Monday Poster Session
Category: General Endoscopy
P2997 - Underwater vs Conventional Endoscopic Mucosal Resection for Superficial Non-Ampullary Duodenal Epithelial Tumors ≤20 Mm in Size: An Updated Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Nouman Shafique, MD2, Nihal I. Khan, MD2, Mohamad Khaled Almujarkesh, MD3, Babu P. Mohan, MD4
1Department of Internal Medicine, Adventhealth Orlando, Orlando, FL; 2AdventHealth Orlando, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic mucosal resection (EMR) is the method of choice for resection of superficial non-ampullary duodenal epithelial tumors (SNADETs) ≤20 mm in size. Underwater EMR (UEMR), unlike conventional EMR (CEMR), is a simpler procedure that does not require submucosal injection. Results of studies comparing UEMR and CEMR show mixed results. We conducted a systematic review and meta-analysis aiming to compare the safety and efficacy of UEMR and CEMR for resection of SNADETs ≤20 mm.
Methods: A comprehensive search of MEDLINE, EMBASE, and Scopus was performed through April 2025 to identify studies comparing UEMR and CEMR for SNADETs ≤20 mm. Outcomes assessed included rates of en bloc and R0 resection, delayed bleeding, perforation, and recurrence. Pooled effect estimates were calculated using a random-effects model and expressed as odds ratios (OR) or mean difference (MD) with 95% confidence intervals (CI). Heterogeneity was evaluated using the I² statistic.
Results: A total of seven retrospective studies and 921 SNADET lesions were included. UEMR was used in 413 lesions, while CEMR was used in 508 lesions. Six studies were set in Japan, while one was multi-center and set in five European countries.
