Monday Poster Session
Category: Functional Bowel Disease
P2941 - Parkinson’s Disease and Inpatient Outcomes Among Adults Hospitalized With Constipation: A Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anwar Uddin, MD (he/him/his)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Anwar Uddin, MD, Madia Ahad, MD, Peter Lymberopoulos, MD, Aisha Elamin, MD, Savanna Thor, DO, MPH
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Constipation is a frequent non-motor manifestation of Parkinson’s disease (PD), linked to autonomic dysfunction, impaired colonic transit, and neuromuscular degeneration. While the association is well recognized in outpatient settings, the impact of PD on hospitalization outcomes among adults admitted with constipation remains underexplored. This study aimed to evaluate inpatient outcomes in hospitalized patients with constipation, stratified by the presence of comorbid Parkinson’s disease.
Methods: We analyzed adult hospitalizations (≥18 years) with constipation (ICD-10-CM K59.00–K59.09) using the National Inpatient Sample (2016–2020). Parkinson’s disease was identified via ICD-10-CM codes G20, G21.0, G21.11, G21.19, G21.8, and G21.9. Outcomes included mortality, LOS, costs, bowel obstruction, electrolyte derangements, urinary retention, delirium, pressure ulcers, and sepsis. Multivariable logistic regression adjusted for age, sex, race, and Charlson Comorbidity Index. Costs were modeled using gamma regression with log-link and adjusted to 2020 USD by the Consumer Price Index.
Results: Among the included patients, those with PD had higher in-hospital mortality (0.9% vs 0.6%, OR 1.15; 95% CI 0.97–1.36), though this was not statistically significant. Length of stay was significantly longer in the PD group (6.2 vs 5.6 days, OR 1.14; 95% CI 1.11–1.16), while hospital costs were lower ($12,768.4 vs $14,099.8, OR 0.92; 95% CI 