Monday Poster Session
Category: General Endoscopy
P2989 - Yield of Esophagogastroduodenoscopy After Positive FOBT and Negative Colonoscopy: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Avneet Kaur, MBBS (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Avneet Kaur, MBBS1, Akhil Gupta, MBBS2, Anjul Verma, MD3, Guy Loic Nguefang Tchoukeu, MD3, Babu P. Mohan, MD4
1SUNY Upstate Medical University, Syracuse, NY; 2Government Medical College, Patiala, Ambala, Haryana, India; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: The role of esophagogastroduodenoscopy (EGD) in patients with a positive fecal occult blood test (FOBT) and negative colonoscopy remains unclear. We conducted a meta-analysis to assess the diagnostic yield of EGD in this patient population.
Methods: We systematically reviewed studies reporting outcomes of EGD in patients with positive FOBT and normal colonoscopy, from PubMed, Embase and Scopus. Pooled prevalence and 95% confidence intervals (CI) were calculated using a fixed-effect model. Subgroup analyses were performed based on lesion type (e.g., ulcers, vascular, erosive, neoplastic).
Results: Nineteen studies comprising a total of 7,773 patients were included. The mean age was 59.5 ± 5.6 years, and 50.6% females. .The pooled prevalence of significant EGD findings in patients with positive FOBT but negative colonoscopy was 22.0% (95% CI: 20.8–23.4). In subgroup analysis, ulcerative lesions were the most frequently identified findings, with a pooled prevalence of 6.6% (95% CI: 6.1–7.2), including erosions (n=85), stomach ulcers (n=256), duodenal ulcers (n=64), and esophageal ulcer/esophagitis (n=195).
Inflammatory lesions had a prevalence of 5.7% (95% CI: 5.2–6.2), predominantly gastritis (n=455), gastropathy (n=21), and duodenitis (n=40). Vascular lesions were found in 1.1% (95% CI: 0.9–1.4), including gastroesophageal varices (n=51), vascular ectasias (n=18), and vascular malformations (n=35). Upper gastrointestinal cancers were uncommon, with a pooled prevalence of 0.67% (95% CI: 0.53–0.87) across oral, esophageal, gastric, small bowel, and unspecified cancers.
