Monday Poster Session
Category: GI Bleeding
P3075 - Non-Variceal Upper Gastrointestinal Bleeding in Solid Organ Transplant Recipients: A Nationwide Comparative Analysis of Outcomes and Predictors of Mortality
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Michael Gianarakis, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
Michael Gianarakis, MD1, Ameen Taufiq, BS2, Sindhu Parupalli, MD1, Elie Ghoulam, MD, MS3, Asim Shuja, MD4
1University of Illinois at Chicago, Chicago, IL; 2Kansas City University, Jacksonville, FL; 3Quincy Medical Group, Quincy, IL; 4University of Illinois Chicago, Chicago, IL
Introduction: Non-variceal upper gastrointestinal bleeding (NVUGIB) is a serious complication following solid organ transplant (SOT), particularly in renal transplant (RTx) recipients. SOT patients may be at increased risk due to immunosuppressive medication–related peptic ulcers and surgical complications. Graft rejection has also been implicated as a bleeding risk factor. However, data on NVUGIB in SOT recipients is limited, mostly to small RTx-focused studies. We present the first nationwide study of characteristics, outcomes, and mortality predictors in SOT patients hospitalized with NVUGIB.
Methods: We analyzed the Nationwide Inpatient Sample (2016–2020), identifying adult patients hospitalized with NVUGIB and stratifying by SOT status. Primary outcomes included mortality and complications; secondary outcomes included predictors of all-cause mortality in the SOT group. Multivariate regression models adjusted for confounders and hospital characteristics.
Results: A total of 2,063,585 weighted hospitalizations were included, with 18,945 (0.92%) having a history of SOT, of whom 61.9% were RTx recipients. Aspirin (ASA) and anticoagulant use rates were similar between SOT and non-SOT cohorts. SOT patients had longer hospital stays (11.6 vs. 6.5 days, p< 0.001), higher healthcare costs, and delayed esophagogastroduodenoscopy (EGD) (4.9 vs. 2.5 days, p< 0.001). Mortality in SOT patients was associated with older age (aOR 1.026, p< 0.001), malnutrition (aOR 2.004, p< 0.001), HSV infection (aOR 7.147, p< 0.05), thrombocytopenia (aOR 1.506, p< 0.05), and transplant rejection (aOR 1.967, p< 0.001). RTx (aOR 0.591, p=0.01) and pancreas transplant (PTx) (aOR 0.235, p< 0.05) were associated with lower mortality compared to liver transplant (LTx). ASA use (aOR 0.505, p< 0.05) and EGD during hospitalization (aOR 0.554, p< 0.001) were associated with reduced mortality.
Discussion: This study highlights increased mortality risk in SOT patients with NVUGIB. LTx recipients had the highest mortality, potentially due to surgical anastomotic bleeding, high rejection rates, and thrombocytopenia from residual hypersplenism. ASA use may reduce mortality via prevention of graft-related complications such as rejection or vascular thrombosis. Further research is needed to explore transplant-specific risk factors and the role of immunosuppressive regimens in NVUGIB outcomes.
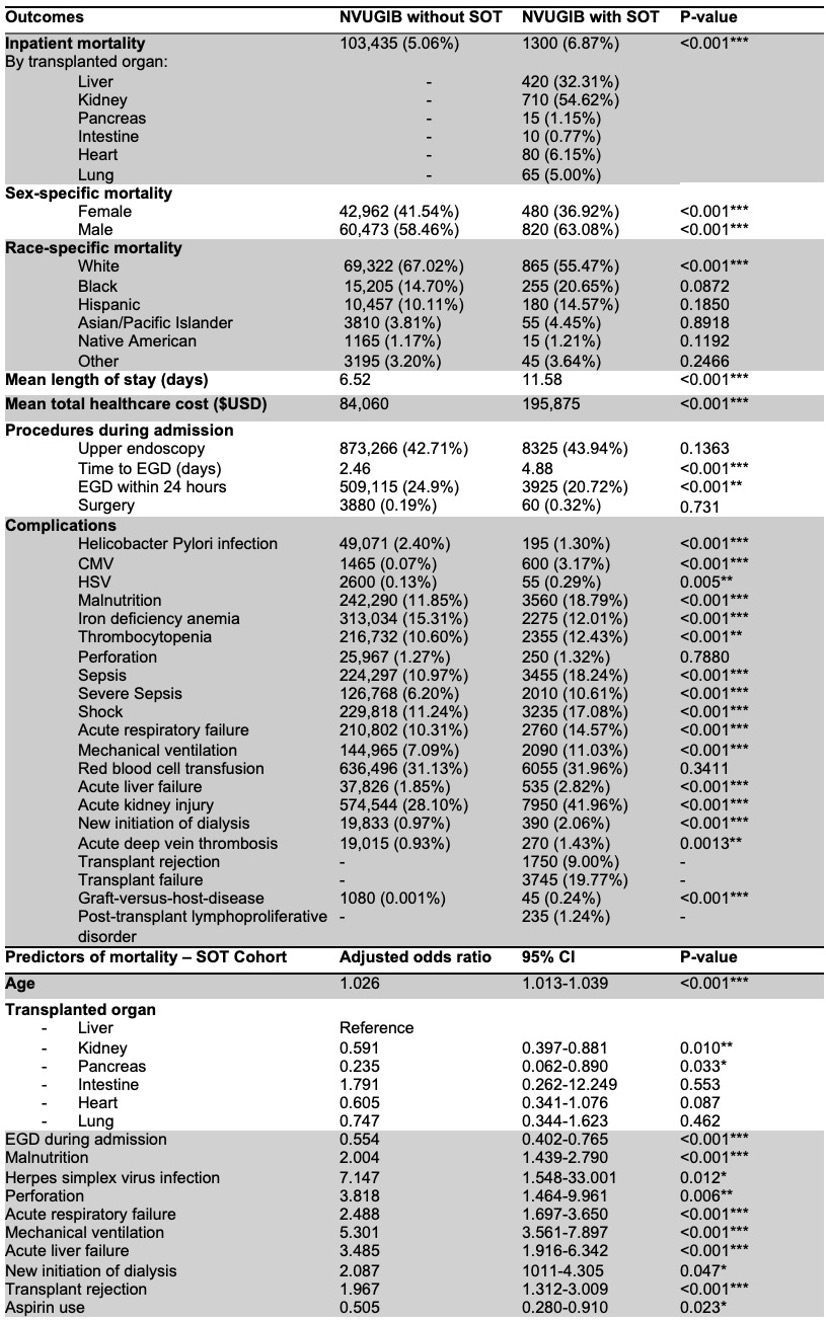
Figure: Table 1: Comparison of demographics, hospital characteristics, comorbidities, hospitalization characteristics in patients hospitalized with NVUGIB with and without history of solid organ transplant (SOT).
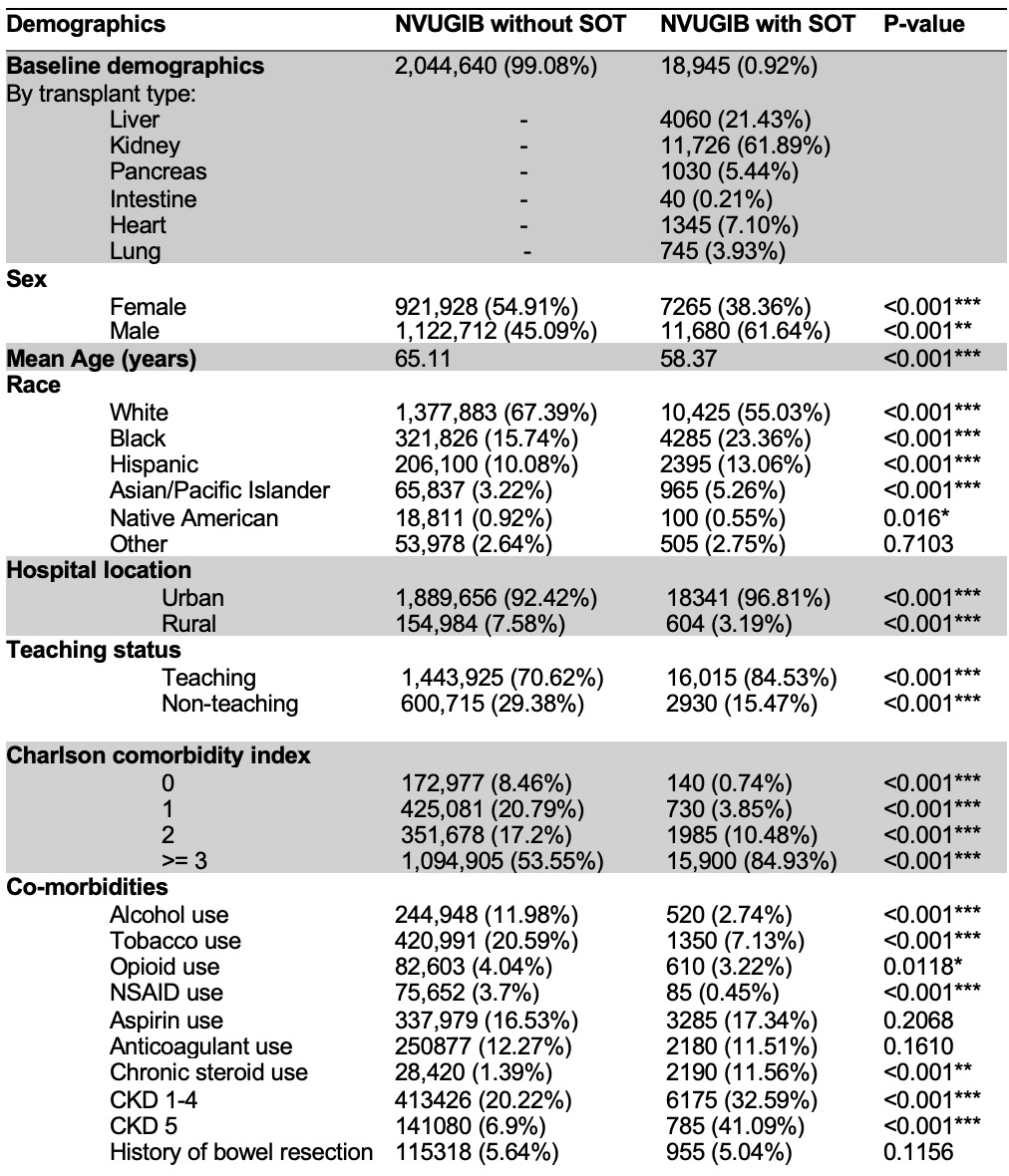
Figure: Table 2: Comparison of clinical outcomes in patients with NVUGIB with and without history of solid organ transplant (SOT) and multivariate logistic regression analysis of predictors of all-cause mortality in patients hospitalized with NVUGIB and history of SOT.
Disclosures:
Michael Gianarakis indicated no relevant financial relationships.
Ameen Taufiq indicated no relevant financial relationships.
Sindhu Parupalli indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
Michael Gianarakis, MD1, Ameen Taufiq, BS2, Sindhu Parupalli, MD1, Elie Ghoulam, MD, MS3, Asim Shuja, MD4. P3075 - Non-Variceal Upper Gastrointestinal Bleeding in Solid Organ Transplant Recipients: A Nationwide Comparative Analysis of Outcomes and Predictors of Mortality, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois at Chicago, Chicago, IL; 2Kansas City University, Jacksonville, FL; 3Quincy Medical Group, Quincy, IL; 4University of Illinois Chicago, Chicago, IL
