Monday Poster Session
Category: General Endoscopy
P3007 - A Case of Upper GI Adenocarcinoma Preceded by Pyoderma Gangrenosum
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- ZF
Zan Ferrin, DO
Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas
Las Vegas, NV
Presenting Author(s)
Zan Ferrin, DO1, Tooba Laeeq, MD2, Yassin Naga, MD2, Yssra Soliman, MD2, Aditi Singh, MD2
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Solid organ malignancies in patients with established Pyoderma Gangrenosum (PG) are rare, and few reported cases have been from an upper GI source. In a recent prospective cohort study in the US, of 356 individuals with PG, 23 patients had solid organ malignancies.1 The exact relationship of PG and malignancy is unknown and current cancer screening guidelines make no adjustment for this population.2 This case highlights the importance of conducting a thorough review of symptoms for patients with PG to improve management.
Case Description/
Methods: A 71 year old male with a recent diagnosis of biopsy proven PG presented for evaluation of a 10-day history of acute progressive dysphagia associated with unintentional weight loss. Labs remarkable for ESR: 32, CRP: 1.84, CEA< 0.5. CT scan upon admission was pertinent for a left hepatic lobe cyst measuring 1.6 x 1.2 cm and a pancreatic tail irregular hypodense lesion. EGD revealed multiple round subepithelial nodules, some with central umbilication. One nodule removed by cold snare polypectomy revealed poorly differentiated carcinoma with features indicating adenocarcinoma, and overlying squamous mucosa suggesting it may secondarily be involving the site. The tissue also stained Positive with CDX2 and CK7 suggesting it was from upper GI or pancreaticobiliary source . EUS of the pancreatic lesions revealed a thick-walled, regular, anechoic pancreatic lesion which was biopsied and revealed a mucinous cystic neoplasm. Colonoscopy revealed no IBD or malignancy. The patient followed up with Oncology who performed a PET scan which showed no obvious source of malignancy. Collective findings suggest that this patient had adenocarcinoma from an unknown primary source, however thought to be Upper GI related as his pancreatic biopsies were not remarkable for adenocarcinoma. He was later started on therapy for Upper GI adenocarcinoma by his Oncologist.
Discussion: PG has been strongly related to other diseases such as IBD, arthritis, and hematological malignancies.3 PG connection to paraneoplastic processes such as solid organ malignancies has not been well established, but have been previously reported through case reports. While dysregulated neutrophilic inflammation may lead to solid organ malignancies the direct relationship is unknown. Current USPSTF Cancer screening recommendations make no adjustments for this population. We submit that patients with PG who are experiencing GI symptoms should be evaluated with EGD and colonoscopy to screen for malignancy.
