Monday Poster Session
Category: GI Bleeding
P3093 - Hark the Herald Bleed
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TM
Trevor McCracken, MD (he/him/his)
University of California Irvine Health
Orange, CA
Presenting Author(s)
Trevor McCracken, MD1, Erica Duh, MD2, Ruby Chien, MD3, Nicholas Garcia, MD1, Marie Balfour, MD1, Momin Masroor, MD3, Frances Dang, MD, MSc4, Peter Nguyen, MD3, Gregory Albers, MD, FACG3
1University of California Irvine Health, Orange, CA; 2University of California Irvine Digestive Health Institute, Orange, CA; 3University of California Irvine, Orange, CA; 4University of California Irvine, Irvine, CA
Introduction: “Hark” in Shakespearean language means to “pay attention” – a relevant term when referring to minor, intermittent “herald” GI bleeds that often precede more major bleeding events. One example is an iliac-artery enteric fistula (IEF), or an abnormal connection between the iliac artery and the GI tract, which can result in massive bleeding.
Case Description/
Methods: A 48-year-old male with dual pancreatic and kidney transplants presented to the emergency department with hematochezia. His hemoglobin was 9.4, and CT imaging revealed mild fat stranding in the pancreas and rectosigmoid colon. He was previously hospitalized five years prior for similar symptoms and had an unremarkable endoscopic evaluation. Given all of this, the ED decided to transfuse one unit of red blood cells before discharging home with close outpatient follow up. Only two weeks later, he presented to the ED again for similar complaints, but this time his hemoglobin was significantly decreased to 5.4. The patient underwent repeat CT imaging which was unrevealing. He was scheduled for a colonoscopy the following day; however, upon starting his bowel prep, he developed hematochezia and eventually hemorrhagic shock. Massive transfusion protocol was activated, and interventional radiology was consulted for emergent angiography which revealed an IEF originating from the proximal right internal iliac artery at the failed pancreatic graft site. An arterial stent was placed successfully with no further evidence of contrast extravasation. Despite this, the patient developed ventricular fibrillation and cardiac arrest secondary to transfusion associated circulatory overload, and his family ultimately decided to transition to comfort measures.
Discussion: IEFs are thought to arise from pressure against the bowel wall by a graft or pseudoaneurysm in conjunction with some degree of infection leading to necrosis and then perforation or fistulization. They occur, albeit rarely, in patients with failed pancreatic transplants. This case highlights the difficulty in identifying arterial-enteric fistulas specifically in dual pancreatic and kidney transplants. While EGD and colonoscopy are the gold standards for evaluating GI bleeds, these procedures often only detect up to 25% of secondary IEFs. We feel this case to be clinically important as it is an example of one of the rarer types of GI bleeds. Let this serve as a poignant reminder to hark the herald GI bleed in patients with pancreatic transplants.
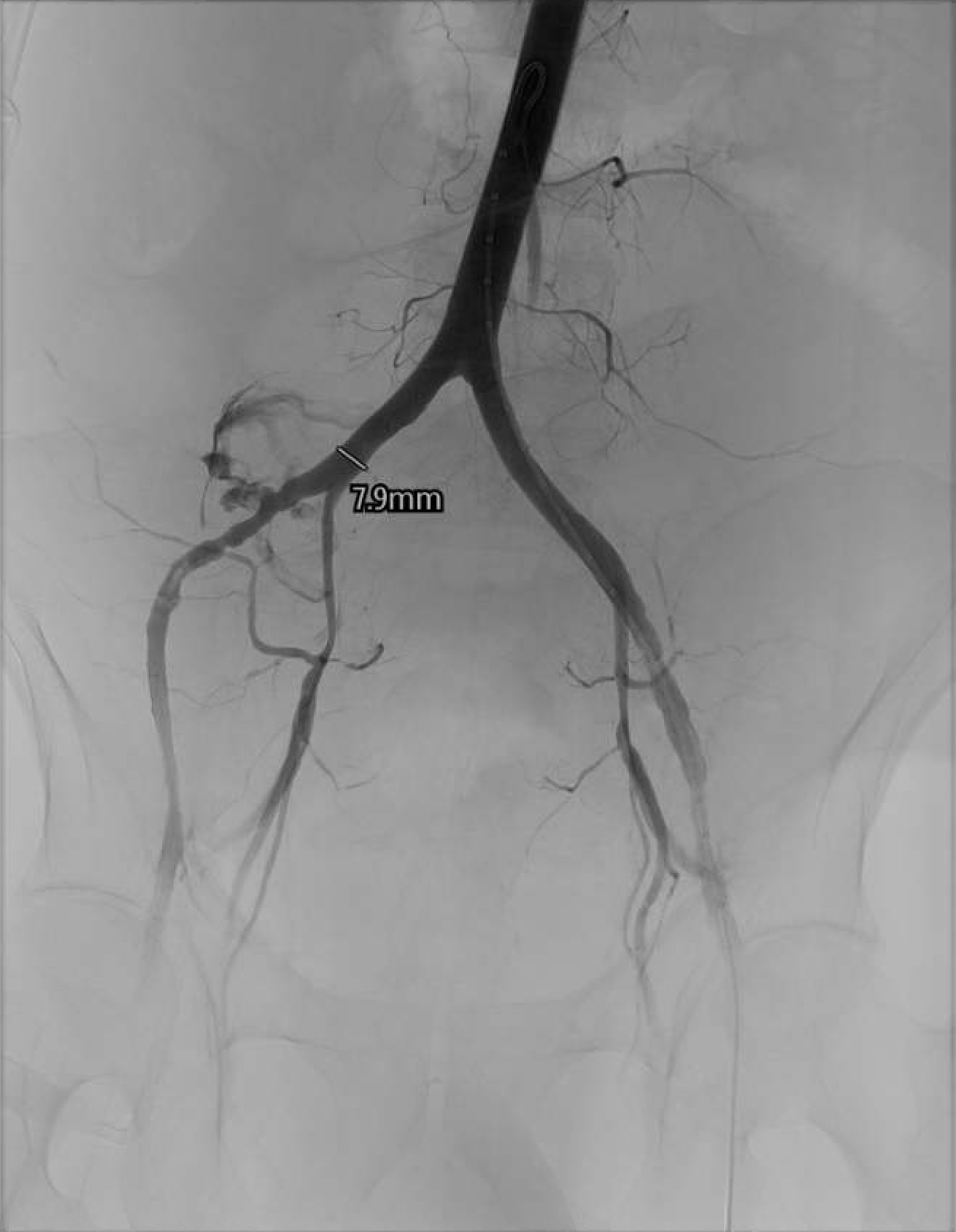
Figure: Figure 1: Angiography demonstrating an injured right internal iliac artery with massive extravasation.
Disclosures:
Trevor McCracken indicated no relevant financial relationships.