0.91–0.94). Patients with PD were more likely to experience acute urinary retention (9.0% vs 5.1%, OR 1.22; 95% CI 1.15–1.30), delirium (2.4% vs 0.7%, OR 2.23; 95% CI 1.99–2.49), and pressure ulcers (3.7% vs 1.6%, OR 1.98; 95% CI 1.80–2.17). Sepsis rates were modestly increased (6.0% vs 5.5%, OR 1.09; 95% CI 1.02–1.17). Electrolyte derangements were less common in the PD group (19% vs 22%, OR 0.80; 95% CI 0.77–0.83). There was also a trend toward decreased rates of bowel obstruction (0.3% vs 0.4%, OR 0.75; 95% CI 0.56–1.00), though this did not reach statistical significance as the confidence interval included 1.
Discussion: Adults hospitalized with constipation and comorbid Parkinson’s disease experienced longer stays and greater risks of delirium, urinary retention, pressure ulcers, and sepsis. Despite these complications, they had lower hospitalization costs and reduced odds of bowel obstruction and electrolyte abnormalities. Further study is needed to guide inpatient care strategies in this medically complex population.
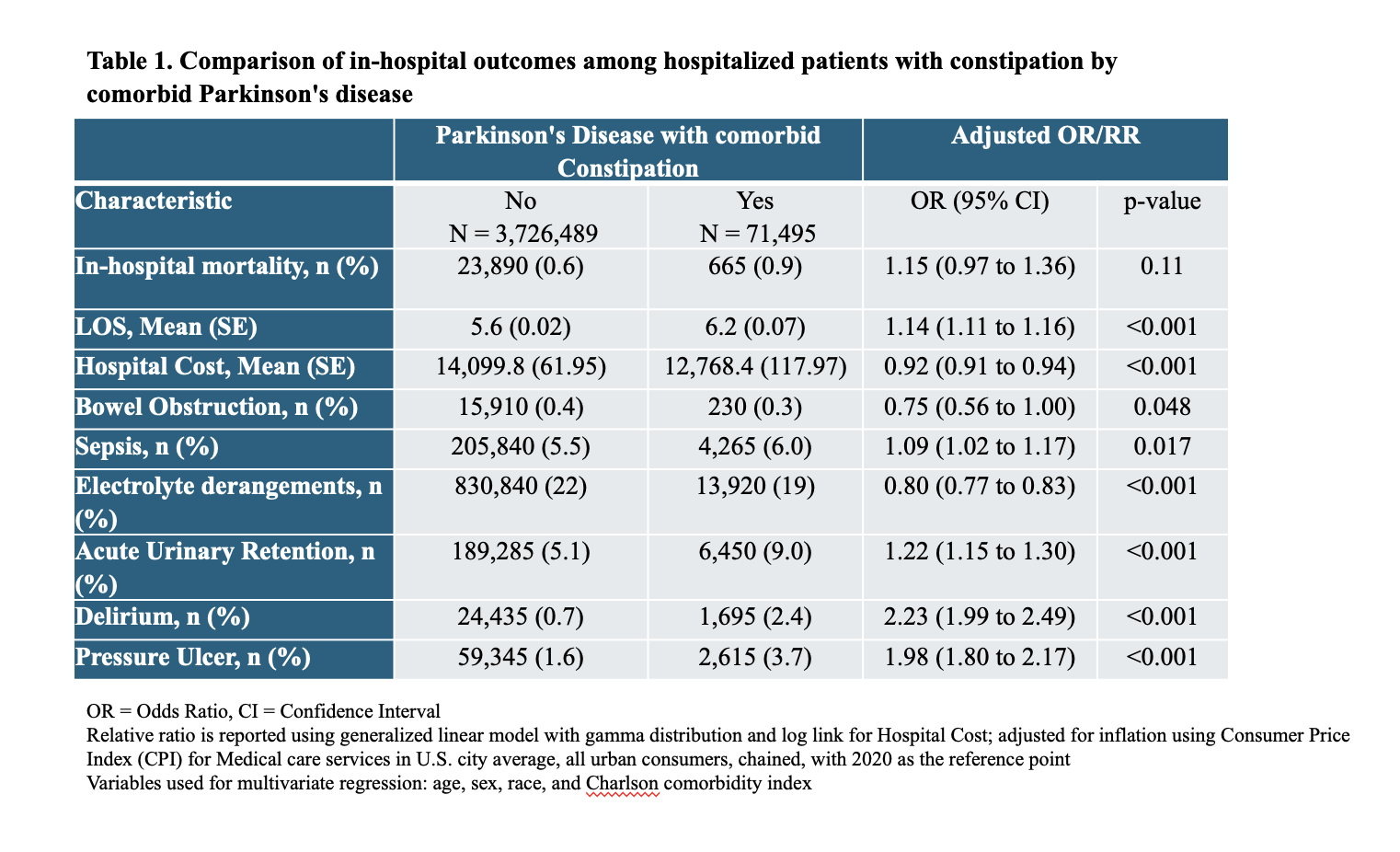
Figure: Table 1: Comparison of in-hospital outcomes among hospitalized patients with constipation by comorbid Parkinson's disease
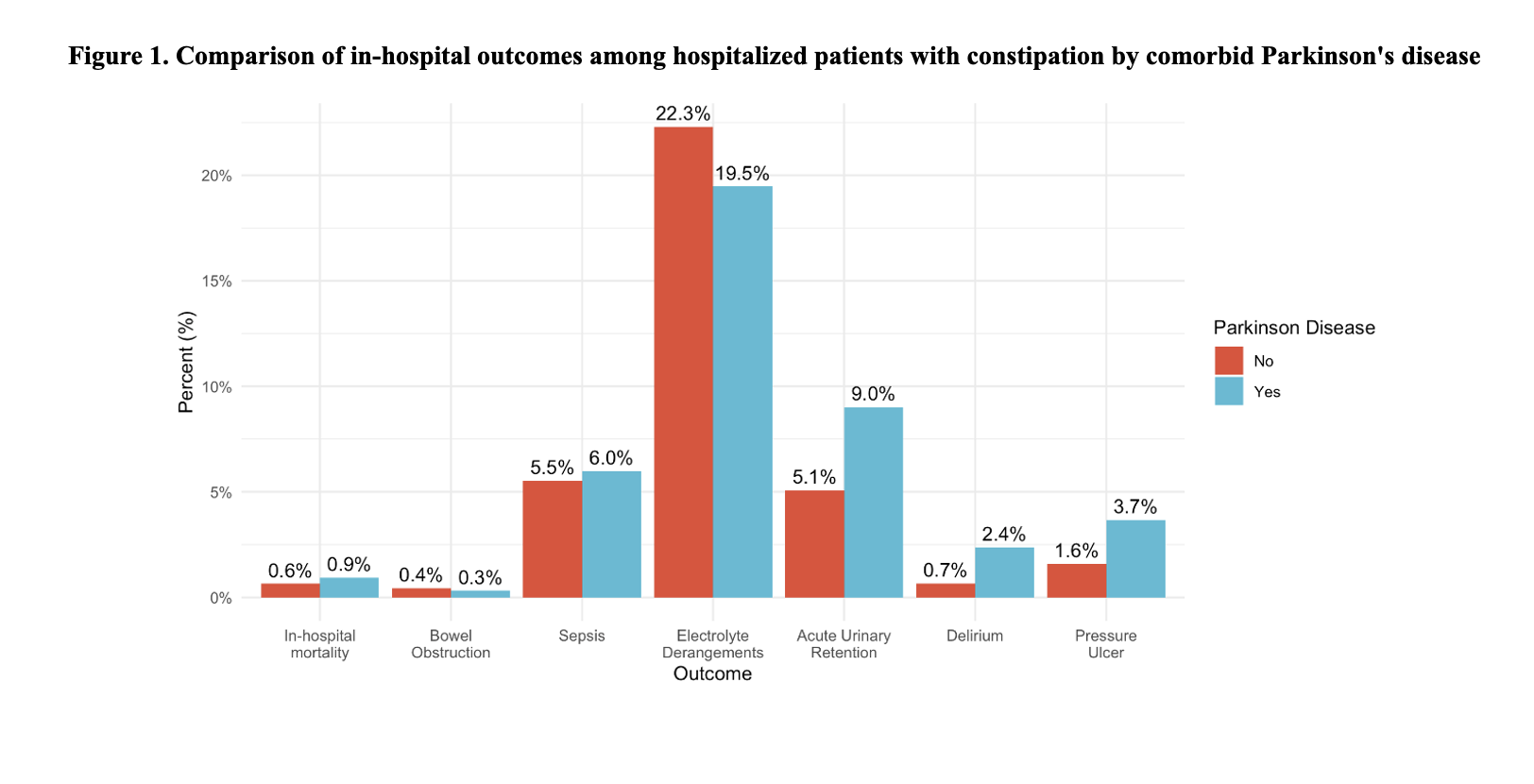
Figure: Figure 1: Bar Chart of in-hospital outcomes among hospitalized patients with constipation by comorbid Parkinson's disease
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Aisha Elamin indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Peter Lymberopoulos, MD, Aisha Elamin, MD, Savanna Thor, DO, MPH. P2941 - Parkinson’s Disease and Inpatient Outcomes Among Adults Hospitalized With Constipation: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Constipation is a frequent non-motor manifestation of Parkinson’s disease (PD), linked to autonomic dysfunction, impaired colonic transit, and neuromuscular degeneration. While