Monday Poster Session
Category: General Endoscopy
P2990 - Impact of Pulmonary Hypertension on Inpatient Outcomes Among Patients Undergoing Colonoscopy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hameed Ullah, MD
St. Luke's Hospital
Chesterfield, MO
Presenting Author(s)
Hameed Ullah, MD1, Mohamad Sharbatji, MD2, Wagmah Javed. Khan, MD1, Ijaz Ali, MD3, Muhammad Arsalan, MD1, Mustafa Shah, MD4, Osama Sherjeel Khan, MD5, Muhammad Waseem, MBBS6, Mohammad Asfari, MD7
1St. Luke's Hospital, Chesterfield, MO; 2AdventHealth, Orlando, FL; 3Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 4Geisinger Health System, Danville, PA; 5Cleveland Clinic Florida, Weston, FL; 6Ayub Teaching Hospital, Chesterfield, MO; 7Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Pulmonary hypertension (pHTN) is associated with hemodynamic instability and unfavorable intra-operative and post-operative outcomes. However, limited data exists on the impact of pHTN during non-surgical procedures such as colonoscopy. We evaluated inpatient outcomes in patients with pHTN undergoing colonoscopy using a large, nationally representative dataset.
Methods: We conducted a retrospective cohort study using the 2020–2021 National Inpatient Sample (NIS). Adult hospitalizations in which colonoscopy was performed were identified using ICD-10-PCS codes. Pulmonary hypertension was identified using a comprehensive set of ICD-10 codes across all diagnosis fields. Survey-weighted descriptive statistics and multivariable analyses were used. The primary exposure was presence of any pHTN. Primary outcomes included in-hospital mortality and acute procedural complications. Secondary outcomes included post-procedural shock, cardiac arrest, intubation, vasopressor use, acute kidney injury (AKI), and acute respiratory failure (ARF). Models were adjusted for demographics, the Charlson comorbidity index, hospital characteristics, and comorbidities, including coronary artery disease (CAD), chronic kidney disease (CKD), and obesity.
