Monday Poster Session
Category: GI Bleeding
P3096 - Hidden Figures: Occult Jejunal Diverticulosis Presenting as a Life-Threatening Gastrointestinal Bleed
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bobby Thomas, MD (he/him/his)
Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Bobby Thomas, MD1, Joshua Aron, MD1, Genanew Bedanie, MD2
1Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, New York, NY; 2Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Isolated jejunal diverticulosis are rare false diverticula of the proximal bowel. While usually asymptomatic, patients may present with non-specific complaints, malabsorption, perforation and rarely as a source of brisk overt GI bleeding.
Case Description/
Methods: A 67- year-old male with a history of a prior hemorrhoidal bleeding was brought to the ED for evaluation of hematochezia. Patient was hemodynamically stable without further bleeding; however, just prior to discharge the patient developed hypotension and brisk red blood per rectum. CTA was without source for GI bleeding. Patient was admitted to the MICU and labs revealed a drop in hemoglobin from 12.9 gm to 7.6 gm. BUN/Cr ratio and INR were normal. Examination with a gastroscope to the 2nd portion of the duodenum was normal and push enteroscopy was done with a pediatric colonoscope. In the mid jejunum, an 8 mm wide single jejunal diverticulum was found with red blood and a overlying fresh clot. After irrigation dislodged the clot, no underlying visible vessel or ulcer was identified. The adjacent area was tattooed and marked with a clip with surgical consultation. At laparotomy, multiple broad-based diverticula were found in the proximal to mid jejunum, and 100cm bowel was resected without further bleeding.
Discussion: First described in 1794 by pathologists Soemmerring and Baillie, isolated jejunal diverticulosis is a rare diagnosis with an incidence of 0.4-4.6% on autopsy studies. They can be identified with luminal contrast imaging but can be missed with studies such as CT angiography. Jejunal diverticulum are more common in men and older patients with 90% of affected individuals greater than 40 years of age. Giant jejunal diverticula are greater than 4 cm and are a rare cause for intestinal obstruction. Our patient presented with intermittent brisk GI bleeding masquerading as a lower GI bleed, and presenting as a self-limited sentinel event. Diagnosis of bleeding jejunal diverticula relies on either push enteroscopy or device-assisted enteroscopy. While double-balloon enteroscopy allows for visualization of the distal bowel, push enteroscopy is adequate for identification of jejunal bleeding. Hemostatic techniques for treating jejunal diverticular bleeding include hemostatic clips, argon plasma coagulation, endoscopic band ligation, and epinephrine injection. Surgery has shown to have lower rebleeding rates, but longer hospital stays. Alternatively, transcatheter embolization can be done, but this may lead to ischemic complications.

Figure: Figure 1: 8 mm Mid Jejunal Diverticula after irrigation
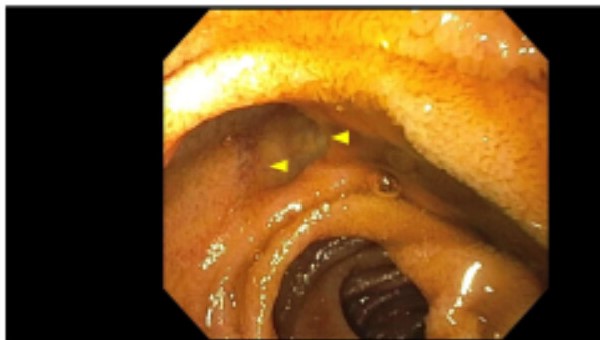
Figure: Figure 2: Diverticula following clipping for marking prior to surgical resection
Disclosures:
Bobby Thomas indicated no relevant financial relationships.
Joshua Aron indicated no relevant financial relationships.
Genanew Bedanie indicated no relevant financial relationships.
Bobby Thomas, MD1, Joshua Aron, MD1, Genanew Bedanie, MD2. P3096 - Hidden Figures: Occult Jejunal Diverticulosis Presenting as a Life-Threatening Gastrointestinal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, New York, NY; 2Elmhurst Hospital Center / Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Isolated jejunal diverticulosis are rare false diverticula of the proximal bowel. While usually asymptomatic, patients may present with non-specific complaints, malabsorption, perforation and rarely as a source of brisk overt GI bleeding.
Case Description/
Methods: A 67- year-old male with a history of a prior hemorrhoidal bleeding was brought to the ED for evaluation of hematochezia. Patient was hemodynamically stable without further bleeding; however, just prior to discharge the patient developed hypotension and brisk red blood per rectum. CTA was without source for GI bleeding. Patient was admitted to the MICU and labs revealed a drop in hemoglobin from 12.9 gm to 7.6 gm. BUN/Cr ratio and INR were normal. Examination with a gastroscope to the 2nd portion of the duodenum was normal and push enteroscopy was done with a pediatric colonoscope. In the mid jejunum, an 8 mm wide single jejunal diverticulum was found with red blood and a overlying fresh clot. After irrigation dislodged the clot, no underlying visible vessel or ulcer was identified. The adjacent area was tattooed and marked with a clip with surgical consultation. At laparotomy, multiple broad-based diverticula were found in the proximal to mid jejunum, and 100cm bowel was resected without further bleeding.
Discussion: First described in 1794 by pathologists Soemmerring and Baillie, isolated jejunal diverticulosis is a rare diagnosis with an incidence of 0.4-4.6% on autopsy studies. They can be identified with luminal contrast imaging but can be missed with studies such as CT angiography. Jejunal diverticulum are more common in men and older patients with 90% of affected individuals greater than 40 years of age. Giant jejunal diverticula are greater than 4 cm and are a rare cause for intestinal obstruction. Our patient presented with intermittent brisk GI bleeding masquerading as a lower GI bleed, and presenting as a self-limited sentinel event. Diagnosis of bleeding jejunal diverticula relies on either push enteroscopy or device-assisted enteroscopy. While double-balloon enteroscopy allows for visualization of the distal bowel, push enteroscopy is adequate for identification of jejunal bleeding. Hemostatic techniques for treating jejunal diverticular bleeding include hemostatic clips, argon plasma coagulation, endoscopic band ligation, and epinephrine injection. Surgery has shown to have lower rebleeding rates, but longer hospital stays. Alternatively, transcatheter embolization can be done, but this may lead to ischemic complications.

Figure: Figure 1: 8 mm Mid Jejunal Diverticula after irrigation
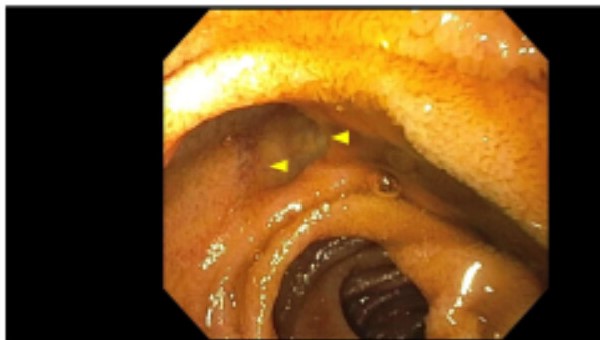
Figure: Figure 2: Diverticula following clipping for marking prior to surgical resection
Disclosures:
Bobby Thomas indicated no relevant financial relationships.
Joshua Aron indicated no relevant financial relationships.
Genanew Bedanie indicated no relevant financial relationships.
Bobby Thomas, MD1, Joshua Aron, MD1, Genanew Bedanie, MD2. P3096 - Hidden Figures: Occult Jejunal Diverticulosis Presenting as a Life-Threatening Gastrointestinal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