Erica Duh indicated no relevant financial relationships.
Ruby Chien indicated no relevant financial relationships.
Nicholas Garcia indicated no relevant financial relationships.
Marie Balfour indicated no relevant financial relationships.
Momin Masroor indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Peter Nguyen indicated no relevant financial relationships.
Gregory Albers: Nestle Pharmaceuticals – Speakers Bureau.
Trevor McCracken, MD1, Erica Duh, MD2, Ruby Chien, MD3, Nicholas Garcia, MD1, Marie Balfour, MD1, Momin Masroor, MD3, Frances Dang, MD, MSc4, Peter Nguyen, MD3, Gregory Albers, MD, FACG3. P3093 - Hark the Herald Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Irvine Health, Orange, CA; 2University of California Irvine Digestive Health Institute, Orange, CA; 3University of California Irvine, Orange, CA; 4University of California Irvine, Irvine, CA
Introduction: “Hark” in Shakespearean language means to “pay attention” – a relevant term when referring to minor, intermittent “herald” GI bleeds that often precede more major bleeding events. One example is an iliac-artery enteric fistula (IEF), or an abnormal connection between the iliac artery and the GI tract, which can result in massive bleeding.
Case Description/
Methods: A 48-year-old male with dual pancreatic and kidney transplants presented to the emergency department with hematochezia. His hemoglobin was 9.4, and CT imaging revealed mild fat stranding in the pancreas and rectosigmoid colon. He was previously hospitalized five years prior for similar symptoms and had an unremarkable endoscopic evaluation. Given all of this, the ED decided to transfuse one unit of red blood cells before discharging home with close outpatient follow up. Only two weeks later, he presented to the ED again for similar complaints, but this time his hemoglobin was significantly decreased to 5.4. The patient underwent repeat CT imaging which was unrevealing. He was scheduled for a colonoscopy the following day; however, upon starting his bowel prep, he developed hematochezia and eventually hemorrhagic shock. Massive transfusion protocol was activated, and interventional radiology was consulted for emergent angiography which revealed an IEF originating from the proximal right internal iliac artery at the failed pancreatic graft site. An arterial stent was placed successfully with no further evidence of contrast extravasation. Despite this, the patient developed ventricular fibrillation and cardiac arrest secondary to transfusion associated circulatory overload, and his family ultimately decided to transition to comfort measures.
Discussion: IEFs are thought to arise from pressure against the bowel wall by a graft or pseudoaneurysm in conjunction with some degree of infection leading to necrosis and then perforation or fistulization. They occur, albeit rarely, in patients with failed pancreatic transplants. This case highlights the difficulty in identifying arterial-enteric fistulas specifically in dual pancreatic and kidney transplants. While EGD and colonoscopy are the gold standards for evaluating GI bleeds, these procedures often only detect up to 25% of secondary IEFs. We feel this case to be clinically important as it is an example of one of the rarer types of GI bleeds. Let this serve as a poignant reminder to hark the herald GI bleed in patients with pancreatic transplants.
