Monday Poster Session
Category: GI Bleeding
P3091 - Pseudoaneurysm-Related Gastrointestinal Bleed in Pancreatitis: A Case Series and Diagnostic Challenges
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AB
Ahmad Barazi, MD
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Mutaz Kalas, MD1, Ahmad Barazi, MD1, M. Ammar Kalas, MD1, Eric S.. Tatro, MD1, Akanksha Togra, MD1, Gethin Williams, MD2, Sherif E. Elhanafi, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2University Medical Center of El Paso, El Paso, TX
Introduction: Gastrointestinal (GI) bleeding in the context of pancreatitis is a rare but morbid complication that may be misattributed to other common causes. Herein, we present three cases that emphasize the importance of clinician awareness, early recognition, and accurate diagnosis of visceral artery pseudoaneurysm (PSA) in the setting of pancreatitis.
Case Description/
Methods: Case 1:
A 61-year-old with history of pancreatitis (diagnosed 3 years prior) presented with hematemesis. EGD without evidence of active bleeding. CT with angiography (CTA) revealed necrotizing pancreatitis with a 10 mm PSA in the distal splenic artery (Figure 1A). Angiography revealed multiple PSAs in the middle and lower poles of the splenic artery and IR guided coil embolization was performed (Figure 1B).
Case 2:
A 64-year-old male with history of necrotizing pancreatitis presented with 3 episodes of melena. EGD with blood in the stomach and duodenum. An area of inflammation with a fistulous tract was found in the 1st part of duodenum. CTA revealed aneurysm of the gastroduodenal artery measuring 8 mm. IR performed coil embolization of GDA with cessation of overt bleeding (Figure 1C,1D).
Case 3:
A 45-year-old female with history of pancreatitis (diagnosed one year prior) presented with hematemesis. EGD with blood in the stomach however no source identified. Patient continued with intermittent GI bleed which required 10 units of blood and underwent an exploratory laparotomy. CTA revealed a large PSA of the splenic artery (Figure 1E), IR performed coil embolization with cessation of overt bleeding (Figure 1F).
Discussion: These cases highlight the importance of early recognition of visceral artery PSA as a potential source of gastrointestinal bleeding in the context of necrotizing pancreatitis. Timely identification enables prompt intervention and improves patient outcomes. Notably, the interval between the diagnosis of pancreatitis and the onset of PSA-related bleeding is highly variable, with some cases occurring years after the initial diagnosis. Intraluminal GI bleeding may result from subtle fistulization between a peripancreatic collection and the GI tract, which can present intermittently and pose significant diagnostic challenges.
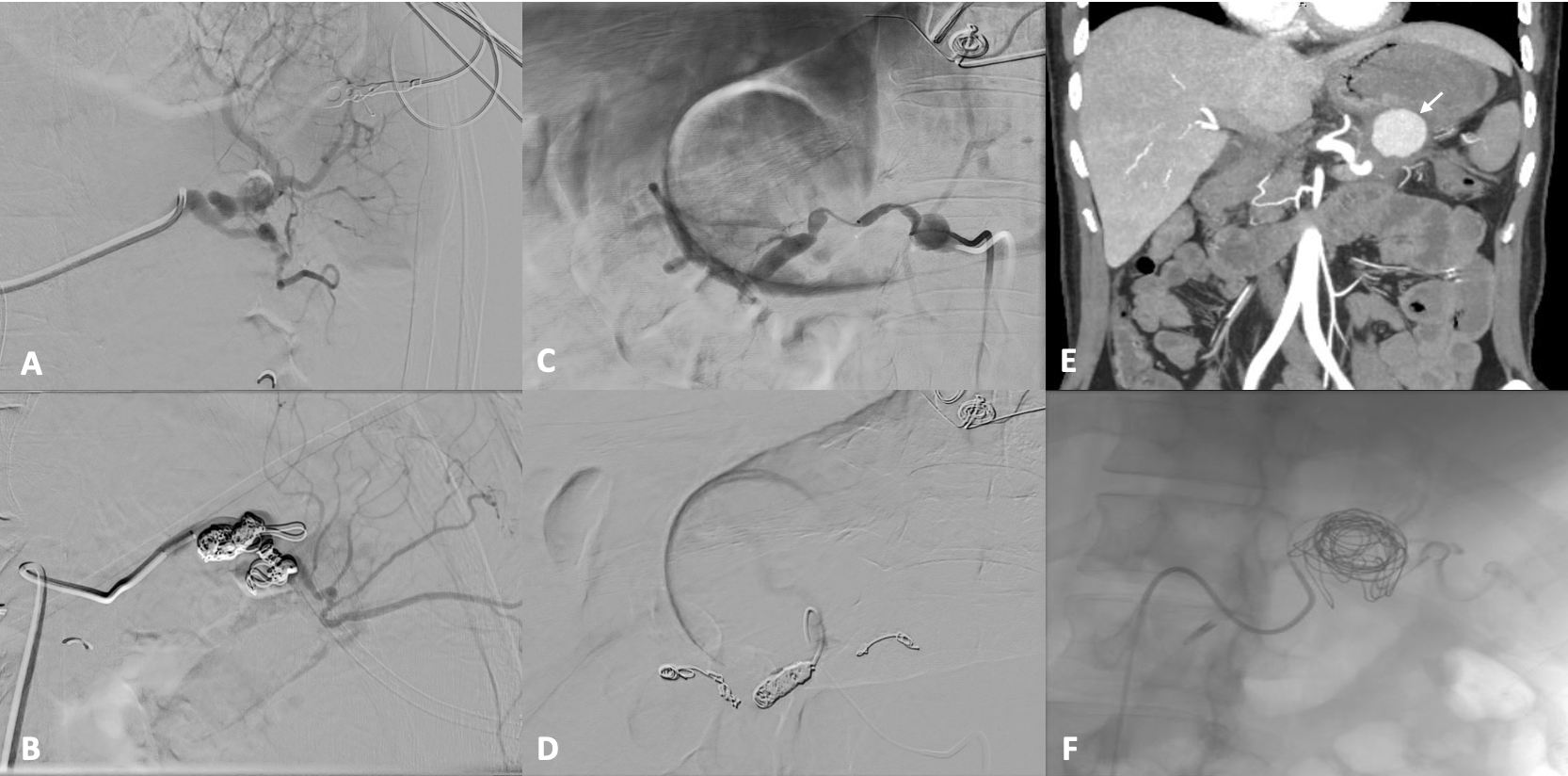
Figure: Figure 1A-F:
A: Case 1 pre-embolization angiogram, B: Case 1 post-embolization angiogram, C: Case 2 pre-embolization angiogram, D: Case 2 post-embolization angiogram, E: Case 3 pre-embolization CTA showing pseudoaneurysm (white arrow) in the splenic artery, F: Case 3 post-embolization angiogram
