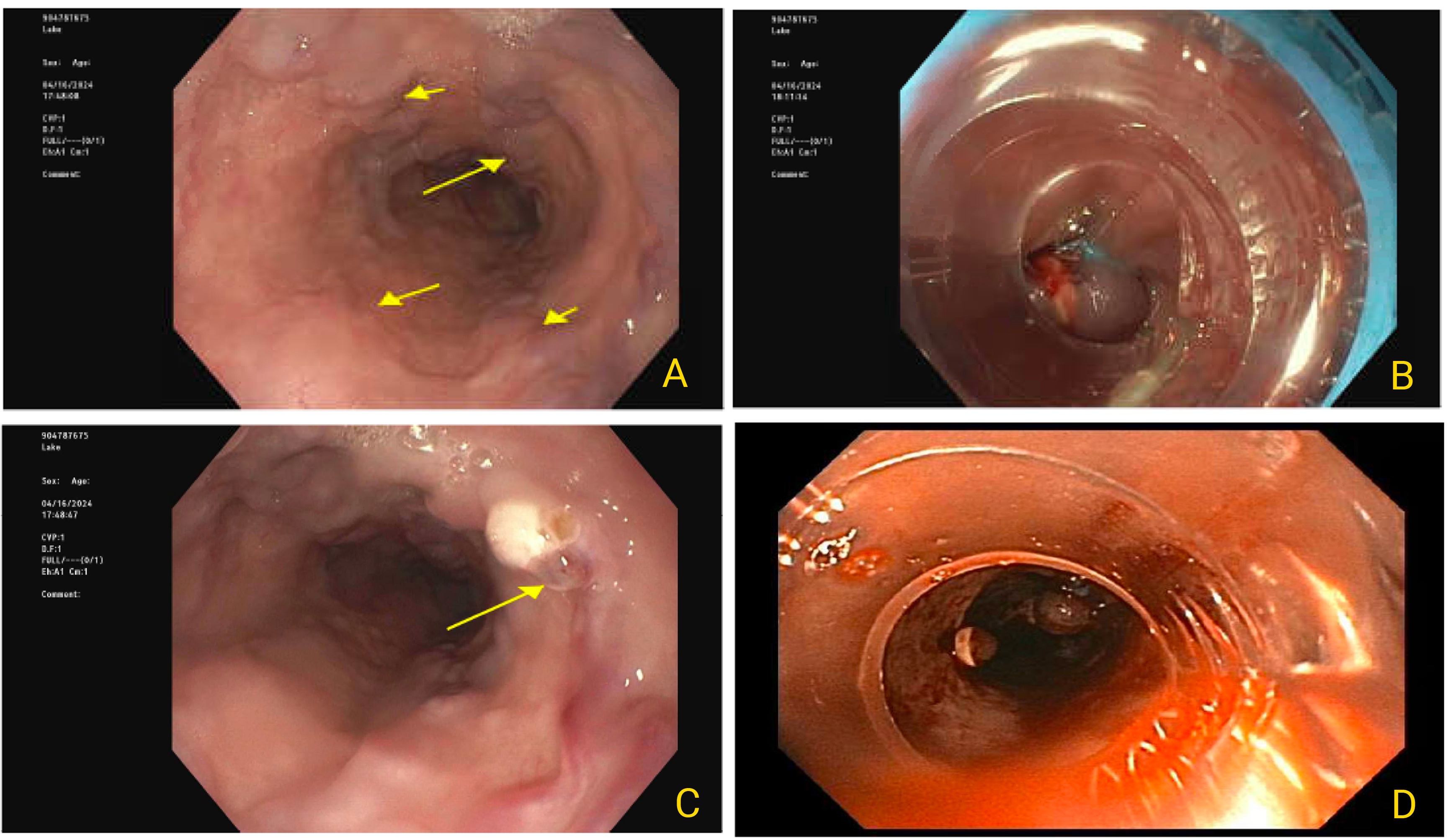
Figure: Endoscopic Images: A) Grade III esophageal varices (>5 mm) from initial endoscopy; B) Varices post-banding during first EGD; C) Slow oozing from varix at 30 cm after distal band placement during first EGD; D) Grade I esophageal varices with stigmata of recent bleeding post-banding during third endoscopy.