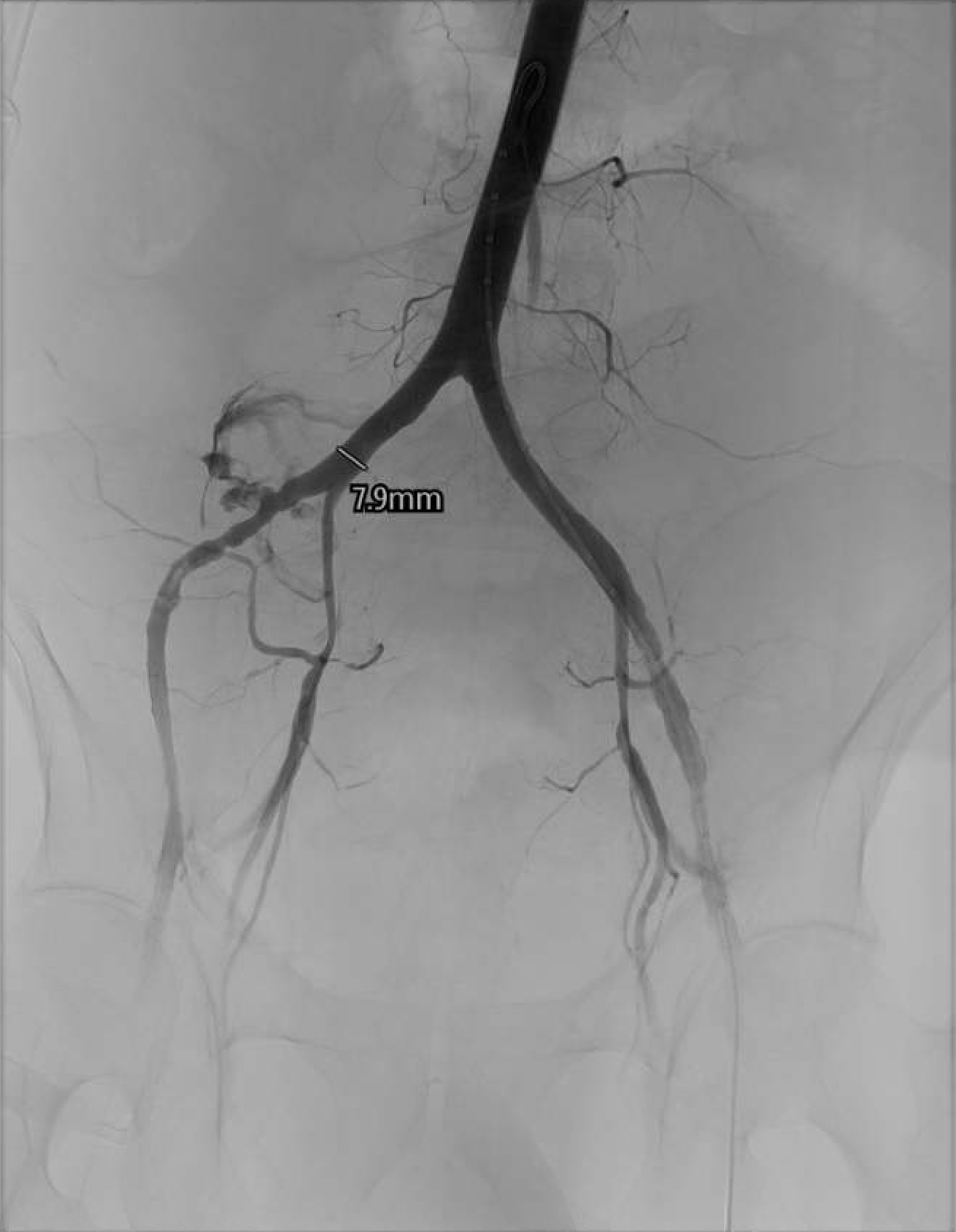
Figure: Figure 1: Angiography demonstrating an injured right internal iliac artery with massive extravasation.
Disclosures:
Trevor McCracken indicated no relevant financial relationships.
Erica Duh indicated no relevant financial relationships.
Ruby Chien indicated no relevant financial relationships.
Nicholas Garcia indicated no relevant financial relationships.
Marie Balfour indicated no relevant financial relationships.
Momin Masroor indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Peter Nguyen indicated no relevant financial relationships.
Gregory Albers: Nestle Pharmaceuticals – Speakers Bureau.
Trevor McCracken, MD1, Erica Duh, MD2, Ruby Chien, MD3, Nicholas Garcia, MD1, Marie Balfour, MD1, Momin Masroor, MD3, Frances Dang, MD, MSc4, Peter Nguyen, MD3, Gregory Albers, MD, FACG3. P3093 - Hark the Herald Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