Barrett’s esophagus was identified in 0.64% (95% CI: 0.50–0.83) of patients. Structural findings such as esophageal strictures and other miscellaneous lesions were less common. Lesions unlikely to bleed, adenomas, and polyps were classified as "Other" and had a pooled prevalence of 2.7% (95% CI: 2.4–3.1). Egger’s test revealed no evidence of publication bias (p = 0.60).
Discussion: EGD identified clinically relevant pathology in approximately 1 in 5 patients with positive FOBT and negative colonoscopy. Malignancy was reported in approximately 7 in 1000 patients. These findings seem to support consideration of EGD in select patients, particularly those with additional risk factors or unexplained anemia.
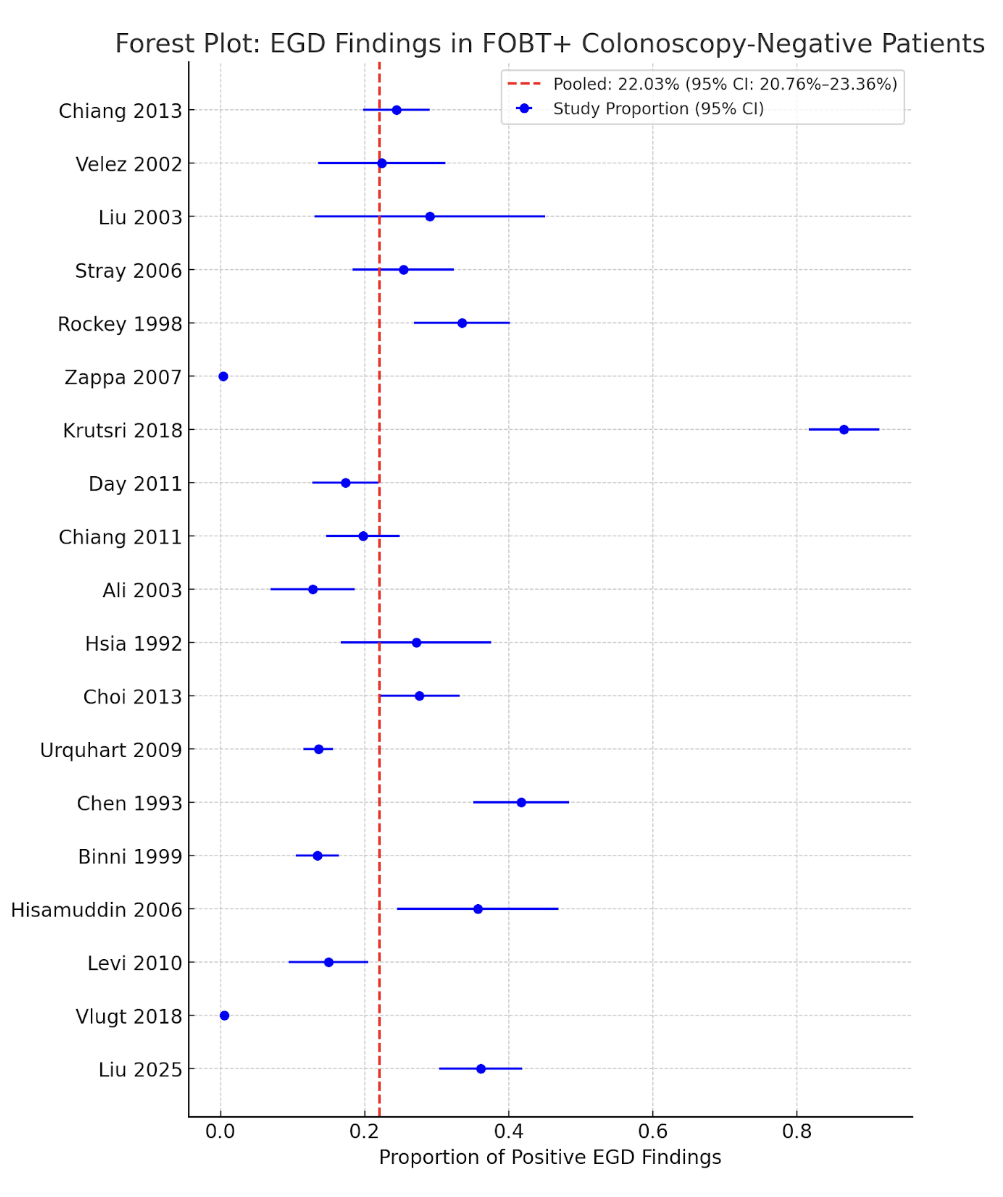
Figure: Figure 1. Forest plot showing the proportion of positive EGD findings across individual studies in patients with positive FOBT and negative colonoscopy. The pooled proportion estimate is 22.03% (95% CI: 20.76–23.36), as indicated by the red dashed line. Blue circles represent study proportions, and horizontal lines indicate 95% confidence intervals.
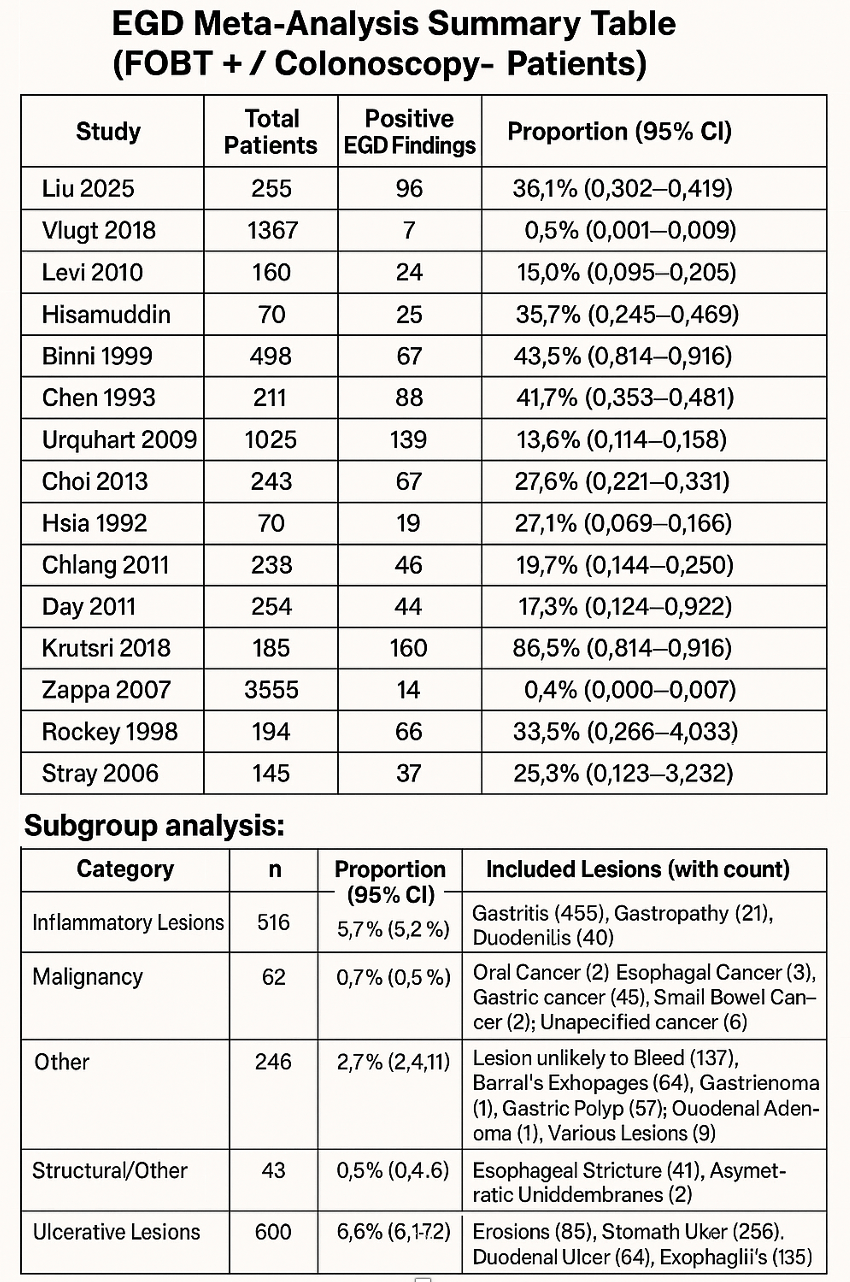
Figure: Figure 2. Summary of studies reporting positive EGD findings in patients with FOBT-positive and colonoscopy-negative results. Includes total patients, proportion with positive findings (95% CI), and subgroup analysis of lesion types.
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Akhil Gupta indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Akhil Gupta, MBBS2, Anjul Verma, MD3, Guy Loic Nguefang Tchoukeu, MD3, Babu P. Mohan, MD4. P2989 - Yield of Esophagogastroduodenoscopy After Positive FOBT and Negative Colonoscopy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University, Syracuse, NY; 2Government Medical College, Patiala, Ambala, Haryana, India; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: The role of esophagogastroduodenoscopy (EGD) in patients with a positive fecal occult blood test (FOBT) and negative colonoscopy remains unclear. We conducted a meta-analysis to assess the diagnostic yield of EGD in this patient population.