Introduction: Non-variceal upper gastrointestinal bleeding (NVUGIB) is a serious complication following solid organ transplant (SOT), particularly in renal transplant (RTx) recipients. SOT patients may be at increased risk due to immunosuppressive medication–related peptic ulcers and surgical complications. Graft rejection has also been implicated as a bleeding risk factor. However, data on NVUGIB in SOT recipients is limited, mostly to small RTx-focused studies. We present the first nationwide study of characteristics, outcomes, and mortality predictors in SOT patients hospitalized with NVUGIB.
Methods: We analyzed the Nationwide Inpatient Sample (2016–2020), identifying adult patients hospitalized with NVUGIB and stratifying by SOT status. Primary outcomes included mortality and complications; secondary outcomes included predictors of all-cause mortality in the SOT group. Multivariate regression models adjusted for confounders and hospital characteristics.
Results: A total of 2,063,585 weighted hospitalizations were included, with 18,945 (0.92%) having a history of SOT, of whom 61.9% were RTx recipients. Aspirin (ASA) and anticoagulant use rates were similar between SOT and non-SOT cohorts. SOT patients had longer hospital stays (11.6 vs. 6.5 days, p< 0.001), higher healthcare costs, and delayed esophagogastroduodenoscopy (EGD) (4.9 vs. 2.5 days, p< 0.001). Mortality in SOT patients was associated with older age (aOR 1.026, p< 0.001), malnutrition (aOR 2.004, p< 0.001), HSV infection (aOR 7.147, p< 0.05), thrombocytopenia (aOR 1.506, p< 0.05), and transplant rejection (aOR 1.967, p< 0.001). RTx (aOR 0.591, p=0.01) and pancreas transplant (PTx) (aOR 0.235, p< 0.05) were associated with lower mortality compared to liver transplant (LTx). ASA use (aOR 0.505, p< 0.05) and EGD during hospitalization (aOR 0.554, p< 0.001) were associated with reduced mortality.
