Monday Poster Session
Category: GI Bleeding
P3090 - Bleeding From the Shadows: Hidden Angiodysplasia Within a Duodenal Diverticulum
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MT
Mehul Trivedi, MD
University of Utah Health
Salt Lake City, UT
Presenting Author(s)
Mehul Trivedi, MD1, Mina Awadallah, MD, MSc2, John Erikson Yap, MD, MBA, FACG1
1University of Utah Health, Salt Lake City, UT; 2University of Utah, Salt Lake City, UT
Introduction: Duodenal diverticula are often incidental findings and rarely implicated as sources of gastrointestinal bleeding. Even more uncommon is the presence of angiodysplasia within these diverticula. We report a case illustrating this unusual source of hemorrhage.
Case Description/
Methods: A 68-year-old man with metastatic melanoma (liver, lung, and splenic metastases) and iron deficiency anemia presented with melena and severe anemia. One week prior, he received two units of packed red blood cells (PRBCs) for a hemoglobin of 6.6 g/dL (baseline 7–8 g/dL) and was discharged with a hemoglobin of 8.7 g/dL after a negative bidirectional endoscopy. He experienced a recurrence of melena two days prior to this admission, with multiple episodes the following day prompting emergency evaluation. On presentation, his hemoglobin was 4.6 g/dL. He was hemodynamically stable and received two units of PRBCs and IV pantoprazole. Upper endoscopy revealed a normal esophagus and diffusely atrophic gastric mucosa without active bleeding. In the second portion of the duodenum, a 40-mm diverticulum was noted. Careful endoscopic inspection revealed a 5-mm angiodysplasia within the diverticulum, displaying typical arborization. Argon plasma coagulation (APC) was performed to treat the lesion. Active oozing was noted during therapy, and hemostasis was achieved at the end of treatment. The patient remained stable post-procedure with no recurrent bleeding and was discharged in good condition.
Discussion: This case demonstrates an unusual and easily missed source of upper gastrointestinal bleeding: an angiodysplasia located within a duodenal diverticulum. Duodenal diverticula are relatively uncommon, reported in approximately 5–22% of autopsy and imaging series, but are infrequently implicated in GI bleeding. Even more rarely, vascular malformations such as angiodysplasia that arise within them. Endoscopists can be wary of investigating within diverticula due to concern for perforating the relatively weaker walls. However, this case illustrates the importance of endoscopically evaluating duodenal diverticula when no other bleeding source is found, as significant pathology can hide within. Recognizing these rare but treatable lesions can prevent ongoing bleeding, reduce transfusion needs, and improve patient outcomes.
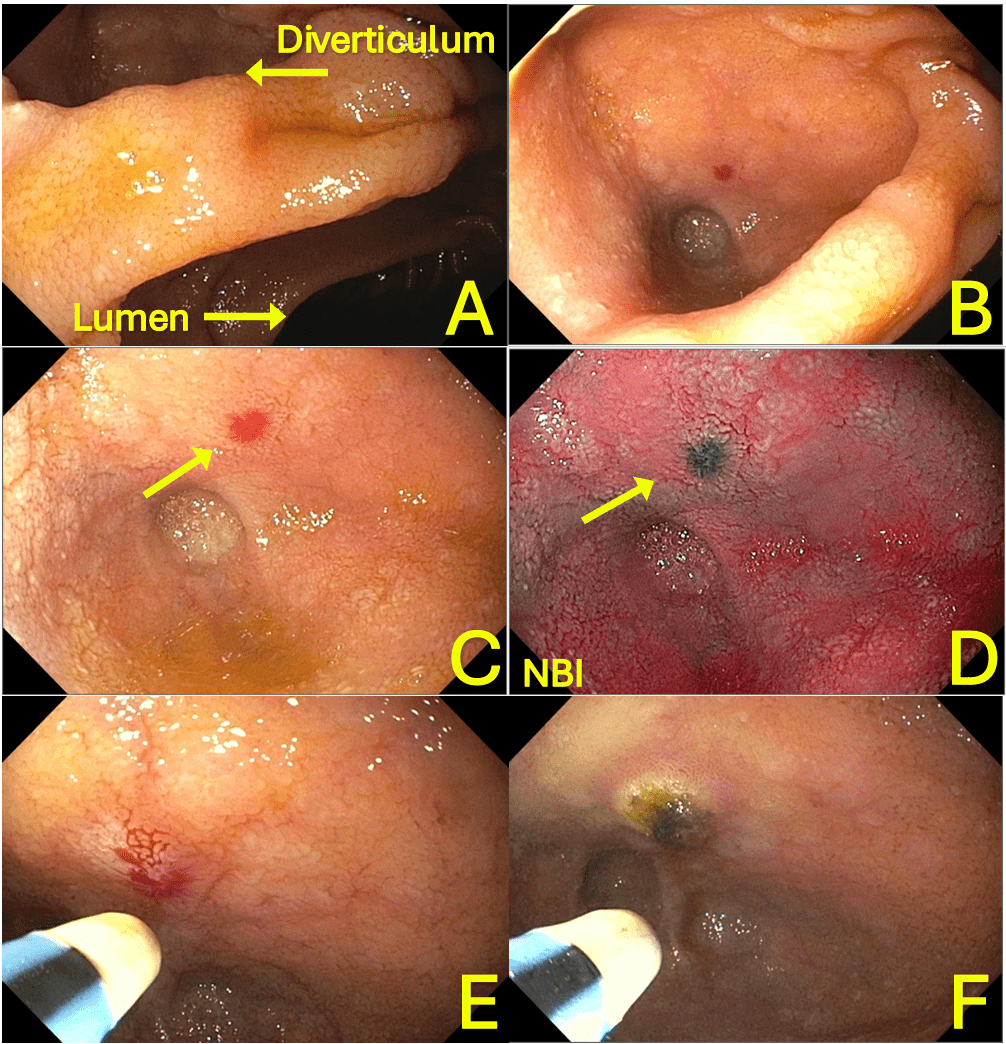
Figure: A. Endoscopic view showing a duodenal diverticulum at the edge of the image, with the duodenal lumen seen on the opposite side.
B. Close-up endoscopic image of the duodenal diverticulum.
