Monday Poster Session
Category: General Endoscopy
A Rare Case of BCL2-Negative Duodenal-Type Follicular Lymphoma Unmasked After <i>H. pylori</i> Eradication
P3042 - A Rare Case of BCL2-Negative Duodenal-Type Follicular Lymphoma Unmasked After H. pylori Eradication
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lakshmi Chirumamilla, MD (she/her/hers)
Howard University Hospital
Washington, DC
Presenting Author(s)
Lakshmi Chirumamilla, MD, Sneha Rao Adidam, MD, Nakul Ganju, MD, Ahmed Mohamed Ebeid, MD, Pinky Bai, MD, Abay Gobezie, MD, Juan C. Santiago-Gonzalez, MD, MSc, Angesom Kibreab, MD
Howard University Hospital, Washington, DC
Introduction: Duodenal Type Follicular Lymphoma (DTFL), a rare variant of follicular lymphoma (FL) that primarily involves the duodenum. It typically presents as incidental finding during endoscopy for unrelated indications. We present a unique case of BCL2-negative DTFL identified on surveillance endoscopy following treatment for H. pylori–associated lymphoid hyperplasia.
Case Description/
Methods: A 76-year-old female with medical history of developmental disability, diabetes and hypertension presented to the gastroenterology clinic with complaints of abdominal pain and unintentional weight loss with no significant prior gastrointestinal history. A screening colonoscopy performed 3-years earlier was unremarkable except for nonbleeding hemorrhoids.
Esophagogastroduodenoscopy (EGD) was performed, revealing diffuse nodularity of both the gastric and duodenal mucosa (Fig 1). Biopsies demonstrated H. pylori positive lymphoid hyperplasia with low mitotic activity, initially considered of uncertain clinical significance. She was treated with standard quadruple therapy for H. Pylori eradication and advised to return for follow-up in 3 to 6 months.
Repeat EGD 5-months later showed persistent duodenal nodularity (Fig 2). Biopsies at that time demonstrated a well-formed lymphoid follicle with immunohistochemical staining positive for CD20, CD10, and BCL6. Fluorescence in situ hybridization analysis (FISH) did not reveal the BCL2 gene rearrangement t(14;18). H. pylori testing was negative. Based on pathology findings (fig 3), diagnosis of BCL2-negative DTFL was made.The patient was offered management options, which includes rituximab-based immunotherapy versus conservative monitoring. Patient opted for active surveillance given the indolent nature and her stable condition.
Discussion: DTFL is a rare extranodal subtype of FL that typically presents as mucosal nodularity or small polyps on endoscopy, necessitating biopsy for diagnosis. While H. pylori play a pathogenic role in gastric MALT lymphoma, its role in DTFL is unclear. In this case, concurrent H. pylori infection and duodenal lymphoid proliferation contributed to initial diagnostic ambiguity. Most FLs harbor the t (14;18) translocation leading to BCL2 overexpression; cases lacking this hallmark are exceedingly rare and pose diagnostic and therapeutic challenges. This case highlights the importance of follow-up endoscopy and histopathological re-evaluation of persistent duodenal lymphoid lesions, especially in the context of H. pylori infection.