Results: Out of an estimated 912,094 weighted adult colonoscopy hospitalizations, 4.8% had a diagnosis of pHTN. Patients with pHTN were older (mean age 72.6 vs 64.7 years, p< 0.001), more likely to be female (57% vs 51%), and had higher comorbidity burdens (Charlson index ≥3: 74.6% vs 44.8%, p< 0.001). Significant differences were observed in insurance status, hospital characteristics, and race distribution between groups. Patients with pHTN had markedly higher rates of post-procedural shock, cardiac arrest, intubation, vasopressor use, AKI, and ARF, all with p-values < 0.001. Baseline characteristics are detailed in table.1. Adjusted outcomes are shown in the infographic given below.
Discussion: In this national cohort, pulmonary hypertension was associated increased burden of comorbidity and significantly worse inpatient outcomes following colonoscopy. These findings emphasize the importance of risk stratification and vigilant peri-procedural monitoring in patients with pulmonary hypertension undergoing colonoscopy.
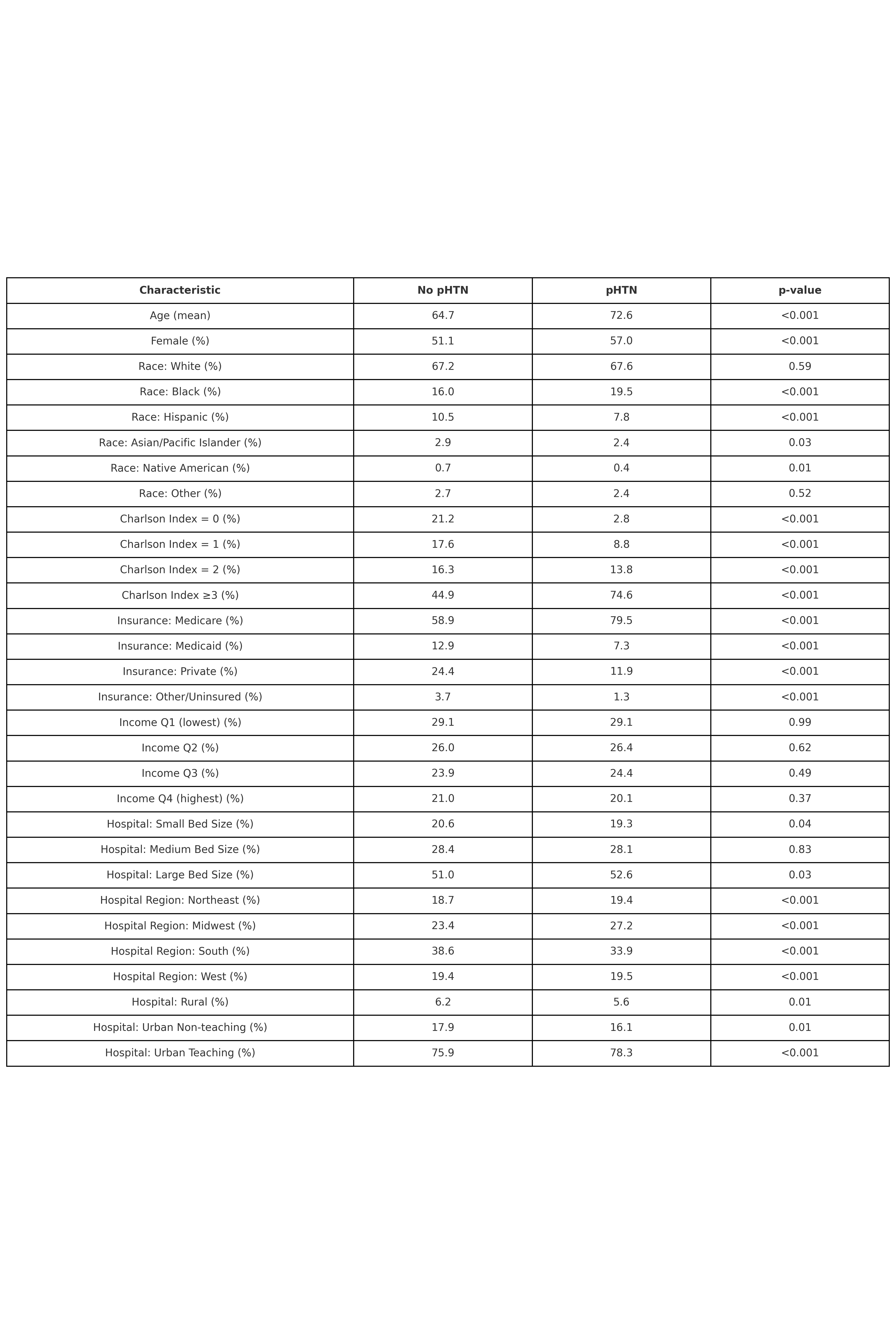
Figure: Table. 1: Baseline Characteristics
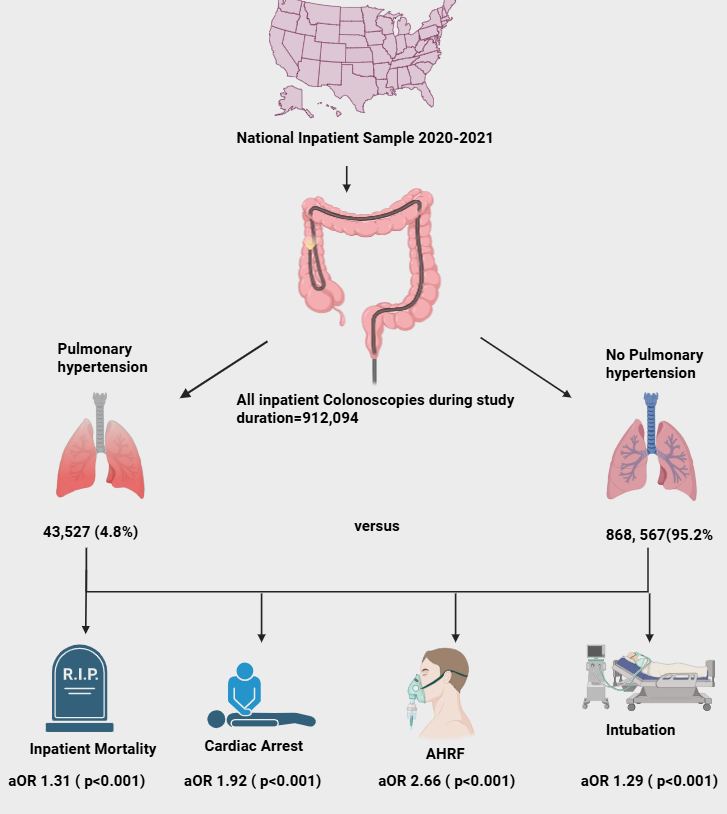
Figure: Adjusted outcomes Infographic
Disclosures:
Hameed Ullah indicated no relevant financial relationships.
Mohamad Sharbatji indicated no relevant financial relationships.
Wagmah Khan indicated no relevant financial relationships.
Ijaz Ali indicated no relevant financial relationships.
Muhammad Arsalan indicated no relevant financial relationships.
Mustafa Shah indicated no relevant financial relationships.
Osama Sherjeel Khan indicated no relevant financial relationships.
