Monday Poster Session
Category: Functional Bowel Disease
P2945 - Understanding the Psychiatric Profile and Sociodemographics of Adults With Irritable Bowel Syndrome: A 10-Year Multicenter Electronic Health Record Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Archana Kharel, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Archana Kharel, MD1, Venkata Sunkesula, MD2, Umesh Bhagat, MD3, Prabhat Kumar, MD4, Lana Dardari, MD5, Gengqing Song, MD, PhD6
1Cleveland Clinic, Cleveland, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Virginia Commonwealth University, Richmond, VA; 5Cleveland Clinic Foundation, Westlake, OH; 6Case Western Reserve University/Metro Health, Cleveland, OH
Introduction: Irritable bowel syndrome (IBS) is frequently accompanied by psychiatric comorbidities that may exacerbate symptom burden and drive healthcare utilization. Contemporary, population-level estimates of mental-health disorders in IBS are limited. We utilized the TriNetX federated research network to evaluate the burden and demographic distribution of psychiatric conditions among adults with IBS.
Methods: We conducted a retrospective analysis of de-identified electronic health records from 100 U.S. healthcare organizations in the TriNetX Research Network from Jan 1, 2015 to Apr 28, 2025. Adults ≥18 years with ≥1 ICD-10-CM diagnosis of IBS (K58.0–K58.9) were included. Psychiatric comorbidities were identified using the following ICD-10-CM codes: major depressive disorder (F32, F33), generalized anxiety disorder (F41.1), bipolar disorder (F31), schizophrenia-spectrum disorders (F20–F29), post-traumatic stress disorder (F43.1), and obsessive-compulsive disorder (F42). Outcomes included incidence, prevalence, peak age range, and stratification by sex and race/ethnicity.
Results: Among 1,275,194 adults with IBS (mean age 45 ± 17 years; 67% female), the most common psychiatric comorbidities were MDD (prevalence: 38.3%) and GAD (17.9%), followed by PTSD (5.6%), BPD (5.5%), OCD (1.9%), and lastly schizophrenia (0.8%). Females exhibited a greater psychiatric burden across nearly all diagnoses, including MDD (41.6% vs. 27.6%), GAD (19.1% vs. 13.5%),BPD ( 5.9% vs 3.9%), OCD (1.93% vs. 1.74%) and PTSD (6.2% vs. 3.8%). Native Hawaiian/Pacific Islander had the highest prevalence of MDD (51.6%), GAD (61.7%) and American Indian/Alaska Native patients had the highest prevalence of BPD(9.7%), OCD(2.8%) and PTSD (14.8%) whereas Black or African-American population had the highest prevalence of schizophrenia (2.1%). Asian patients consistently had the lowest prevalence across all psychiatric conditions.
Discussion: In this nationwide real-world cohort more than half of adults with IBS carried at least one psychiatric diagnosis, most commonly MDD and GAD with markedly higher burdens in women and in several under-represented minority populations.These findings underscore the importance of routine mental-health screening and culturally tailored, integrated care pathways for patients with IBS, particularly for high-risk sex and racial/ethnic groups, to help reduce symptom burden and optimize resource utilization.
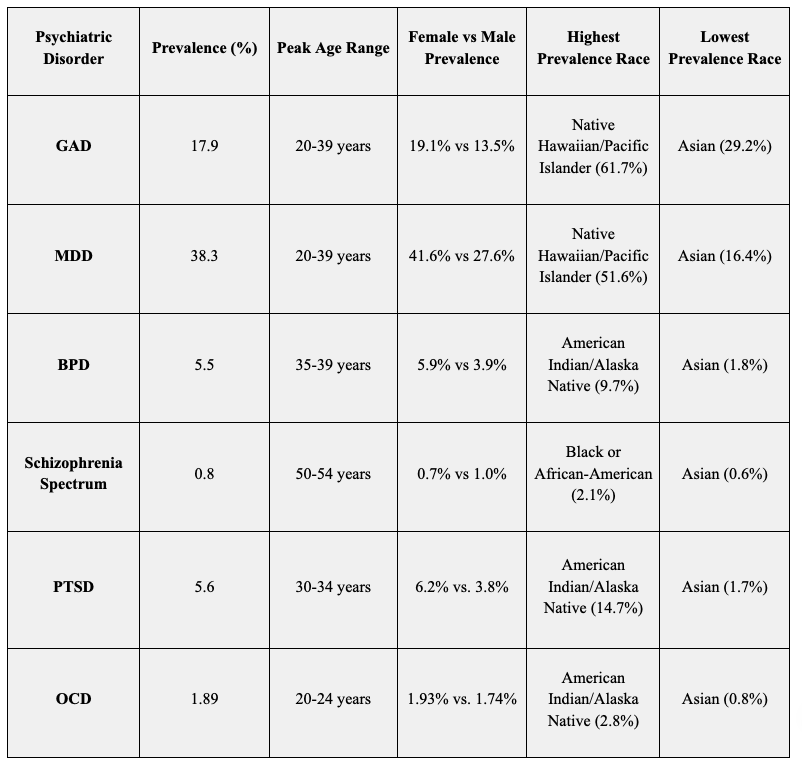
Figure: Table: Psychiatric Comorbidity Trends in Adult IBS Patients Stratified by Age, Sex, and Race/Ethnicity (2015–2025)
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Lana Dardari indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Archana Kharel, MD1, Venkata Sunkesula, MD2, Umesh Bhagat, MD3, Prabhat Kumar, MD4, Lana Dardari, MD5, Gengqing Song, MD, PhD6. P2945 - Understanding the Psychiatric Profile and Sociodemographics of Adults With Irritable Bowel Syndrome: A 10-Year Multicenter Electronic Health Record Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Virginia Commonwealth University, Richmond, VA; 5Cleveland Clinic Foundation, Westlake, OH; 6Case Western Reserve University/Metro Health, Cleveland, OH
Introduction: Irritable bowel syndrome (IBS) is frequently accompanied by psychiatric comorbidities that may exacerbate symptom burden and drive healthcare utilization. Contemporary, population-level estimates of mental-health disorders in IBS are limited. We utilized the TriNetX federated research network to evaluate the burden and demographic distribution of psychiatric conditions among adults with IBS.