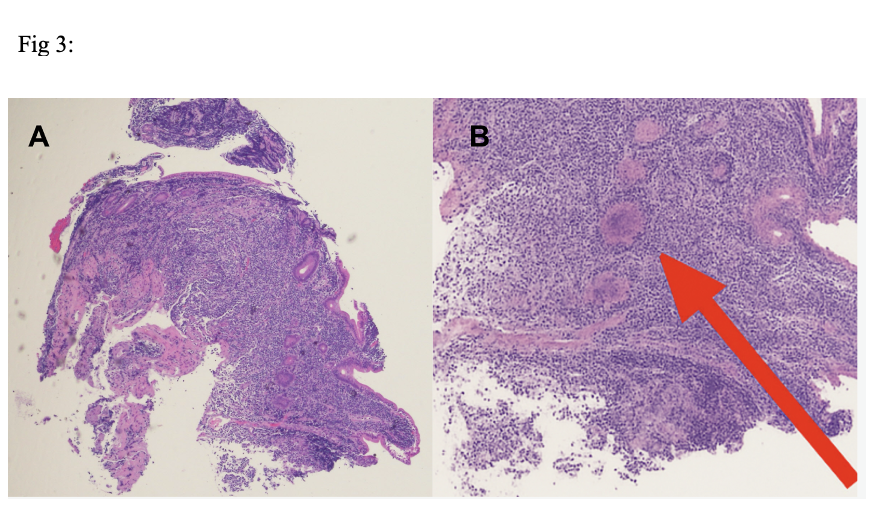
Figure: Fig 1a, 1b. Second portion of the duodenum characterized by granularity, nodularity, white specks and ulceration seen. Fig 2. Second portion of the duodenum with lymphangiectasia.
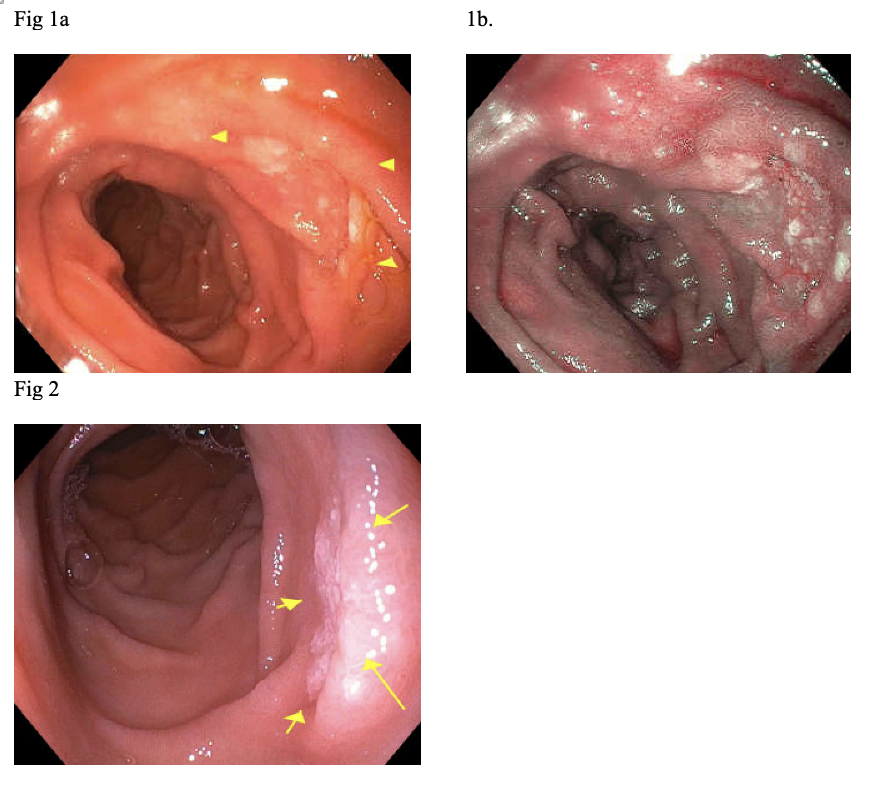
Figure: Histopathologic features of duodenal-type follicular lymphoma. (A) Low-power H&E-stained section of duodenal mucosa demonstrating multiple well-formed lymphoid follicles within the lamina propria. (B) Higher magnification of the same region highlighting neoplastic lymphoid follicles (red arrow).
Disclosures:
Lakshmi Chirumamilla indicated no relevant financial relationships.
Sneha Rao Adidam indicated no relevant financial relationships.
Nakul Ganju indicated no relevant financial relationships.