Muhammad Waseem indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Hameed Ullah, MD1, Mohamad Sharbatji, MD2, Wagmah Javed. Khan, MD1, Ijaz Ali, MD3, Muhammad Arsalan, MD1, Mustafa Shah, MD4, Osama Sherjeel Khan, MD5, Muhammad Waseem, MBBS6, Mohammad Asfari, MD7. P2990 - Impact of Pulmonary Hypertension on Inpatient Outcomes Among Patients Undergoing Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's Hospital, Chesterfield, MO; 2AdventHealth, Orlando, FL; 3Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 4Geisinger Health System, Danville, PA; 5Cleveland Clinic Florida, Weston, FL; 6Ayub Teaching Hospital, Chesterfield, MO; 7Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Pulmonary hypertension (pHTN) is associated with hemodynamic instability and unfavorable intra-operative and post-operative outcomes. However, limited data exists on the impact of pHTN during non-surgical procedures such as colonoscopy. We evaluated inpatient outcomes in patients with pHTN undergoing colonoscopy using a large, nationally representative dataset.
Methods: We conducted a retrospective cohort study using the 2020–2021 National Inpatient Sample (NIS). Adult hospitalizations in which colonoscopy was performed were identified using ICD-10-PCS codes. Pulmonary hypertension was identified using a comprehensive set of ICD-10 codes across all diagnosis fields. Survey-weighted descriptive statistics and multivariable analyses were used. The primary exposure was presence of any pHTN. Primary outcomes included in-hospital mortality and acute procedural complications. Secondary outcomes included post-procedural shock, cardiac arrest, intubation, vasopressor use, acute kidney injury (AKI), and acute respiratory failure (ARF). Models were adjusted for demographics, the Charlson comorbidity index, hospital characteristics, and comorbidities, including coronary artery disease (CAD), chronic kidney disease (CKD), and obesity.