There was no difference in the odds of en bloc resection (OR 1.26; 95% CI [0.65, 2.43]; P = 0.5) and R0 resection (OR 1.21; 95% CI [0.68, 2.13]; P = 0.52) in the UEMR compared to the CEMR group. Mean procedure time was significantly shorter in the UEMR group (MD -3.54; 95% CI [-6.67, -0.41]; P = 0.03) (Figure 1).
There was no difference demonstrated in the odds of perforation following resection (OR 0.43; 95% [0.07, 2.65]; P = 0.36), delayed bleeding (OR 0.92; 95% CI [0.20, 4.16]; P = 0.91) and recurrence (OR 0.65; 95% CI [0.27, 1.59]; P = 0.35) (Figure 2).
Discussion: Our meta-analysis shows that the resection of SNADETs ≤20 mm with UEMR carries equal rates of clinical outcomes, including adverse events compared to CEMR while having shorter procedure times. For these lesions, UEMR may be a faster alternative to CEMR with equal efficacy, but further large-scale prospective studies are needed to better define its role.
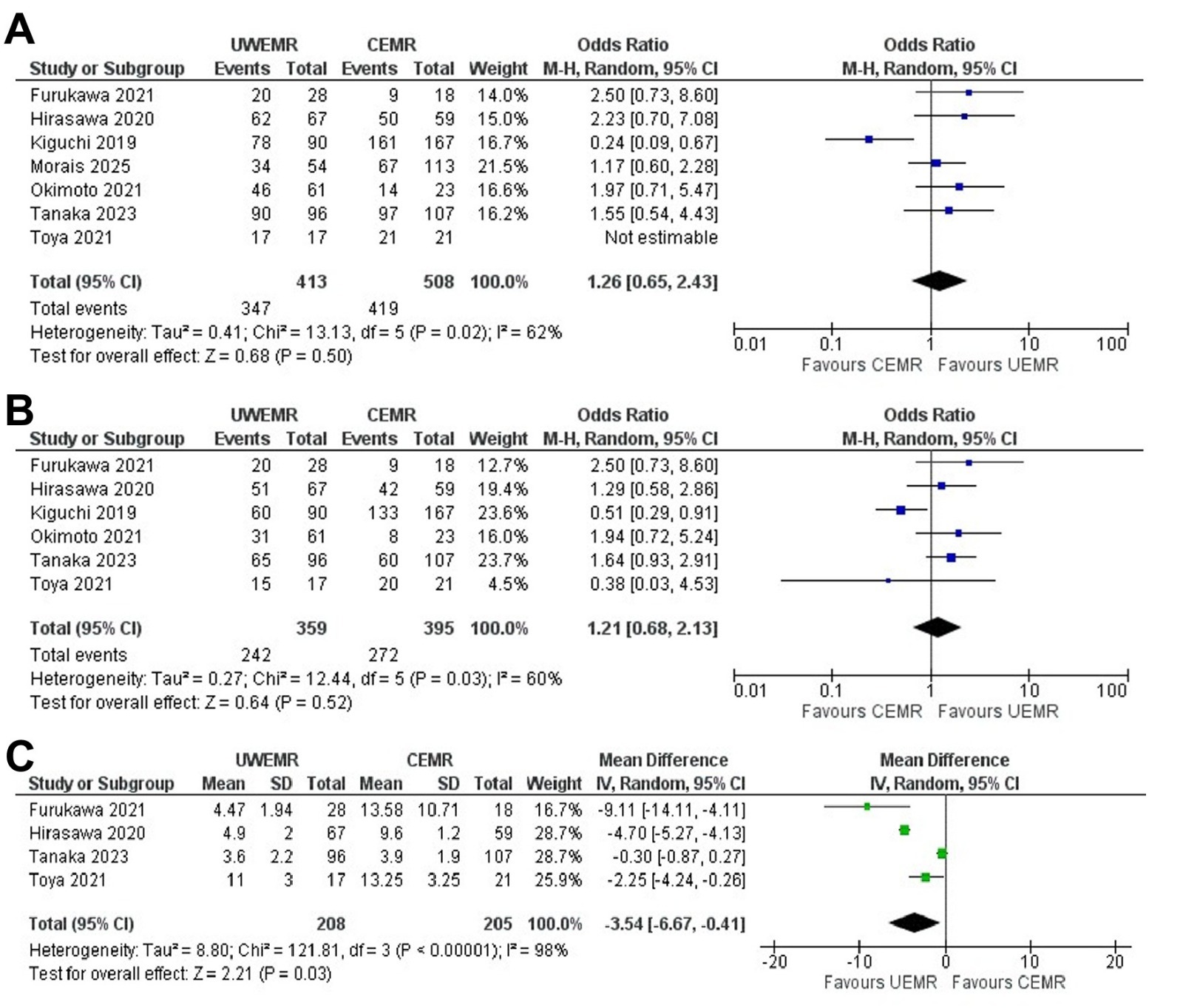
Figure: Pooled odds ratio (OR) between UEMR and CEMR of: A – En bloc resection, B – R0 resection, C – Procedure time
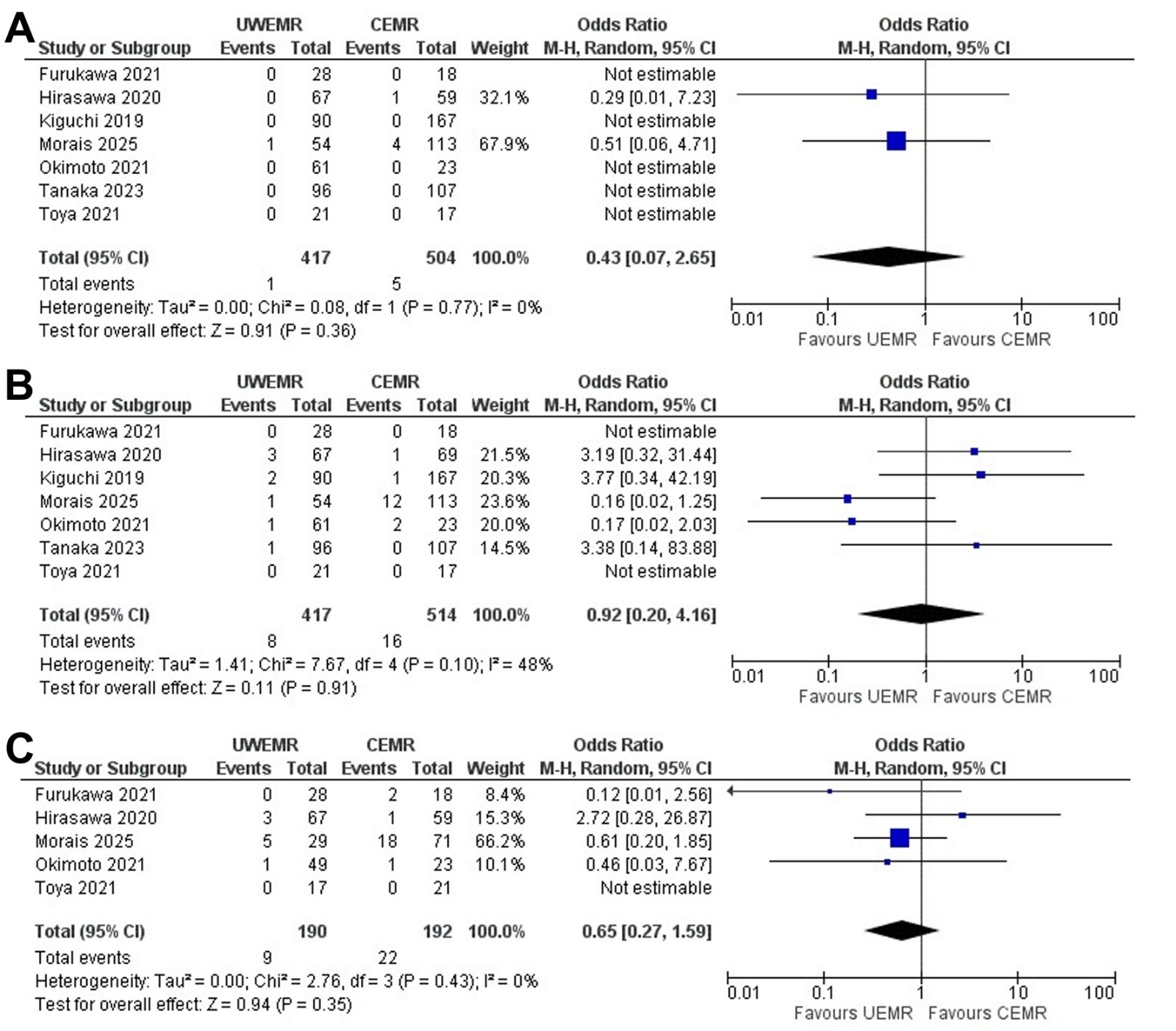
Figure: Pooled odds ratio (OR) between UEMR and CEMR: A - Perforation, B - Delayed Bleeding, C - Recurrence
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Nouman Shafique, MD2, Nihal I. Khan, MD2, Mohamad Khaled Almujarkesh, MD3, Babu P. Mohan, MD4. P2997 - Underwater vs Conventional Endoscopic Mucosal Resection for Superficial Non-Ampullary Duodenal Epithelial Tumors ≤20 Mm in Size: An Updated Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, Adventhealth Orlando, Orlando, FL; 2AdventHealth Orlando, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Endoscopic mucosal resection (EMR) is the method of