Monday Poster Session
Category: General Endoscopy
P3012 - A Meshy Situation: A Case of Asymptomatic Late-Onset Colonic Invasion by Hernia Mesh
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Reena Razdan, MD
NewYork-Presbyterian/Queens
Flushing, NY
Presenting Author(s)
Reena Razdan, MD1, Abrahim Mahmood, DO2, Constantine Fisher, MD1
1NewYork-Presbyterian/Queens, Flushing, NY; 2NewYork-Presbyterian/Queens, Greenlawn, NY
Introduction: Mesh migration is a rare complication of inguinal hernia repair with mesh. Here, we describe a case of asymptomatic, late-onset mesh invasion six years after bilateral inguinal hernia repair with prosthetic mesh.
Case Description/
Methods: An 82-year-old male with pertinent medical history of CAD, IBS-M, bilateral inguinal hernia repair 6 years prior, and adenomatous colon polyps presented to outpatient GI clinic for routine follow up colonoscopy. The patient had no complaints. At outpatient colonoscopy, the patient was found to have a hernia repair mesh in the sigmoid colon, which was biopsied and tattooed distally. Pathology revealed chronic active colitis, negative for dysplasia or granulomas. The patient was advised to seek ED evaluation promptly, but presented 3 days later. CTAP with IV contrast showed extensive colonic diverticulosis, a focal area of wall thickening and peri-colonic fat stranding with indwelling hyperdense material possibly presenting foreign body with no evidence of perforation. Surgical consult advised prompt follow-up with the patient’s outpatient surgeon for elective sigmoidectomy, which was scheduled for 3 days later. The patient was scheduled for flexible sigmoidoscopy 1 week later, where the mesh could not be reached. Approximately 2.5 months after initial colonoscopy, the patient underwent colonoscopy where endoscopic removal of the mesh was unsuccessful and the procedure was then converted to laparoscopic sigmoidectomy with side to end anastomosis. The patient tolerated the procedure well and was discharged home post-op 2 days later. At outpatient follow-up surgery visit the patient only had mild constipation and abdominal discomfort.
Discussion: Late-onset mesh invasion of the Gl tract is rare. There are no clear guidelines on the management of these cases, though review highlights that endoscopic removal is attempted initially, though often unsuccessful. In a literature review of intestinal erosions following inguinal hernia repair, an open primary procedure and bowel resection was more frequent in late presenting cases (occurring >6 months after surgery). Clinical presentation of these cases also varies, including abdominal pain, sepsis, or change in bowel habits. Our clinical case is unique due to the patient’s complete lack of symptoms despite marked bowel invasion by the hernia mesh. Our case highlights a possible complication of hernia repair even years after index surgery, and how clinical presentation may not correlate with incidental colonoscopy findings.
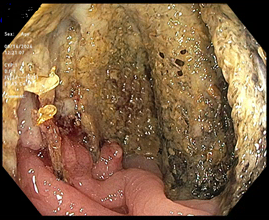
Figure: Foreign body (hernia repair mesh) in the sigmoid colon incidentally found on routine outpatient colonoscopy.

Figure: CT AP with IV contrast showing a focal area of wall thickening in the sigmoid colon and pericolonic fat stranding with indwelling hyperdense material possibly presenting foreign body (hernia mesh).
Disclosures:
Reena Razdan indicated no relevant financial relationships.
Abrahim Mahmood indicated no relevant financial relationships.
Constantine Fisher indicated no relevant financial relationships.
Reena Razdan, MD1, Abrahim Mahmood, DO2, Constantine Fisher, MD1. P3012 - A Meshy Situation: A Case of Asymptomatic Late-Onset Colonic Invasion by Hernia Mesh, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian/Queens, Flushing, NY; 2NewYork-Presbyterian/Queens, Greenlawn, NY
Introduction: Mesh migration is a rare complication of inguinal hernia repair with mesh. Here, we describe a case of asymptomatic, late-onset mesh invasion six years after bilateral inguinal hernia repair with prosthetic mesh.
Case Description/
Methods: An 82-year-old male with pertinent medical history of CAD, IBS-M, bilateral inguinal hernia repair 6 years prior, and adenomatous colon polyps presented to outpatient GI clinic for routine follow up colonoscopy. The patient had no complaints. At outpatient colonoscopy, the patient was found to have a hernia repair mesh in the sigmoid colon, which was biopsied and tattooed distally. Pathology revealed chronic active colitis, negative for dysplasia or granulomas. The patient was advised to seek ED evaluation promptly, but presented 3 days later. CTAP with IV contrast showed extensive colonic diverticulosis, a focal area of wall thickening and peri-colonic fat stranding with indwelling hyperdense material possibly presenting foreign body with no evidence of perforation. Surgical consult advised prompt follow-up with the patient’s outpatient surgeon for elective sigmoidectomy, which was scheduled for 3 days later. The patient was scheduled for flexible sigmoidoscopy 1 week later, where the mesh could not be reached. Approximately 2.5 months after initial colonoscopy, the patient underwent colonoscopy where endoscopic removal of the mesh was unsuccessful and the procedure was then converted to laparoscopic sigmoidectomy with side to end anastomosis. The patient tolerated the procedure well and was discharged home post-op 2 days later. At outpatient follow-up surgery visit the patient only had mild constipation and abdominal discomfort.
Discussion: Late-onset mesh invasion of the Gl tract is rare. There are no clear guidelines on the management of these cases, though review highlights that endoscopic removal is attempted initially, though often unsuccessful. In a literature review of intestinal erosions following inguinal hernia repair, an open primary procedure and bowel resection was more frequent in late presenting cases (occurring >6 months after surgery). Clinical presentation of these cases also varies, including abdominal pain, sepsis, or change in bowel habits. Our clinical case is unique due to the patient’s complete lack of symptoms despite marked bowel invasion by the hernia mesh. Our case highlights a possible complication of hernia repair even years after index surgery, and how clinical presentation may not correlate with incidental colonoscopy findings.
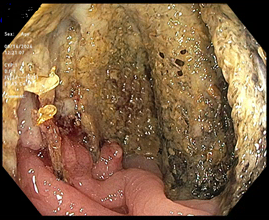
Figure: Foreign body (hernia repair mesh) in the sigmoid colon incidentally found on routine outpatient colonoscopy.

Figure: CT AP with IV contrast showing a focal area of wall thickening in the sigmoid colon and pericolonic fat stranding with indwelling hyperdense material possibly presenting foreign body (hernia mesh).
Disclosures:
Reena Razdan indicated no relevant financial relationships.
Abrahim Mahmood indicated no relevant financial relationships.
Constantine Fisher indicated no relevant financial relationships.
Reena Razdan, MD1, Abrahim Mahmood, DO2, Constantine Fisher, MD1. P3012 - A Meshy Situation: A Case of Asymptomatic Late-Onset Colonic Invasion by Hernia Mesh, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