Ahmed Mohamed Ebeid indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Abay Gobezie indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Lakshmi Chirumamilla, MD, Sneha Rao Adidam, MD, Nakul Ganju, MD, Ahmed Mohamed Ebeid, MD, Pinky Bai, MD, Abay Gobezie, MD, Juan C. Santiago-Gonzalez, MD, MSc, Angesom Kibreab, MD. P3042 - A Rare Case of BCL2-Negative Duodenal-Type Follicular Lymphoma Unmasked After <i>H. pylori</i> Eradication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Howard University Hospital, Washington, DC
Introduction: Duodenal Type Follicular Lymphoma (DTFL), a rare variant of follicular lymphoma (FL) that primarily involves the duodenum. It typically presents as incidental finding during endoscopy for unrelated indications. We present a unique case of BCL2-negative DTFL identified on surveillance endoscopy following treatment for H. pylori–associated lymphoid hyperplasia.
Case Description/
Methods: A 76-year-old female with medical history of developmental disability, diabetes and hypertension presented to the gastroenterology clinic with complaints of abdominal pain and unintentional weight loss with no significant prior gastrointestinal history. A screening colonoscopy performed 3-years earlier was unremarkable except for nonbleeding hemorrhoids.
Esophagogastroduodenoscopy (EGD) was performed, revealing diffuse nodularity of both the gastric and duodenal mucosa (Fig 1). Biopsies demonstrated H. pylori positive lymphoid hyperplasia with low mitotic activity, initially considered of uncertain clinical significance. She was treated with standard quadruple therapy for H. Pylori eradication and advised to return for follow-up in 3 to 6 months.
Repeat EGD 5-months later showed persistent duodenal nodularity (Fig 2). Biopsies at that time demonstrated a well-formed lymphoid follicle with immunohistochemical staining positive for CD20, CD10, and BCL6. Fluorescence in situ hybridization analysis (FISH) did not reveal the BCL2 gene rearrangement t(14;18). H. pylori testing was negative. Based on pathology findings (fig 3), diagnosis of BCL2-negative DTFL was made.The patient was offered management options, which includes rituximab-based immunotherapy versus conservative monitoring. Patient opted for active surveillance given the indolent nature and her stable condition.
Discussion: DTFL is a rare extranodal subtype of FL that typically presents as mucosal nodularity or small polyps on endoscopy, necessitating biopsy for diagnosis. While H. pylori play a pathogenic role in gastric MALT lymphoma, its role in DTFL is unclear. In this case, concurrent H. pylori infection and duodenal lymphoid proliferation contributed to initial diagnostic ambiguity. Most FLs harbor the t (14;18) translocation leading to BCL2 overexpression; cases lacking this hallmark are exceedingly rare and pose diagnostic and therapeutic challenges. This case highlights the importance of follow-up endoscopy and histopathological re-evaluation of persistent duodenal lymphoid lesions, especially in the context of H. pylori infection.
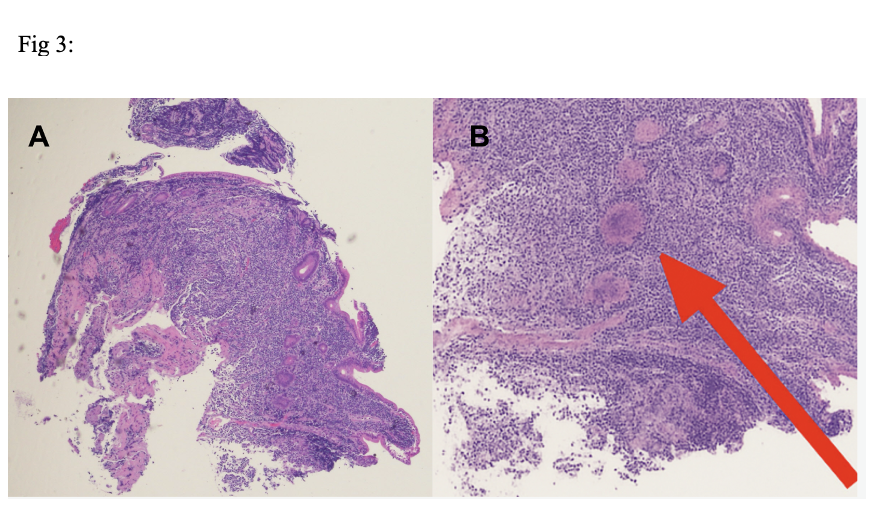
Figure: Fig 1a, 1b. Second portion of the duodenum characterized by granularity, nodularity, white specks and ulceration seen. Fig 2. Second portion of the duodenum with lymphangiectasia.