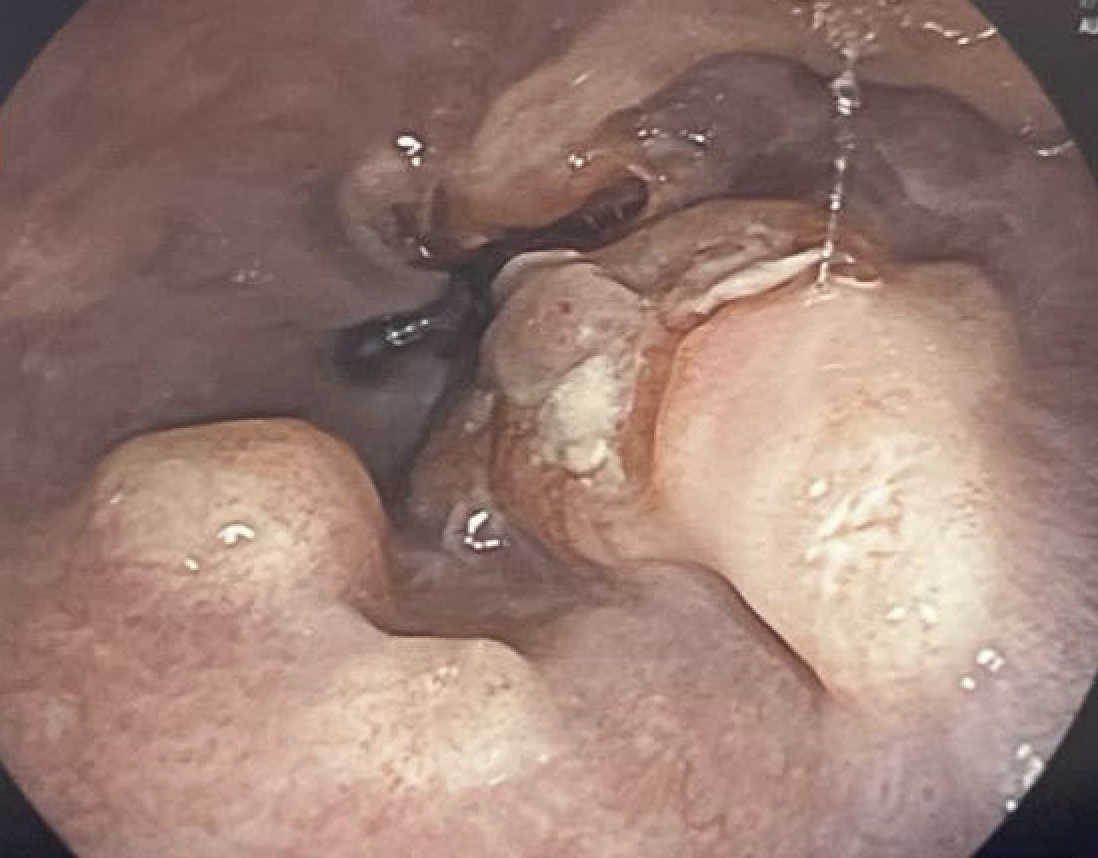
Figure: Endoscopic image of Distal Esophagus with multiple subepithelial nodules s/p polypectomy
Disclosures:
Zan Ferrin indicated no relevant financial relationships.
Tooba Laeeq indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Yssra Soliman indicated no relevant financial relationships.
Aditi Singh indicated no relevant financial relationships.
Zan Ferrin, DO1, Tooba Laeeq, MD2, Yassin Naga, MD2, Yssra Soliman, MD2, Aditi Singh, MD2. P3007 - A Case of Upper GI Adenocarcinoma Preceded by Pyoderma Gangrenosum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Solid organ malignancies in patients with established Pyoderma Gangrenosum (PG) are rare, and few reported cases have been from an upper GI source. In a recent prospective cohort study in the US, of 356 individuals with PG, 23 patients had solid organ malignancies.1 The exact relationship of PG and malignancy is unknown and current cancer screening guidelines make no adjustment for this population.2 This case highlights the importance of conducting a thorough review of symptoms for patients with PG to improve management.
Case Description/
Methods: A 71 year old male with a recent diagnosis of biopsy proven PG presented for evaluation of a 10-day history of acute progressive dysphagia associated with unintentional weight loss. Labs remarkable for ESR: 32, CRP: 1.84, CEA< 0.5. CT scan upon admission was pertinent for a left hepatic lobe cyst measuring 1.6 x 1.2 cm and a pancreatic tail irregular hypodense lesion. EGD revealed multiple round subepithelial nodules, some with central umbilication. One nodule removed by cold snare polypectomy revealed poorly differentiated carcinoma with features indicating adenocarcinoma, and overlying squamous mucosa suggesting it may secondarily be involving the site. The tissue also stained Positive with CDX2 and CK7 suggesting it was from upper GI or pancreaticobiliary source . EUS of the pancreatic lesions revealed a thick-walled, regular, anechoic pancreatic lesion which was biopsied and revealed a mucinous cystic neoplasm. Colonoscopy revealed no IBD or malignancy. The patient followed up with Oncology who performed a PET scan which showed no obvious source of malignancy. Collective findings suggest that this patient had adenocarcinoma from an unknown primary source, however thought to be Upper GI related as his pancreatic biopsies were not remarkable for adenocarcinoma. He was later started on therapy for Upper GI adenocarcinoma by his Oncologist.