Methods: We systematically reviewed studies reporting outcomes of EGD in patients with positive FOBT and normal colonoscopy, from PubMed, Embase and Scopus. Pooled prevalence and 95% confidence intervals (CI) were calculated using a fixed-effect model. Subgroup analyses were performed based on lesion type (e.g., ulcers, vascular, erosive, neoplastic).
Results: Nineteen studies comprising a total of 7,773 patients were included. The mean age was 59.5 ± 5.6 years, and 50.6% females. .The pooled prevalence of significant EGD findings in patients with positive FOBT but negative colonoscopy was 22.0% (95% CI: 20.8–23.4). In subgroup analysis, ulcerative lesions were the most frequently identified findings, with a pooled prevalence of 6.6% (95% CI: 6.1–7.2), including erosions (n=85), stomach ulcers (n=256), duodenal ulcers (n=64), and esophageal ulcer/esophagitis (n=195).
Inflammatory lesions had a prevalence of 5.7% (95% CI: 5.2–6.2), predominantly gastritis (n=455), gastropathy (n=21), and duodenitis (n=40). Vascular lesions were found in 1.1% (95% CI: 0.9–1.4), including gastroesophageal varices (n=51), vascular ectasias (n=18), and vascular malformations (n=35). Upper gastrointestinal cancers were uncommon, with a pooled prevalence of 0.67% (95% CI: 0.53–0.87) across oral, esophageal, gastric, small bowel, and unspecified cancers.
Barrett’s esophagus was identified in 0.64% (95% CI: 0.50–0.83) of patients. Structural findings such as esophageal strictures and other miscellaneous lesions were less common. Lesions unlikely to bleed, adenomas, and polyps were classified as "Other" and had a pooled prevalence of 2.7% (95% CI: 2.4–3.1). Egger’s test revealed no evidence of publication bias (p = 0.60).