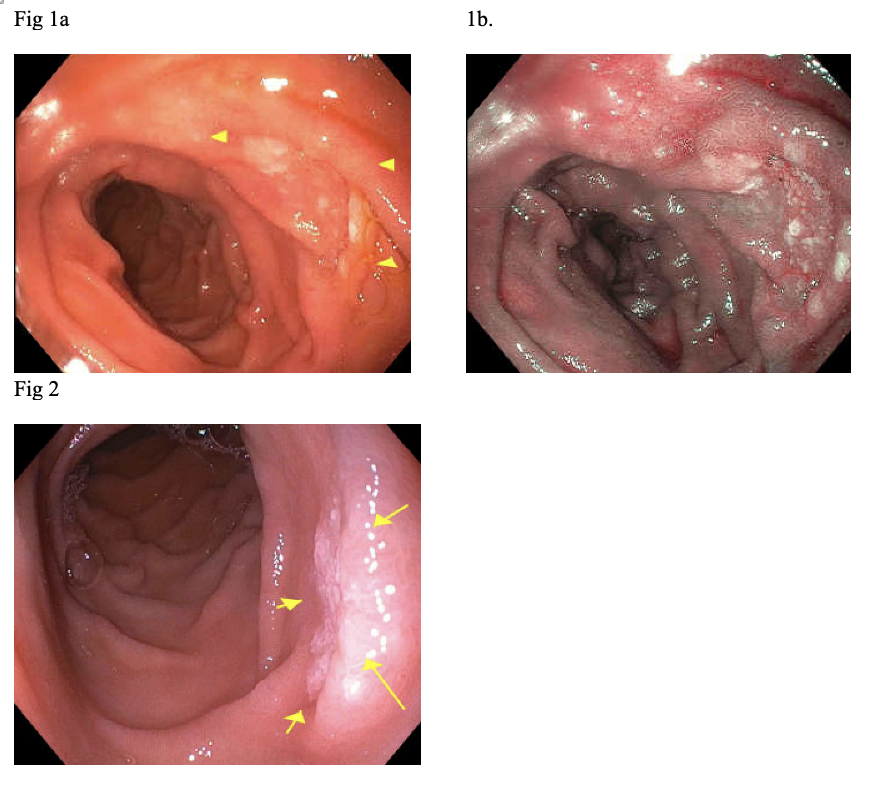
Figure: Histopathologic features of duodenal-type follicular lymphoma. (A) Low-power H&E-stained section of duodenal mucosa demonstrating multiple well-formed lymphoid follicles within the lamina propria. (B) Higher magnification of the same region highlighting neoplastic lymphoid follicles (red arrow).
Disclosures:
Lakshmi Chirumamilla indicated no relevant financial relationships.
Sneha Rao Adidam indicated no relevant financial relationships.
Nakul Ganju indicated no relevant financial relationships.
Ahmed Mohamed Ebeid indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Abay Gobezie indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Lakshmi Chirumamilla, MD, Sneha Rao Adidam, MD, Nakul Ganju, MD, Ahmed Mohamed Ebeid, MD, Pinky Bai, MD, Abay Gobezie, MD, Juan C. Santiago-Gonzalez, MD, MSc, Angesom Kibreab, MD. P3042 - A Rare Case of BCL2-Negative Duodenal-Type Follicular Lymphoma Unmasked After <i>H. pylori</i> Eradication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