Disclosures:
Mutaz Kalas indicated no relevant financial relationships.
Ahmad Barazi indicated no relevant financial relationships.
M. Ammar Kalas indicated no relevant financial relationships.
Eric Tatro indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Gethin Williams indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Mutaz Kalas, MD1, Ahmad Barazi, MD1, M. Ammar Kalas, MD1, Eric S.. Tatro, MD1, Akanksha Togra, MD1, Gethin Williams, MD2, Sherif E. Elhanafi, MD1. P3091 - Pseudoaneurysm-Related Gastrointestinal Bleed in Pancreatitis: A Case Series and Diagnostic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, TX; 2University Medical Center of El Paso, El Paso, TX
Introduction: Gastrointestinal (GI) bleeding in the context of pancreatitis is a rare but morbid complication that may be misattributed to other common causes. Herein, we present three cases that emphasize the importance of clinician awareness, early recognition, and accurate diagnosis of visceral artery pseudoaneurysm (PSA) in the setting of pancreatitis.
Case Description/
Methods: Case 1:
A 61-year-old with history of pancreatitis (diagnosed 3 years prior) presented with hematemesis. EGD without evidence of active bleeding. CT with angiography (CTA) revealed necrotizing pancreatitis with a 10 mm PSA in the distal splenic artery (Figure 1A). Angiography revealed multiple PSAs in the middle and lower poles of the splenic artery and IR guided coil embolization was performed (Figure 1B).
Case 2:
A 64-year-old male with history of necrotizing pancreatitis presented with 3 episodes of melena. EGD with blood in the stomach and duodenum. An area of inflammation with a fistulous tract was found in the 1st part of duodenum. CTA revealed aneurysm of the gastroduodenal artery measuring 8 mm. IR performed coil embolization of GDA with cessation of overt bleeding (Figure 1C,1D).
Case 3:
A 45-year-old female with history of pancreatitis (diagnosed one year prior) presented with hematemesis. EGD with blood in the stomach however no source identified. Patient continued with intermittent GI bleed which required 10 units of blood and underwent an exploratory laparotomy. CTA revealed a large PSA of the splenic artery (Figure 1E), IR performed coil embolization with cessation of overt bleeding (Figure 1F).
Discussion: These cases highlight the importance of early recognition of visceral artery PSA as a potential source of gastrointestinal bleeding in the context of necrotizing pancreatitis. Timely identification enables prompt intervention and improves patient outcomes. Notably, the interval between the diagnosis of pancreatitis and the onset of PSA-related bleeding is highly variable, with some cases occurring years after the initial diagnosis. Intraluminal GI bleeding may result from subtle fistulization between a peripancreatic collection and the GI tract, which can present intermittently and pose significant diagnostic challenges.