C. Angiodysplasia visualized within the diverticulum using white light imaging.
D. Narrow-band imaging (NBI) highlighting angiodysplasia inside the diverticulum.
E. Argon plasma coagulation (APC) of the angiodysplasia with visible mild oozing.
F. Post-treatment image showing complete coagulation of the angiodysplasia.
Disclosures:
Mehul Trivedi indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mehul Trivedi, MD1, Mina Awadallah, MD, MSc2, John Erikson Yap, MD, MBA, FACG1. P3090 - Bleeding From the Shadows: Hidden Angiodysplasia Within a Duodenal Diverticulum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah Health, Salt Lake City, UT; 2University of Utah, Salt Lake City, UT
Introduction: Duodenal diverticula are often incidental findings and rarely implicated as sources of gastrointestinal bleeding. Even more uncommon is the presence of angiodysplasia within these diverticula. We report a case illustrating this unusual source of hemorrhage.
Case Description/
Methods: A 68-year-old man with metastatic melanoma (liver, lung, and splenic metastases) and iron deficiency anemia presented with melena and severe anemia. One week prior, he received two units of packed red blood cells (PRBCs) for a hemoglobin of 6.6 g/dL (baseline 7–8 g/dL) and was discharged with a hemoglobin of 8.7 g/dL after a negative bidirectional endoscopy. He experienced a recurrence of melena two days prior to this admission, with multiple episodes the following day prompting emergency evaluation. On presentation, his hemoglobin was 4.6 g/dL. He was hemodynamically stable and received two units of PRBCs and IV pantoprazole. Upper endoscopy revealed a normal esophagus and diffusely atrophic gastric mucosa without active bleeding. In the second portion of the duodenum, a 40-mm diverticulum was noted. Careful endoscopic inspection revealed a 5-mm angiodysplasia within the diverticulum, displaying typical arborization. Argon plasma coagulation (APC) was performed to treat the lesion. Active oozing was noted during therapy, and hemostasis was achieved at the end of treatment. The patient remained stable post-procedure with no recurrent bleeding and was discharged in good condition.
Discussion: This case demonstrates an unusual and easily missed source of upper gastrointestinal bleeding: an angiodysplasia located within a duodenal diverticulum. Duodenal diverticula are relatively uncommon, reported in approximately 5–22% of autopsy and imaging series, but are infrequently implicated in GI bleeding. Even more rarely, vascular malformations such as angiodysplasia that arise within them. Endoscopists can be wary of investigating within diverticula due to concern for perforating the relatively weaker walls. However, this case illustrates the importance of endoscopically evaluating duodenal diverticula when no other bleeding source is found, as significant pathology can hide within. Recognizing these rare but treatable lesions can prevent ongoing bleeding, reduce transfusion needs, and improve patient outcomes.