Discussion: EGD identified clinically relevant pathology in approximately 1 in 5 patients with positive FOBT and negative colonoscopy. Malignancy was reported in approximately 7 in 1000 patients. These findings seem to support consideration of EGD in select patients, particularly those with additional risk factors or unexplained anemia.
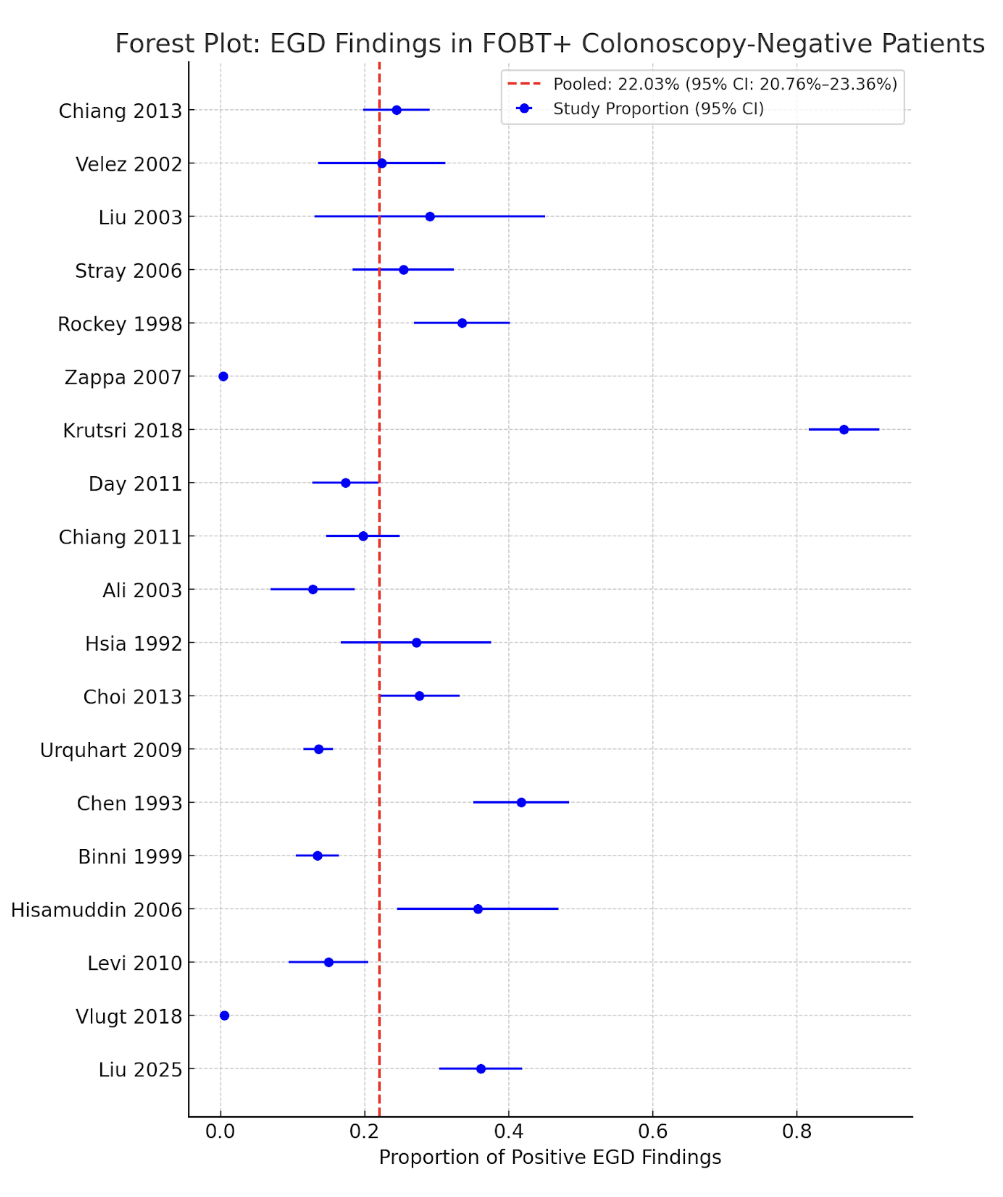
Figure: Figure 1. Forest plot showing the proportion of positive EGD findings across individual studies in patients with positive FOBT and negative colonoscopy. The pooled proportion estimate is 22.03% (95% CI: 20.76–23.36), as indicated by the red dashed line. Blue circles represent study proportions, and horizontal lines indicate 95% confidence intervals.