Results: Out of an estimated 912,094 weighted adult colonoscopy hospitalizations, 4.8% had a diagnosis of pHTN. Patients with pHTN were older (mean age 72.6 vs 64.7 years, p< 0.001), more likely to be female (57% vs 51%), and had higher comorbidity burdens (Charlson index ≥3: 74.6% vs 44.8%, p< 0.001). Significant differences were observed in insurance status, hospital characteristics, and race distribution between groups. Patients with pHTN had markedly higher rates of post-procedural shock, cardiac arrest, intubation, vasopressor use, AKI, and ARF, all with p-values < 0.001. Baseline characteristics are detailed in table.1. Adjusted outcomes are shown in the infographic given below.
Discussion: In this national cohort, pulmonary hypertension was associated increased burden of comorbidity and significantly worse inpatient outcomes following colonoscopy. These findings emphasize the importance of risk stratification and vigilant peri-procedural monitoring in patients with pulmonary hypertension undergoing colonoscopy.
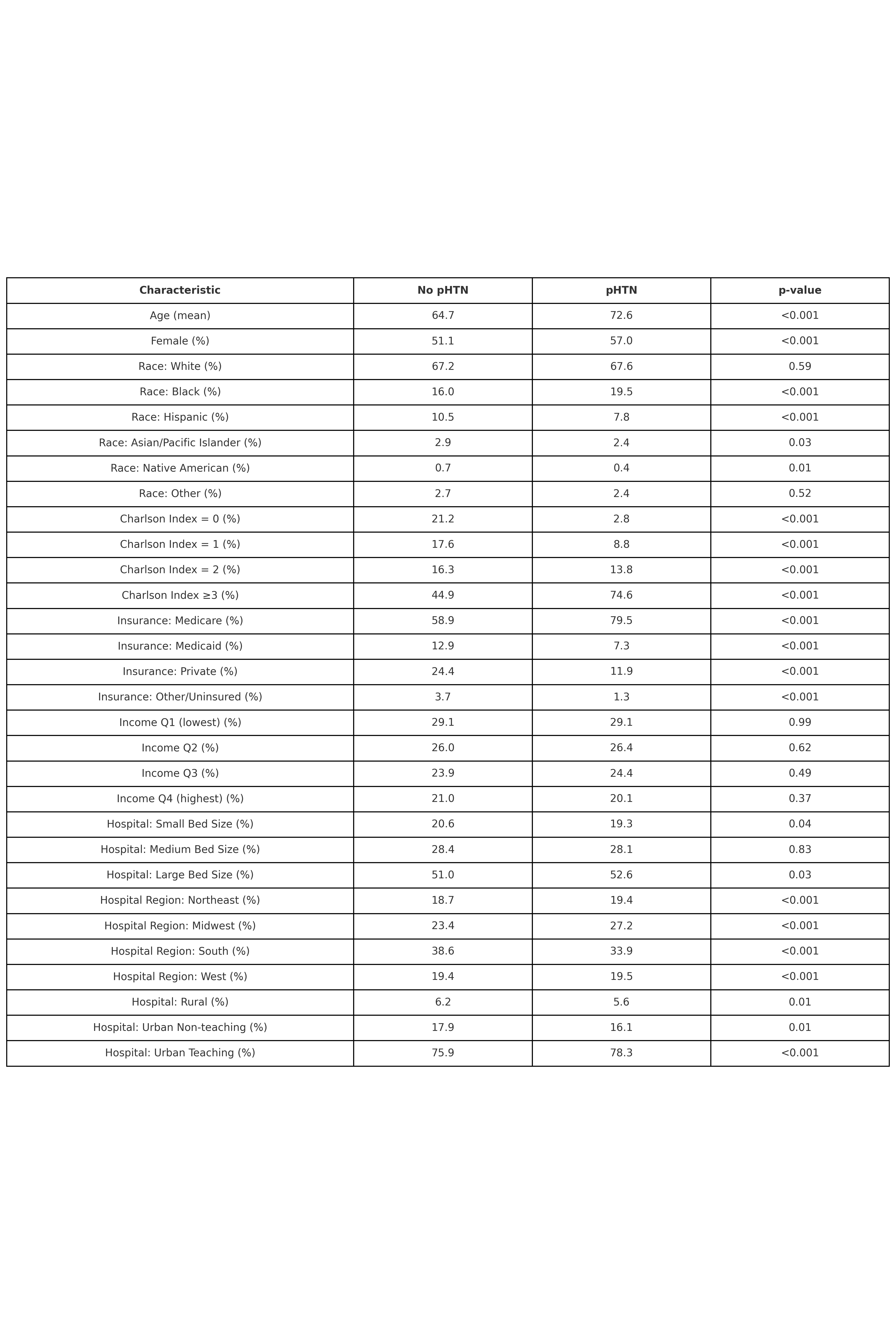
Figure: Table. 1: Baseline Characteristics
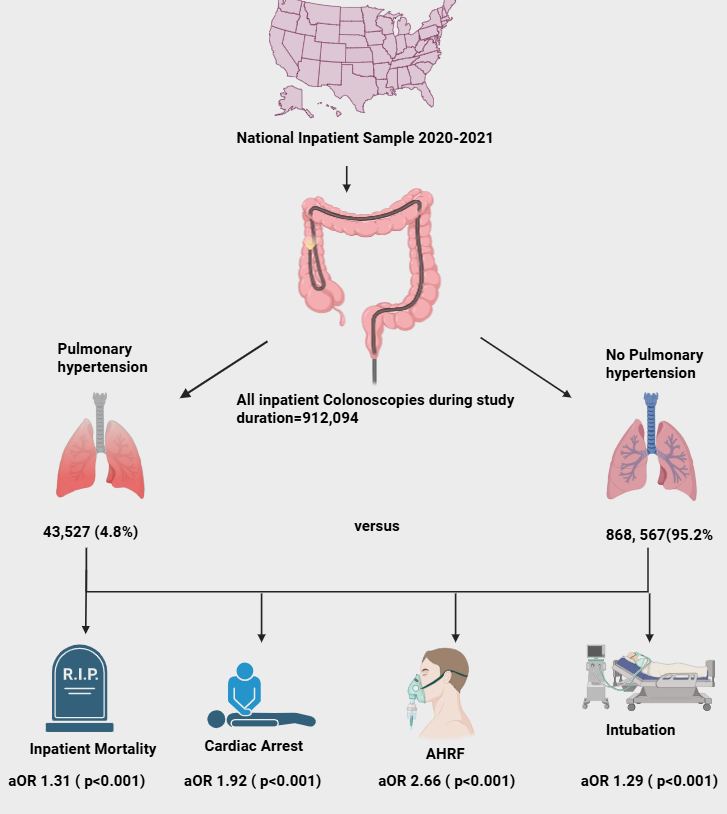
Figure: Adjusted outcomes Infographic
Disclosures:
Hameed Ullah indicated no relevant financial relationships.
Mohamad Sharbatji indicated no relevant financial relationships.
Wagmah Khan indicated no relevant financial relationships.
Ijaz Ali indicated no relevant financial relationships.
Muhammad Arsalan indicated no relevant financial relationships.
Mustafa Shah indicated no relevant financial relationships.
Osama Sherjeel Khan indicated no relevant financial relationships.
Muhammad Waseem indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Hameed Ullah, MD1, Mohamad Sharbatji, MD2, Wagmah Javed. Khan, MD1, Ijaz Ali, MD3, Muhammad Arsalan, MD1, Mustafa Shah, MD4, Osama Sherjeel Khan, MD5, Muhammad Waseem, MBBS6, Mohammad Asfari, MD7. P2990 - Impact of Pulmonary Hypertension on Inpatient Outcomes Among Patients Undergoing Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
