Monday Poster Session
Category: Functional Bowel Disease
P2944 - Functional Dyspepsia and Gastroparesis Is Linked to Higher Psychiatric Burden Than Irritable Bowel Syndrome: A Propensity-Matched TriNetX Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Archana Kharel, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Archana Kharel, MD1, Venkata Sunkesula, MD2, Umesh Bhagat, MD3, Basil Jalamneh, MD3, Prabhat Kumar, MD4, Gengqing Song, MD, PhD5
1Cleveland Clinic, Cleveland, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Virginia Commonwealth University, Richmond, VA; 5Case Western Reserve University/Metro Health, Cleveland, OH
Introduction: Although psychiatric comorbidity is recognized in functional gastrointestinal disorders, comparative data for upper-GI dysmotility (functional dyspepsia and gastroparesis; FD/GP) versus irritable bowel syndrome (IBS) are scarce
Methods: We queried the TriNetX Research Network (100 health-care organizations) in May 2025. Adults ≥ 18 years with IBS (ICD-10-CM K58.x) or both FD (K30) and gastroparesis (K31.84) were identified. Index date was the first qualifying diagnosis. Six psychiatric outcomes-major depressive disorder (MDD F32), generalized anxiety disorder (GAD F41), bipolar disorder (BPD F31),schizophrenia-spectrum disorders (F20/F20-F29), obsessive-compulsive disorder (OCD F42) and post-traumatic stress disorder (PTSD F43.1) were assessed beginning 1 day post-index. 1:1 propensity-score matching was done with balanced demographics, race/ethnicity, central nervous system and gastrointestinal medication classes, and endoscopy exposure. Risk ratios (RR), absolute risk differences (ARD) and Kaplan–Meier hazard ratios (HR) were calculated.
Results: After matching, 37,872 patients with FD/GP were compared to an equal number of IBS patients with excellent covariate balance. FD/GP patients experienced significantly higher rates of psychiatric disorders: MDD (38.7% vs. 27.7%; RR 1.40, 95% CI 1.37–1.43), GAD (43.3% vs. 37.6%; RR 1.15, 1.13–1.17), BPD (6.0% vs. 4.6%; RR 1.30, 1.22–1.38), schizophrenia (3.6% vs. 2.2%; RR 1.64, 1.49–1.80), PTSD (10.2% vs. 6.7%), and OCD (2.9% vs. 2.2%).OCD was least common among both the groups.Time-to-event analysis showed earlier psychiatric diagnosis in FD/GP, including MDD (median: 2,518 vs. 5,323 days; HR 1.56) and GAD (1,785 vs. 2,582 days; HR 1.23). For schizophrenia and BPD, median survival times were not reached, but hazard ratios remained elevated (HRs ≈1.3–1.7).
Discussion: Patients with FD/GP carry a substantially greater and earlier psychiatric burden compared to those with IBS, including elevated risks of PTSD and OCD. These findings support routine mental health screening and integrated behavioral care in upper GI dysmotility syndromes.
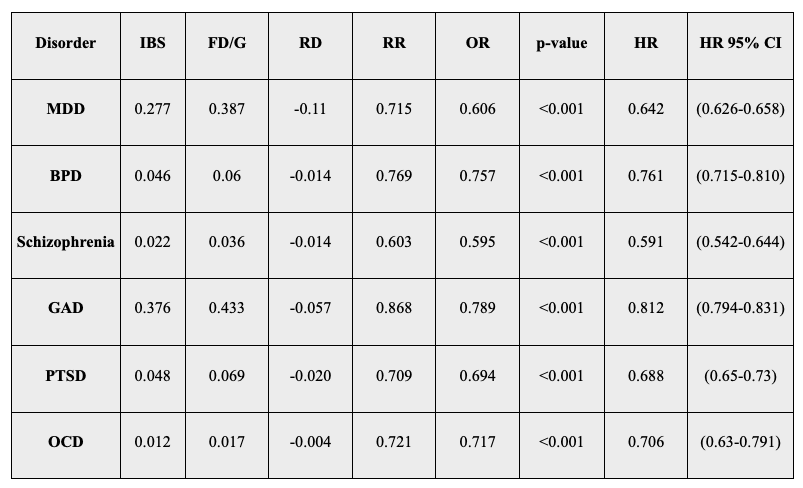
Figure: Table 1. Risk of Psychiatric Disorders in IBS vs FD/GP Cohorts After Propensity Score Matching.