the association is well recognized in outpatient settings, the impact of PD on hospitalization outcomes among adults admitted with constipation remains underexplored. This study aimed to evaluate inpatient outcomes in hospitalized patients with constipation, stratified by the presence of comorbid Parkinson’s disease.
Methods: We analyzed adult hospitalizations (≥18 years) with constipation (ICD-10-CM K59.00–K59.09) using the National Inpatient Sample (2016–2020). Parkinson’s disease was identified via ICD-10-CM codes G20, G21.0, G21.11, G21.19, G21.8, and G21.9. Outcomes included mortality, LOS, costs, bowel obstruction, electrolyte derangements, urinary retention, delirium, pressure ulcers, and sepsis. Multivariable logistic regression adjusted for age, sex, race, and Charlson Comorbidity Index. Costs were modeled using gamma regression with log-link and adjusted to 2020 USD by the Consumer Price Index.
Results: Among the included patients, those with PD had higher in-hospital mortality (0.9% vs 0.6%, OR 1.15; 95% CI 0.97–1.36), though this was not statistically significant. Length of stay was significantly longer in the PD group (6.2 vs 5.6 days, OR 1.14; 95% CI 1.11–1.16), while hospital costs were lower ($12,768.4 vs $14,099.8, OR 0.92; 95% CI 0.91–0.94). Patients with PD were more likely to experience acute urinary retention (9.0% vs 5.1%, OR 1.22; 95% CI 1.15–1.30), delirium (2.4% vs 0.7%, OR 2.23; 95% CI 1.99–2.49), and pressure ulcers (3.7% vs 1.6%, OR 1.98; 95% CI 1.80–2.17). Sepsis rates were modestly increased (6.0% vs 5.5%, OR 1.09; 95% CI 1.02–1.17). Electrolyte derangements were less common in the PD group (19% vs 22%, OR 0.80; 95% CI 0.77–0.83). There was also a trend toward decreased rates of bowel obstruction (0.3% vs 0.4%, OR 0.75; 95% CI 0.56–1.00), though this did not reach statistical significance as the confidence interval included 1.