choice for resection of superficial non-ampullary duodenal epithelial tumors (SNADETs) ≤20 mm in size. Underwater EMR (UEMR), unlike conventional EMR (CEMR), is a simpler procedure that does not require submucosal injection. Results of studies comparing UEMR and CEMR show mixed results. We conducted a systematic review and meta-analysis aiming to compare the safety and efficacy of UEMR and CEMR for resection of SNADETs ≤20 mm.
Methods: A comprehensive search of MEDLINE, EMBASE, and Scopus was performed through April 2025 to identify studies comparing UEMR and CEMR for SNADETs ≤20 mm. Outcomes assessed included rates of en bloc and R0 resection, delayed bleeding, perforation, and recurrence. Pooled effect estimates were calculated using a random-effects model and expressed as odds ratios (OR) or mean difference (MD) with 95% confidence intervals (CI). Heterogeneity was evaluated using the I² statistic.
Results: A total of seven retrospective studies and 921 SNADET lesions were included. UEMR was used in 413 lesions, while CEMR was used in 508 lesions. Six studies were set in Japan, while one was multi-center and set in five European countries.
There was no difference in the odds of en bloc resection (OR 1.26; 95% CI [0.65, 2.43]; P = 0.5) and R0 resection (OR 1.21; 95% CI [0.68, 2.13]; P = 0.52) in the UEMR compared to the CEMR group. Mean procedure time was significantly shorter in the UEMR group (MD -3.54; 95% CI [-6.67, -0.41]; P = 0.03) (Figure 1).
There was no difference demonstrated in the odds of perforation following resection (OR 0.43; 95% [0.07, 2.65]; P = 0.36), delayed bleeding (OR 0.92; 95% CI [0.20, 4.16]; P = 0.91) and recurrence (OR 0.65; 95% CI [0.27, 1.59]; P = 0.35) (Figure 2).