Discussion: This study highlights increased mortality risk in SOT patients with NVUGIB. LTx recipients had the highest mortality, potentially due to surgical anastomotic bleeding, high rejection rates, and thrombocytopenia from residual hypersplenism. ASA use may reduce mortality via prevention of graft-related complications such as rejection or vascular thrombosis. Further research is needed to explore transplant-specific risk factors and the role of immunosuppressive regimens in NVUGIB outcomes.
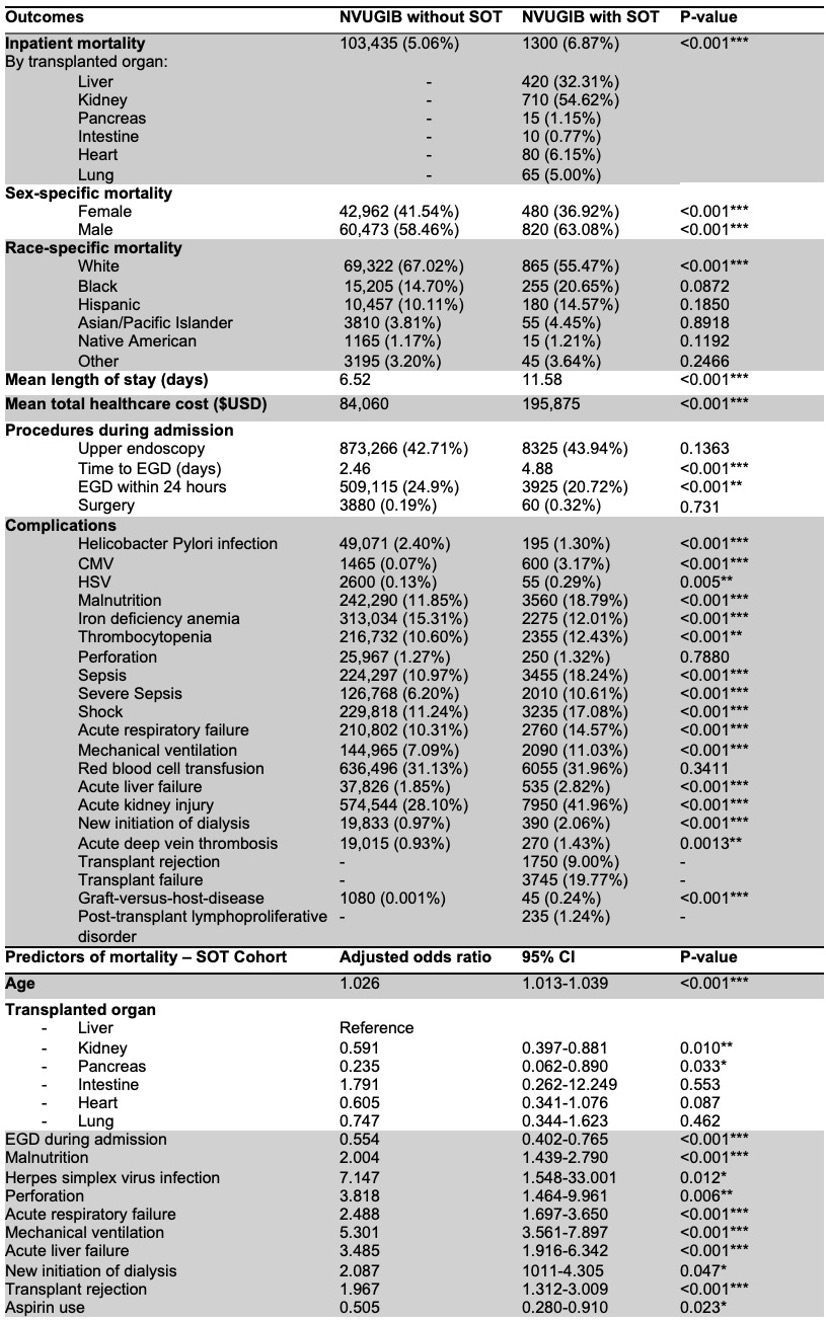
Figure: Table 1: Comparison of demographics, hospital characteristics, comorbidities, hospitalization characteristics in patients hospitalized with NVUGIB with and without history of solid organ transplant (SOT).