IBS patients had consistently lower risk and hazard of major psychiatric disorders—including MDD, GAD, BPD, schizophrenia, PTSD, and OCD—compared to matched FD/GP patients. All between-group differences were statistically significant (p < 0.001).
Abbreviations: MDD – Major Depressive Disorder; GAD – Generalized Anxiety Disorder; BPD – Bipolar Disorder; PTSD – Post-Traumatic Stress Disorder; OCD – Obsessive-Compulsive Disorder; RD – Risk Difference; RR – Risk Ratio; OR – Odds Ratio; HR – Hazard Ratio; CI – Confidence Interval; FD/GP – Functional Dyspepsia and Gastroparesis; IBS – Irritable Bowel Syndrome.
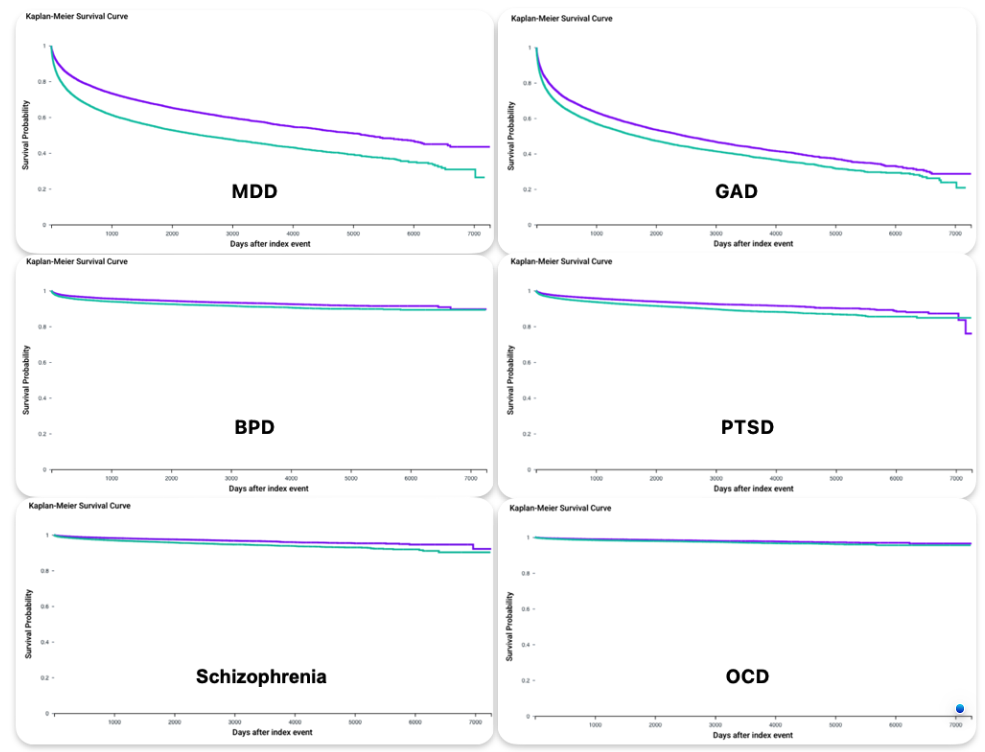
Figure: Figure: Kaplan–Meier Survival Curves Comparing Time to Psychiatric Diagnosis in IBS vs. FD/GP Cohorts.
Each panel displays survival probability over time for a specific psychiatric outcome. Across all conditions—MDD, GAD, BPD, schizophrenia, PTSD, and OCD—IBS patients (green) consistently demonstrated longer time-to-event and higher survival probabilities compared to matched FD/GP patients (purple). All comparisons were statistically significant (log-rank p < 0.001).