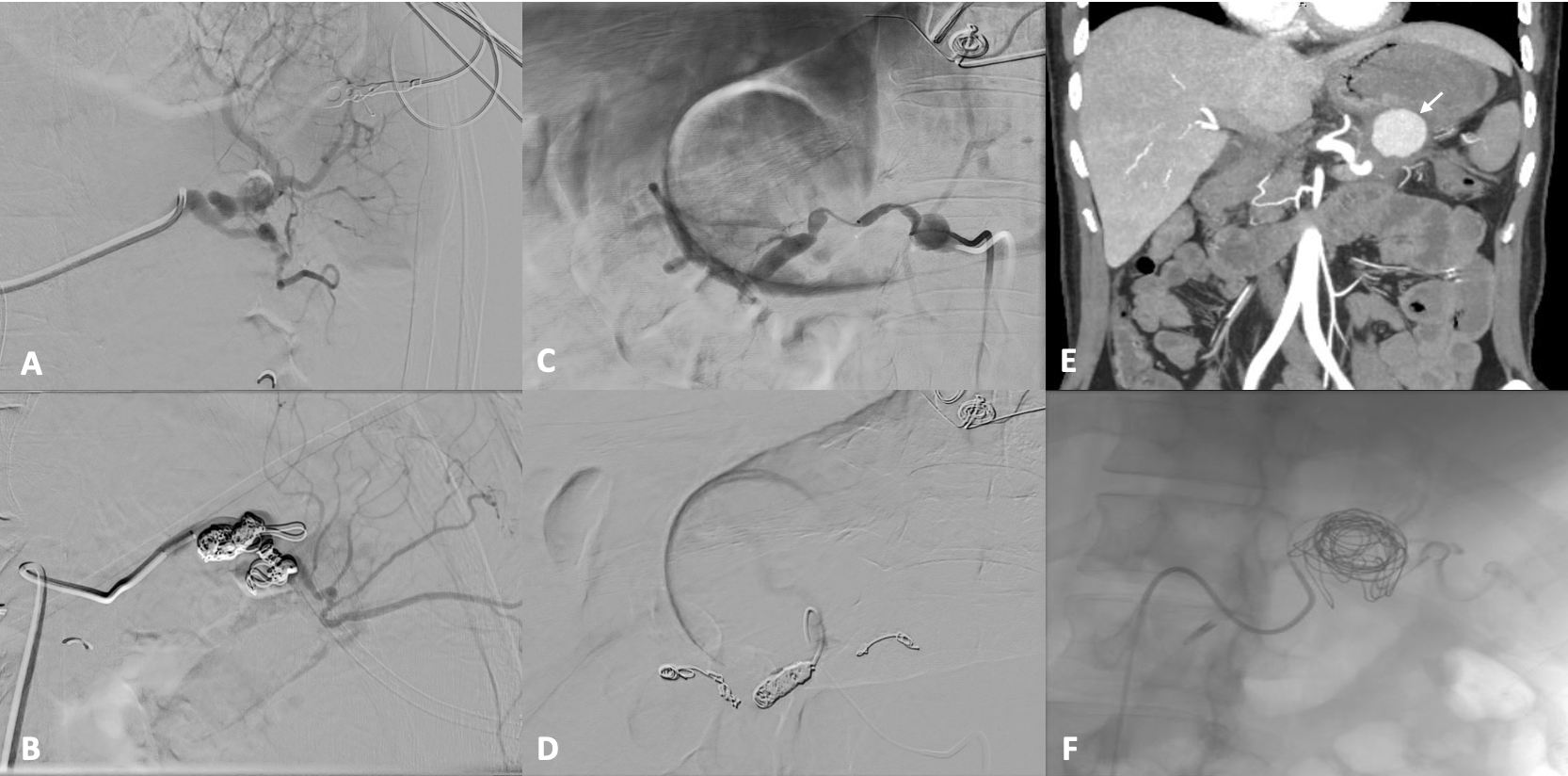
Figure: Figure 1A-F:
A: Case 1 pre-embolization angiogram, B: Case 1 post-embolization angiogram, C: Case 2 pre-embolization angiogram, D: Case 2 post-embolization angiogram, E: Case 3 pre-embolization CTA showing pseudoaneurysm (white arrow) in the splenic artery, F: Case 3 post-embolization angiogram
Disclosures:
Mutaz Kalas indicated no relevant financial relationships.
Ahmad Barazi indicated no relevant financial relationships.
M. Ammar Kalas indicated no relevant financial relationships.
Eric Tatro indicated no relevant financial relationships.
Akanksha Togra indicated no relevant financial relationships.
Gethin Williams indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Mutaz Kalas, MD1, Ahmad Barazi, MD1, M. Ammar Kalas, MD1, Eric S.. Tatro, MD1, Akanksha Togra, MD1, Gethin Williams, MD2, Sherif E. Elhanafi, MD1. P3091 - Pseudoaneurysm-Related Gastrointestinal Bleed in Pancreatitis: A Case Series and Diagnostic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