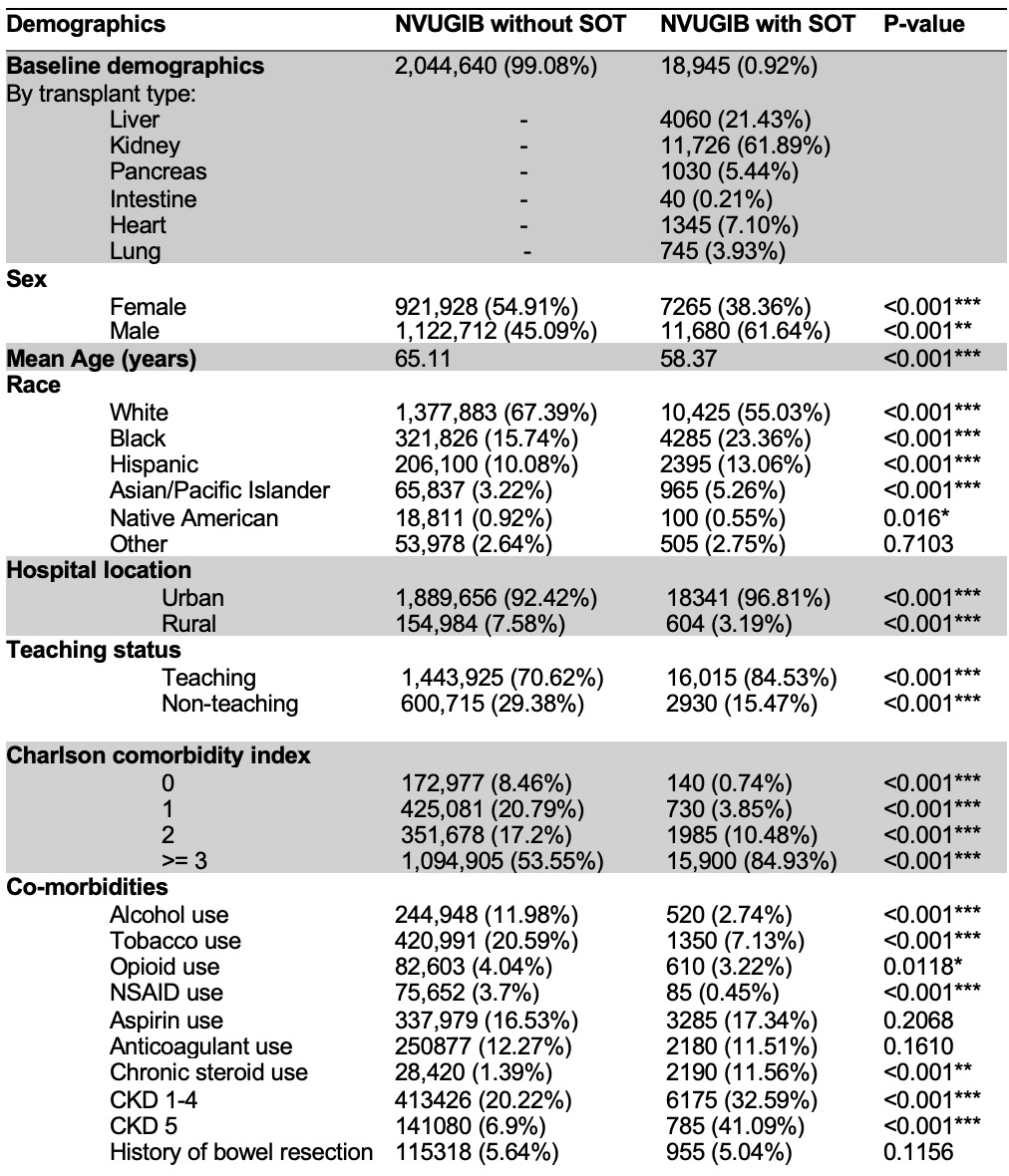
Figure: Table 2: Comparison of clinical outcomes in patients with NVUGIB with and without history of solid organ transplant (SOT) and multivariate logistic regression analysis of predictors of all-cause mortality in patients hospitalized with NVUGIB and history of SOT.
Disclosures:
Michael Gianarakis indicated no relevant financial relationships.
Ameen Taufiq indicated no relevant financial relationships.
Sindhu Parupalli indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
Michael Gianarakis, MD1, Ameen Taufiq, BS2, Sindhu Parupalli, MD1, Elie Ghoulam, MD, MS3, Asim Shuja, MD4. P3075 - Non-Variceal Upper Gastrointestinal Bleeding in Solid Organ Transplant Recipients: A Nationwide Comparative Analysis of Outcomes and Predictors of Mortality, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