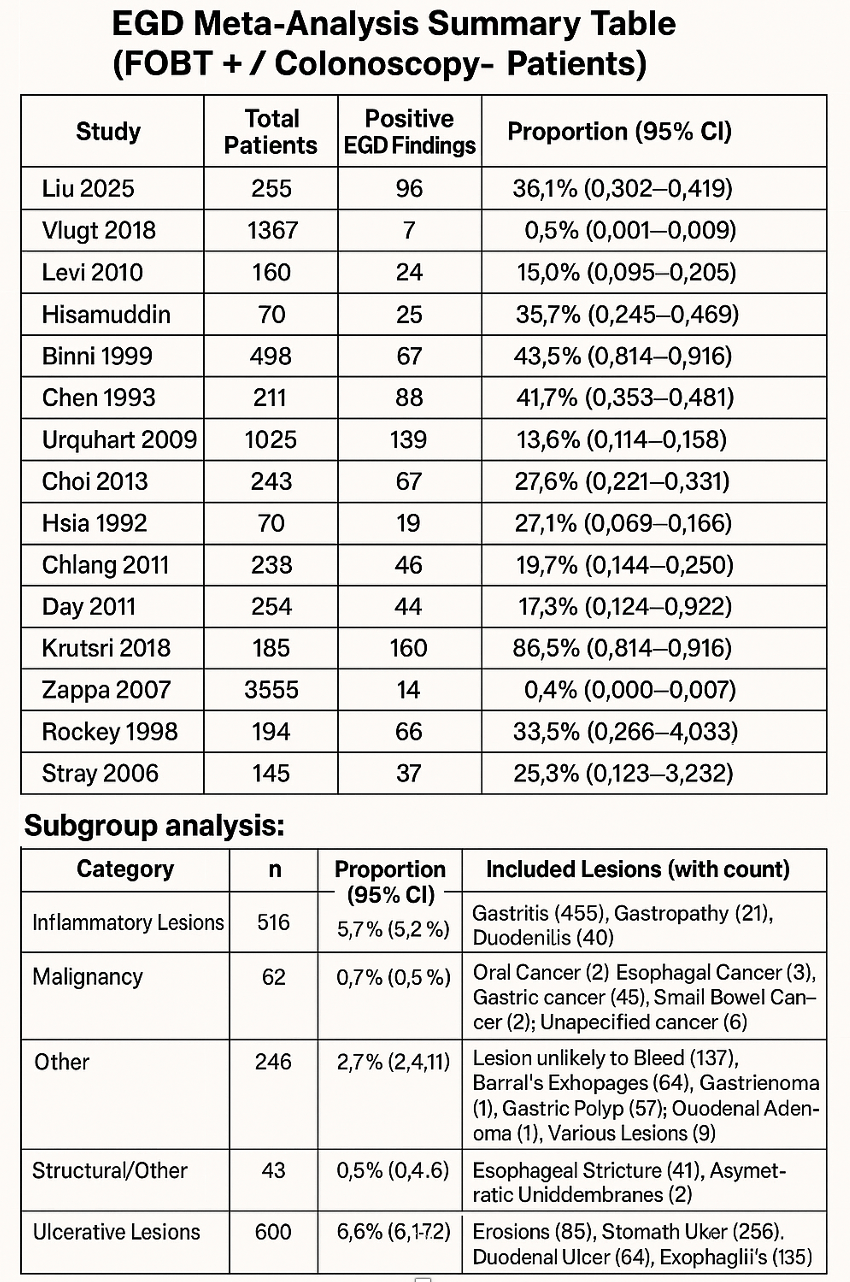
Figure: Figure 2. Summary of studies reporting positive EGD findings in patients with FOBT-positive and colonoscopy-negative results. Includes total patients, proportion with positive findings (95% CI), and subgroup analysis of lesion types.
Disclosures:
Avneet Kaur indicated no relevant financial relationships.
Akhil Gupta indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Avneet Kaur, MBBS1, Akhil Gupta, MBBS2, Anjul Verma, MD3, Guy Loic Nguefang Tchoukeu, MD3, Babu P. Mohan, MD4. P2989 - Yield of Esophagogastroduodenoscopy After Positive FOBT and Negative Colonoscopy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