Discussion: Our meta-analysis shows that the resection of SNADETs ≤20 mm with UEMR carries equal rates of clinical outcomes, including adverse events compared to CEMR while having shorter procedure times. For these lesions, UEMR may be a faster alternative to CEMR with equal efficacy, but further large-scale prospective studies are needed to better define its role.
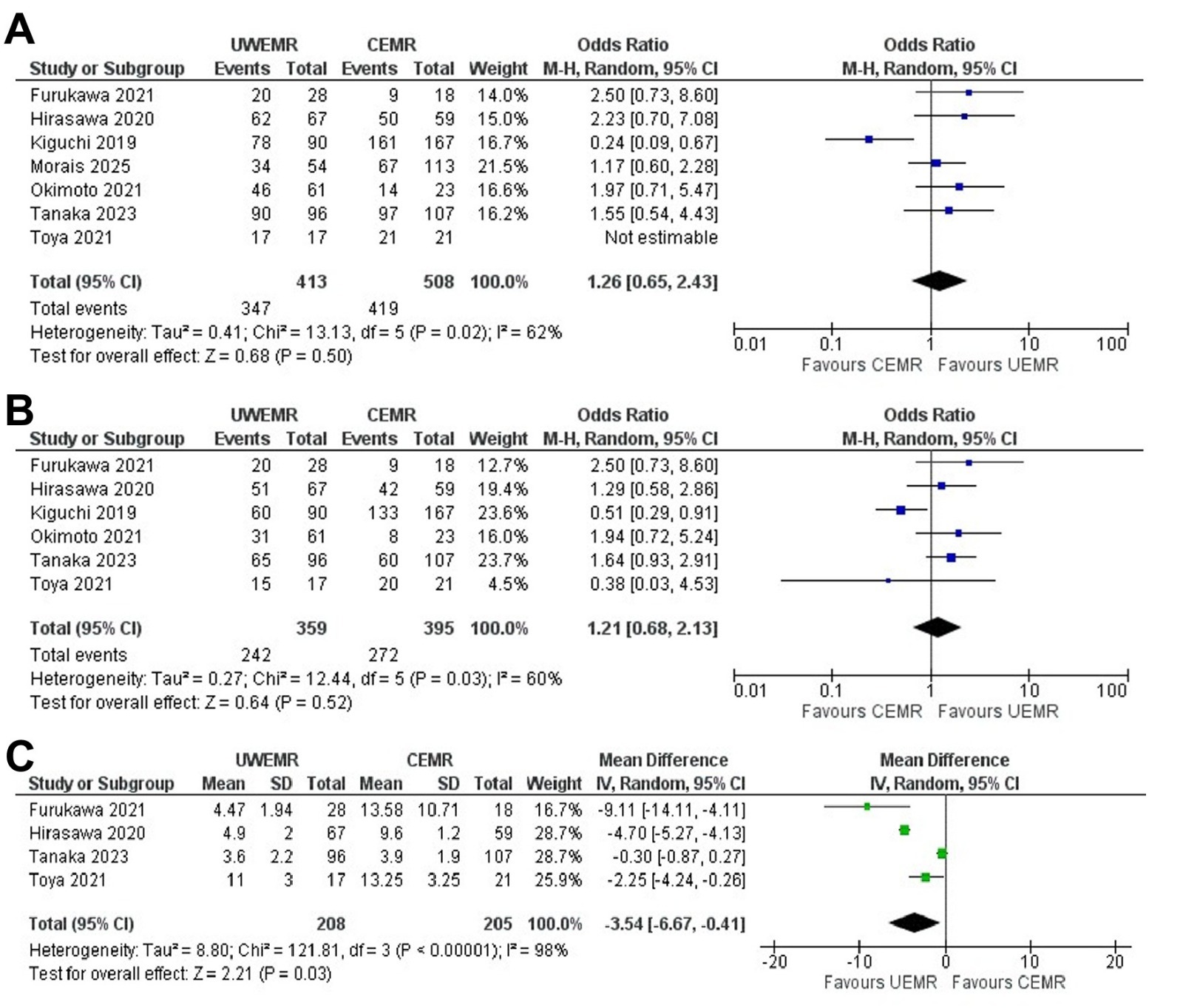
Figure: Pooled odds ratio (OR) between UEMR and CEMR of: A – En bloc resection, B – R0 resection, C – Procedure time