Abbreviations:
MDD – Major Depressive Disorder; GAD – Generalized Anxiety Disorder; BPD – Bipolar Disorder; PTSD – Post-Traumatic Stress Disorder; OCD – Obsessive-Compulsive Disorder; FD/GP – Functional Dyspepsia and Gastroparesis; IBS – Irritable Bowel Syndrome
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Basil Jalamneh indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Archana Kharel, MD1, Venkata Sunkesula, MD2, Umesh Bhagat, MD3, Basil Jalamneh, MD3, Prabhat Kumar, MD4, Gengqing Song, MD, PhD5. P2944 - Functional Dyspepsia and Gastroparesis Is Linked to Higher Psychiatric Burden Than Irritable Bowel Syndrome: A Propensity-Matched TriNetX Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Virginia Commonwealth University, Richmond, VA; 5Case Western Reserve University/Metro Health, Cleveland, OH
Introduction: Although psychiatric comorbidity is recognized in functional gastrointestinal disorders, comparative data for upper-GI dysmotility (functional dyspepsia and gastroparesis; FD/GP) versus irritable bowel syndrome (IBS) are scarce
Methods: We queried the TriNetX Research Network (100 health-care organizations) in May 2025. Adults ≥ 18 years with IBS (ICD-10-CM K58.x) or both FD (K30) and gastroparesis (K31.84) were identified. Index date was the first qualifying diagnosis. Six psychiatric outcomes-major depressive disorder (MDD F32), generalized anxiety disorder (GAD F41), bipolar disorder (BPD F31),schizophrenia-spectrum disorders (F20/F20-F29), obsessive-compulsive disorder (OCD F42) and post-traumatic stress disorder (PTSD F43.1) were assessed beginning 1 day post-index. 1:1 propensity-score matching was done with balanced demographics, race/ethnicity, central nervous system and gastrointestinal medication classes, and endoscopy exposure. Risk ratios (RR), absolute risk differences (ARD) and Kaplan–Meier hazard ratios (HR) were calculated.
Results: After matching, 37,872 patients with FD/GP were compared to an equal number of IBS patients with excellent covariate balance. FD/GP patients experienced significantly higher rates of psychiatric disorders: MDD (38.7% vs. 27.7%; RR 1.40, 95% CI 1.37–1.43), GAD (43.3% vs. 37.6%; RR 1.15, 1.13–1.17), BPD (6.0% vs. 4.6%; RR 1.30, 1.22–1.38), schizophrenia (3.6% vs. 2.2%; RR 1.64, 1.49–1.80), PTSD (10.2% vs. 6.7%), and OCD (2.9% vs. 2.2%).OCD was least common among both the groups.Time-to-event analysis showed earlier psychiatric diagnosis in FD/GP, including MDD (median: 2,518 vs. 5,323 days; HR 1.56) and GAD (1,785 vs. 2,582 days; HR 1.23). For schizophrenia and BPD, median survival times were not reached, but hazard ratios remained elevated (HRs ≈1.3–1.7).
Discussion: Patients with FD/GP carry a substantially greater and earlier psychiatric burden compared to those with IBS, including elevated risks of PTSD and OCD. These findings support routine mental health screening and integrated behavioral care in upper GI dysmotility syndromes.
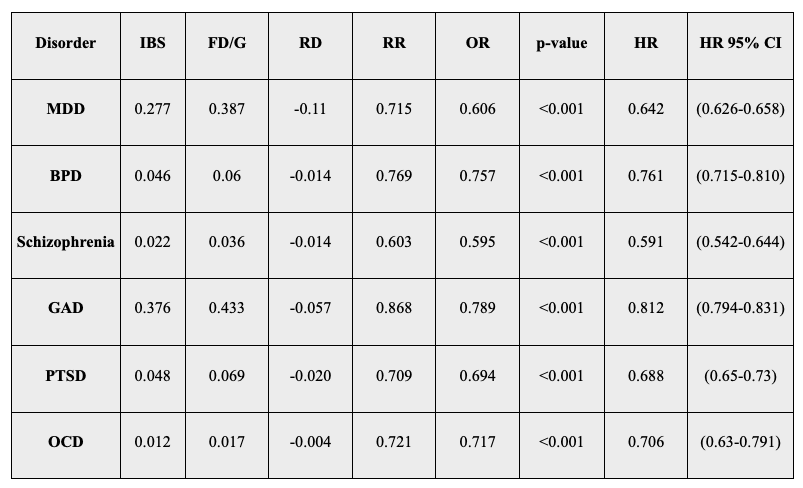
Figure: Table 1. Risk of Psychiatric Disorders in IBS vs FD/GP Cohorts After Propensity Score Matching.
IBS patients had consistently lower risk and hazard of major psychiatric disorders—including MDD, GAD, BPD, schizophrenia, PTSD, and OCD—compared to matched FD/GP patients. All between-group differences were statistically significant (p < 0.001).