Discussion: PG has been strongly related to other diseases such as IBD, arthritis, and hematological malignancies.3 PG connection to paraneoplastic processes such as solid organ malignancies has not been well established, but have been previously reported through case reports. While dysregulated neutrophilic inflammation may lead to solid organ malignancies the direct relationship is unknown. Current USPSTF Cancer screening recommendations make no adjustments for this population. We submit that patients with PG who are experiencing GI symptoms should be evaluated with EGD and colonoscopy to screen for malignancy.
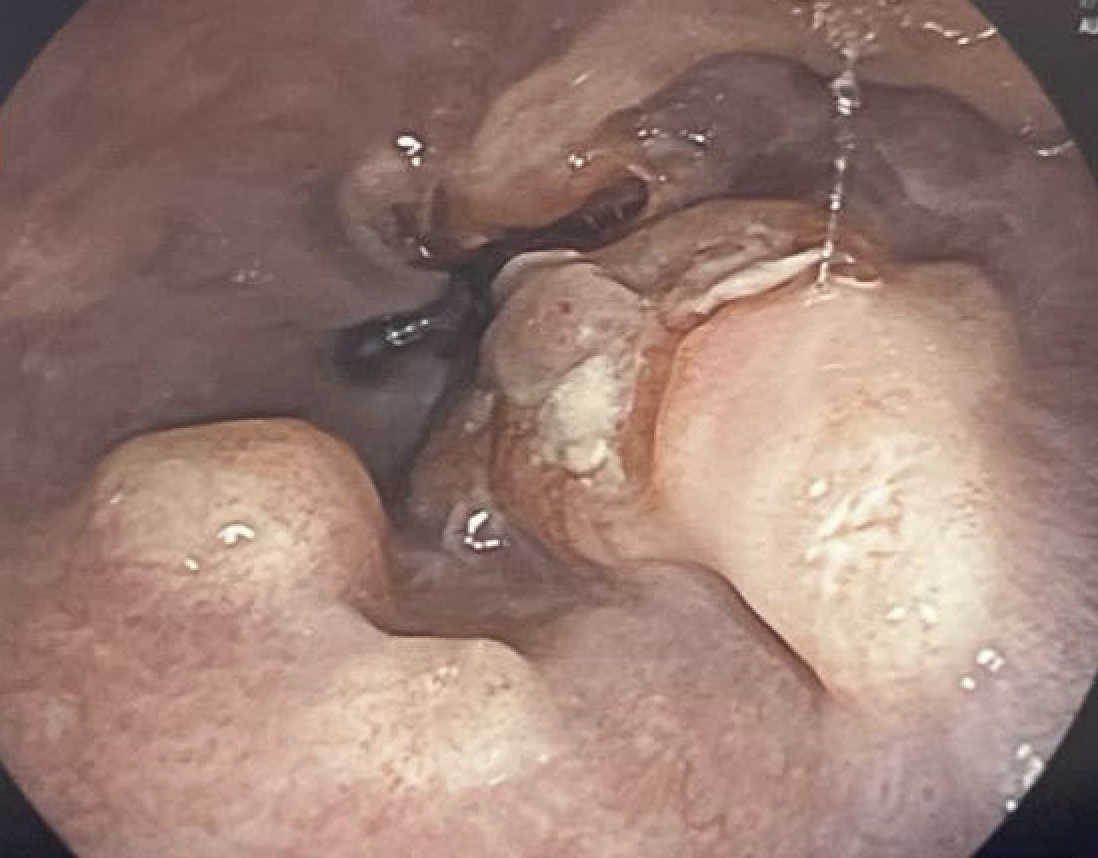
Figure: Endoscopic image of Distal Esophagus with multiple subepithelial nodules s/p polypectomy
Disclosures:
Zan Ferrin indicated no relevant financial relationships.
Tooba Laeeq indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Yssra Soliman indicated no relevant financial relationships.
Aditi Singh indicated no relevant financial relationships.
Zan Ferrin, DO1, Tooba Laeeq, MD2, Yassin Naga, MD2, Yssra Soliman, MD2, Aditi Singh, MD2. P3007 - A Case of Upper GI Adenocarcinoma Preceded by Pyoderma Gangrenosum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