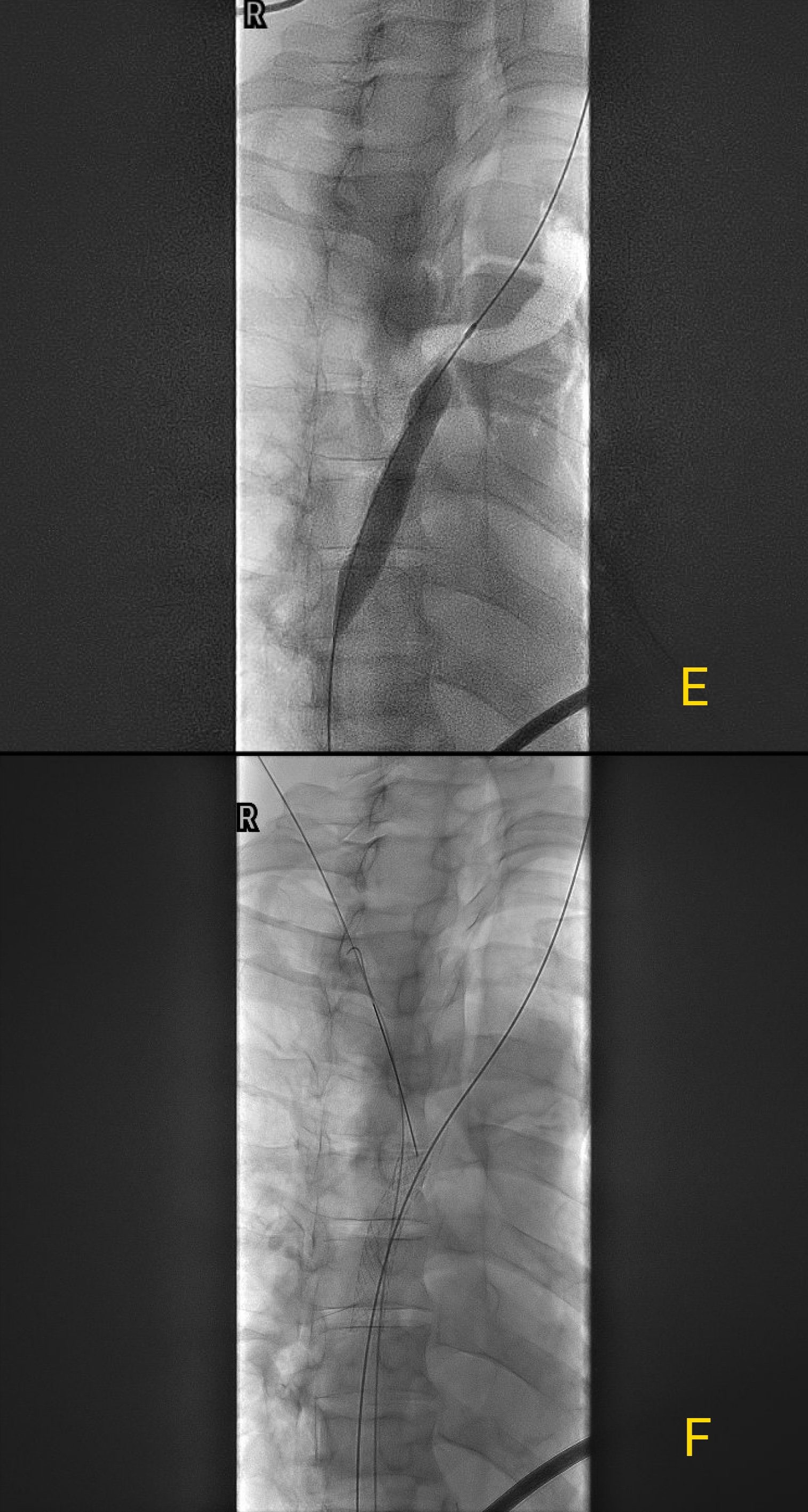
Figure: Venogram Images: E) Severe stenosis of the superior vena cava (SVC) pre-intervention; F) SVC post-stent placement with visible stent in place.
Disclosures:
Ade Waterman indicated no relevant financial relationships.
Adam Khalaf indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Michael Tseng indicated no relevant financial relationships.
Ghassan Alzayer indicated no relevant financial relationships.
Ade Waterman, MBChB1, Adam Khalaf, MD1, Ahmad Abdulraheem, MD2, Michael Tseng, MD1, Ghassan Alzayer, MD3. P3100 - When the SVC Blocks the Way: A Rare Route to Esophageal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