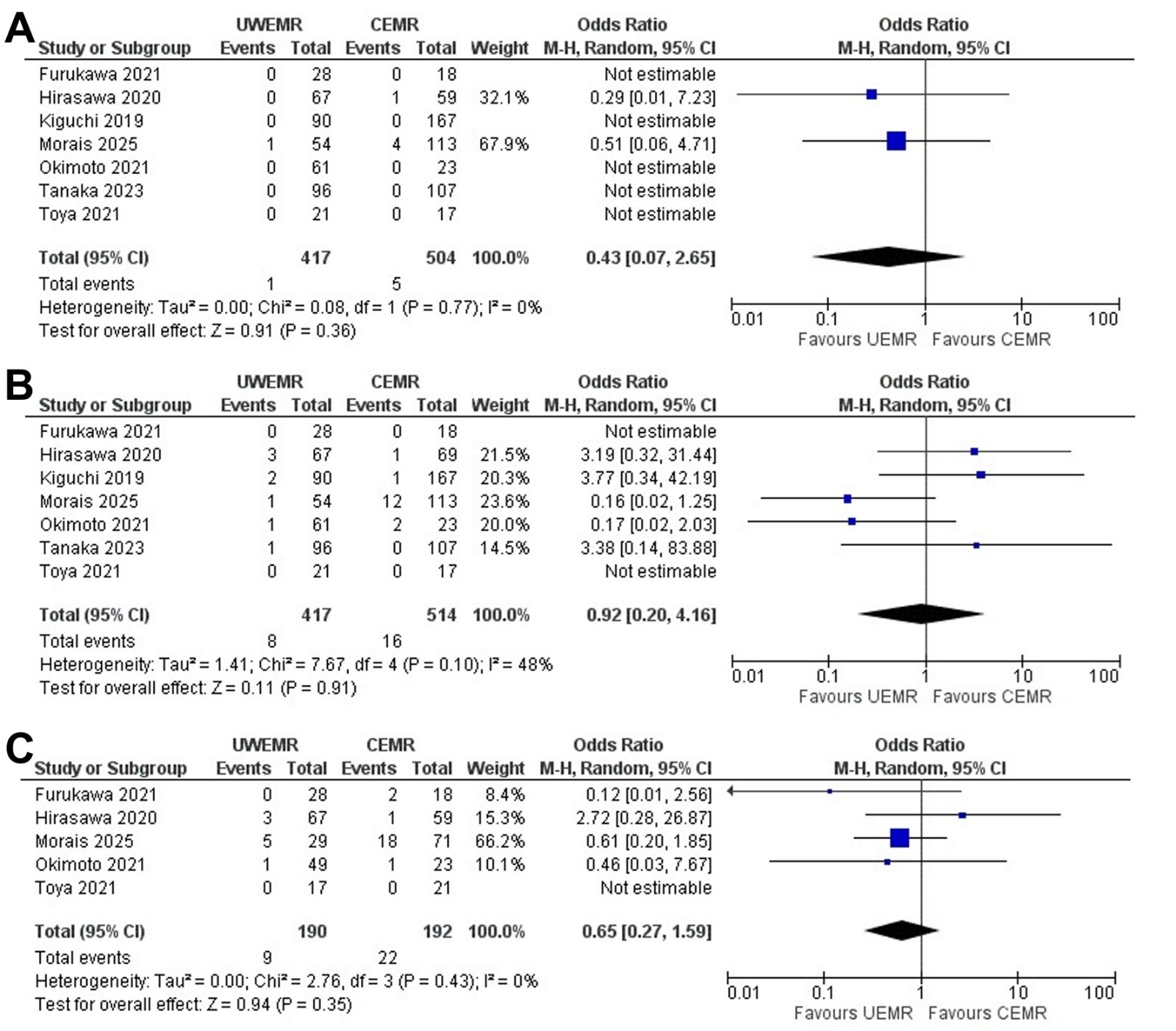
Figure: Pooled odds ratio (OR) between UEMR and CEMR: A - Perforation, B - Delayed Bleeding, C - Recurrence
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Nouman Shafique, MD2, Nihal I. Khan, MD2, Mohamad Khaled Almujarkesh, MD3, Babu P. Mohan, MD4. P2997 - Underwater vs Conventional Endoscopic Mucosal Resection for Superficial Non-Ampullary Duodenal Epithelial Tumors ≤20 Mm in Size: An Updated Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