Methods: We conducted a retrospective analysis of de-identified electronic health records from 100 U.S. healthcare organizations in the TriNetX Research Network from Jan 1, 2015 to Apr 28, 2025. Adults ≥18 years with ≥1 ICD-10-CM diagnosis of IBS (K58.0–K58.9) were included. Psychiatric comorbidities were identified using the following ICD-10-CM codes: major depressive disorder (F32, F33), generalized anxiety disorder (F41.1), bipolar disorder (F31), schizophrenia-spectrum disorders (F20–F29), post-traumatic stress disorder (F43.1), and obsessive-compulsive disorder (F42). Outcomes included incidence, prevalence, peak age range, and stratification by sex and race/ethnicity.
Results: Among 1,275,194 adults with IBS (mean age 45 ± 17 years; 67% female), the most common psychiatric comorbidities were MDD (prevalence: 38.3%) and GAD (17.9%), followed by PTSD (5.6%), BPD (5.5%), OCD (1.9%), and lastly schizophrenia (0.8%). Females exhibited a greater psychiatric burden across nearly all diagnoses, including MDD (41.6% vs. 27.6%), GAD (19.1% vs. 13.5%),BPD ( 5.9% vs 3.9%), OCD (1.93% vs. 1.74%) and PTSD (6.2% vs. 3.8%). Native Hawaiian/Pacific Islander had the highest prevalence of MDD (51.6%), GAD (61.7%) and American Indian/Alaska Native patients had the highest prevalence of BPD(9.7%), OCD(2.8%) and PTSD (14.8%) whereas Black or African-American population had the highest prevalence of schizophrenia (2.1%). Asian patients consistently had the lowest prevalence across all psychiatric conditions.
Discussion: In this nationwide real-world cohort more than half of adults with IBS carried at least one psychiatric diagnosis, most commonly MDD and GAD with markedly higher burdens in women and in several under-represented minority populations.These findings underscore the importance of routine mental-health screening and culturally tailored, integrated care pathways for patients with IBS, particularly for high-risk sex and racial/ethnic groups, to help reduce symptom burden and optimize resource utilization.
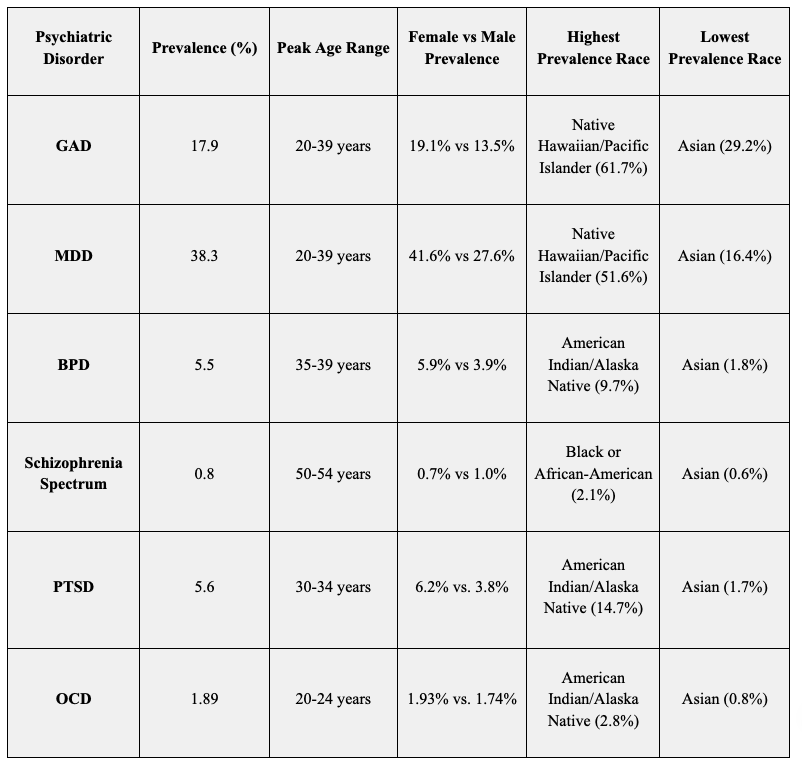
Figure: Table: Psychiatric Comorbidity Trends in Adult IBS Patients Stratified by Age, Sex, and Race/Ethnicity (2015–2025)
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Lana Dardari indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Archana Kharel, MD1, Venkata Sunkesula, MD2, Umesh Bhagat, MD3, Prabhat Kumar, MD4, Lana Dardari, MD5, Gengqing Song, MD, PhD6. P2945 - Understanding the Psychiatric Profile and Sociodemographics of Adults With Irritable Bowel Syndrome: A 10-Year Multicenter Electronic Health Record Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