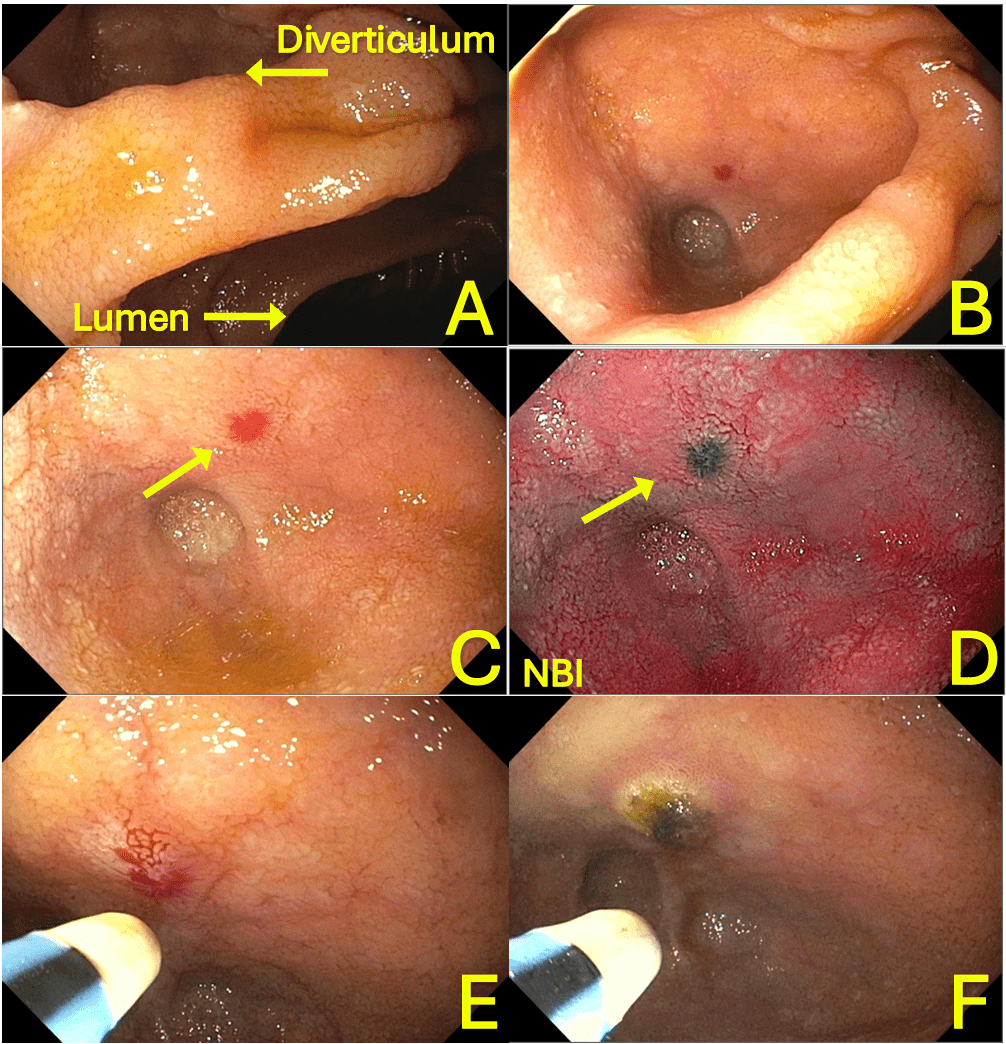
Figure: A. Endoscopic view showing a duodenal diverticulum at the edge of the image, with the duodenal lumen seen on the opposite side.
B. Close-up endoscopic image of the duodenal diverticulum.
C. Angiodysplasia visualized within the diverticulum using white light imaging.
D. Narrow-band imaging (NBI) highlighting angiodysplasia inside the diverticulum.
E. Argon plasma coagulation (APC) of the angiodysplasia with visible mild oozing.
F. Post-treatment image showing complete coagulation of the angiodysplasia.
Disclosures:
Mehul Trivedi indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mehul Trivedi, MD1, Mina Awadallah, MD, MSc2, John Erikson Yap, MD, MBA, FACG1. P3090 - Bleeding From the Shadows: Hidden Angiodysplasia Within a Duodenal Diverticulum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