Abbreviations: MDD – Major Depressive Disorder; GAD – Generalized Anxiety Disorder; BPD – Bipolar Disorder; PTSD – Post-Traumatic Stress Disorder; OCD – Obsessive-Compulsive Disorder; RD – Risk Difference; RR – Risk Ratio; OR – Odds Ratio; HR – Hazard Ratio; CI – Confidence Interval; FD/GP – Functional Dyspepsia and Gastroparesis; IBS – Irritable Bowel Syndrome.
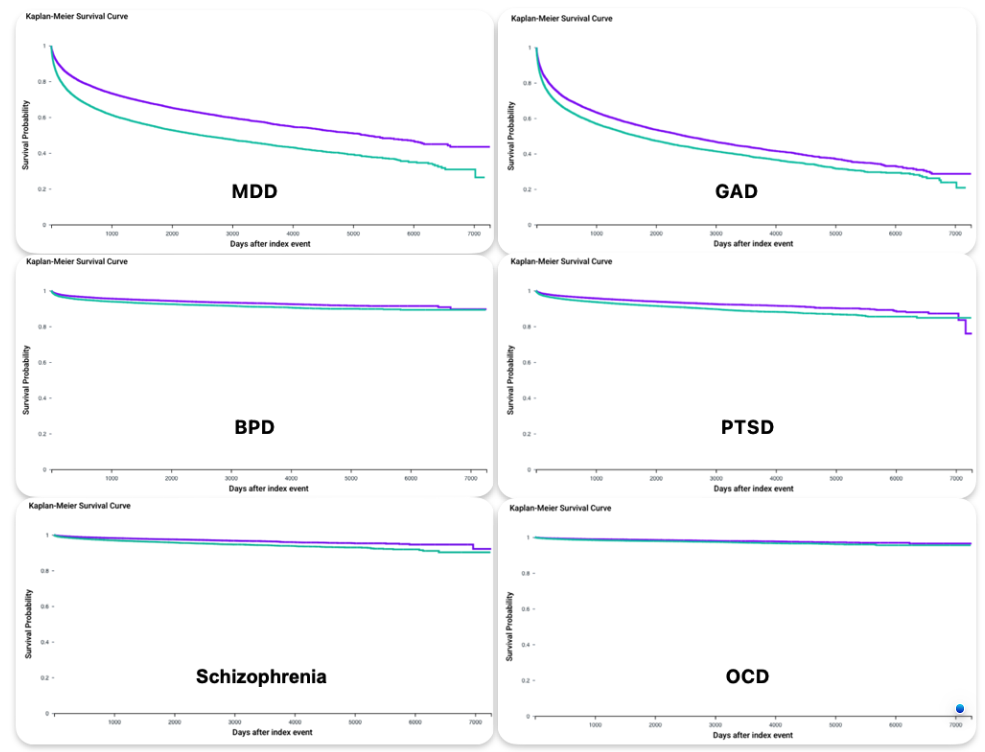
Figure: Figure: Kaplan–Meier Survival Curves Comparing Time to Psychiatric Diagnosis in IBS vs. FD/GP Cohorts.
Each panel displays survival probability over time for a specific psychiatric outcome. Across all conditions—MDD, GAD, BPD, schizophrenia, PTSD, and OCD—IBS patients (green) consistently demonstrated longer time-to-event and higher survival probabilities compared to matched FD/GP patients (purple). All comparisons were statistically significant (log-rank p < 0.001).
Abbreviations:
MDD – Major Depressive Disorder; GAD – Generalized Anxiety Disorder; BPD – Bipolar Disorder; PTSD – Post-Traumatic Stress Disorder; OCD – Obsessive-Compulsive Disorder; FD/GP – Functional Dyspepsia and Gastroparesis; IBS – Irritable Bowel Syndrome
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Basil Jalamneh indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Archana Kharel, MD1, Venkata Sunkesula, MD2, Umesh Bhagat, MD3, Basil Jalamneh, MD3, Prabhat Kumar, MD4, Gengqing Song, MD, PhD5. P2944 - Functional Dyspepsia and Gastroparesis Is Linked to Higher Psychiatric Burden Than Irritable Bowel Syndrome: A Propensity-Matched TriNetX Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