Discussion: Adults hospitalized with constipation and comorbid Parkinson’s disease experienced longer stays and greater risks of delirium, urinary retention, pressure ulcers, and sepsis. Despite these complications, they had lower hospitalization costs and reduced odds of bowel obstruction and electrolyte abnormalities. Further study is needed to guide inpatient care strategies in this medically complex population.
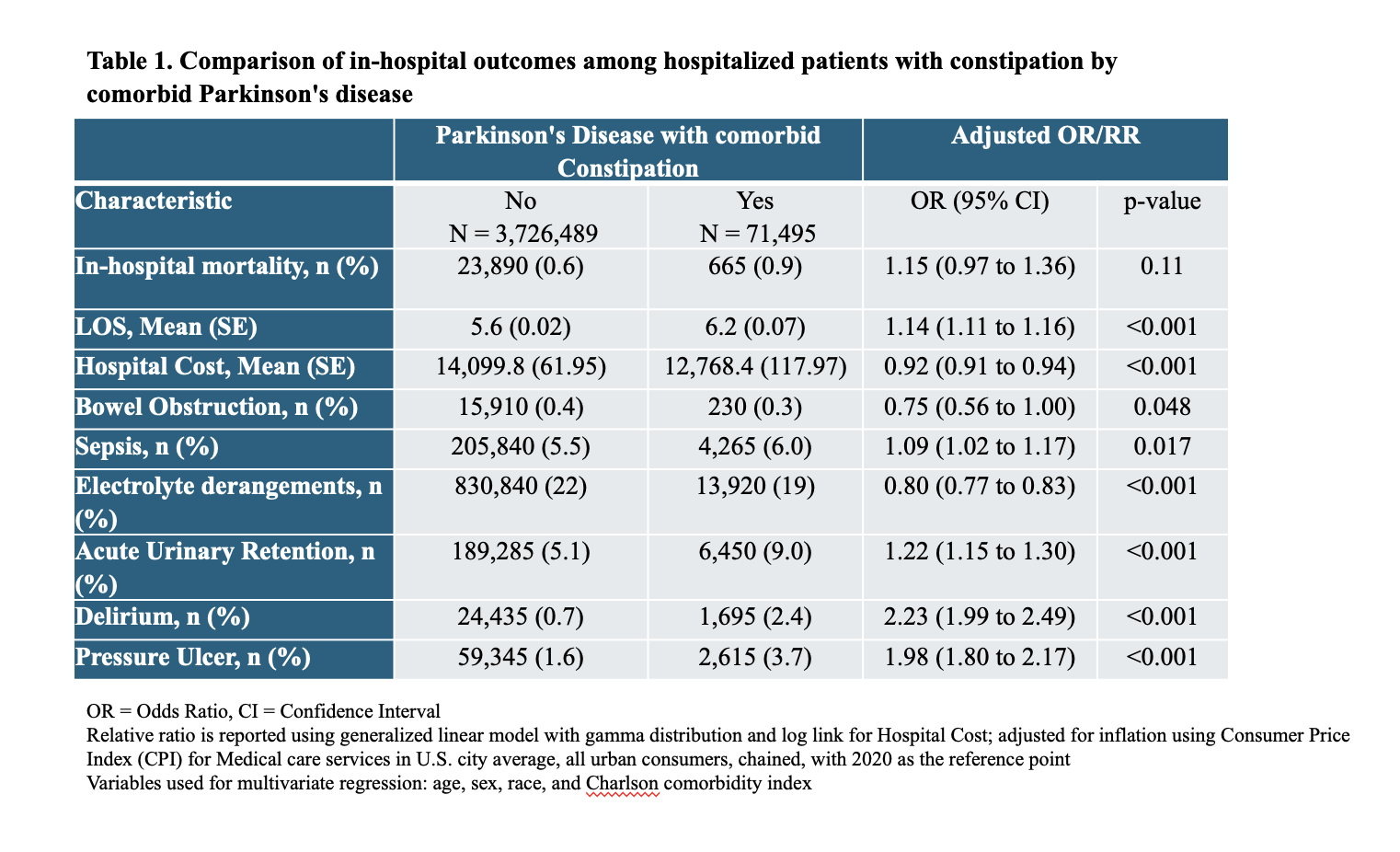
Figure: Table 1: Comparison of in-hospital outcomes among hospitalized patients with constipation by comorbid Parkinson's disease
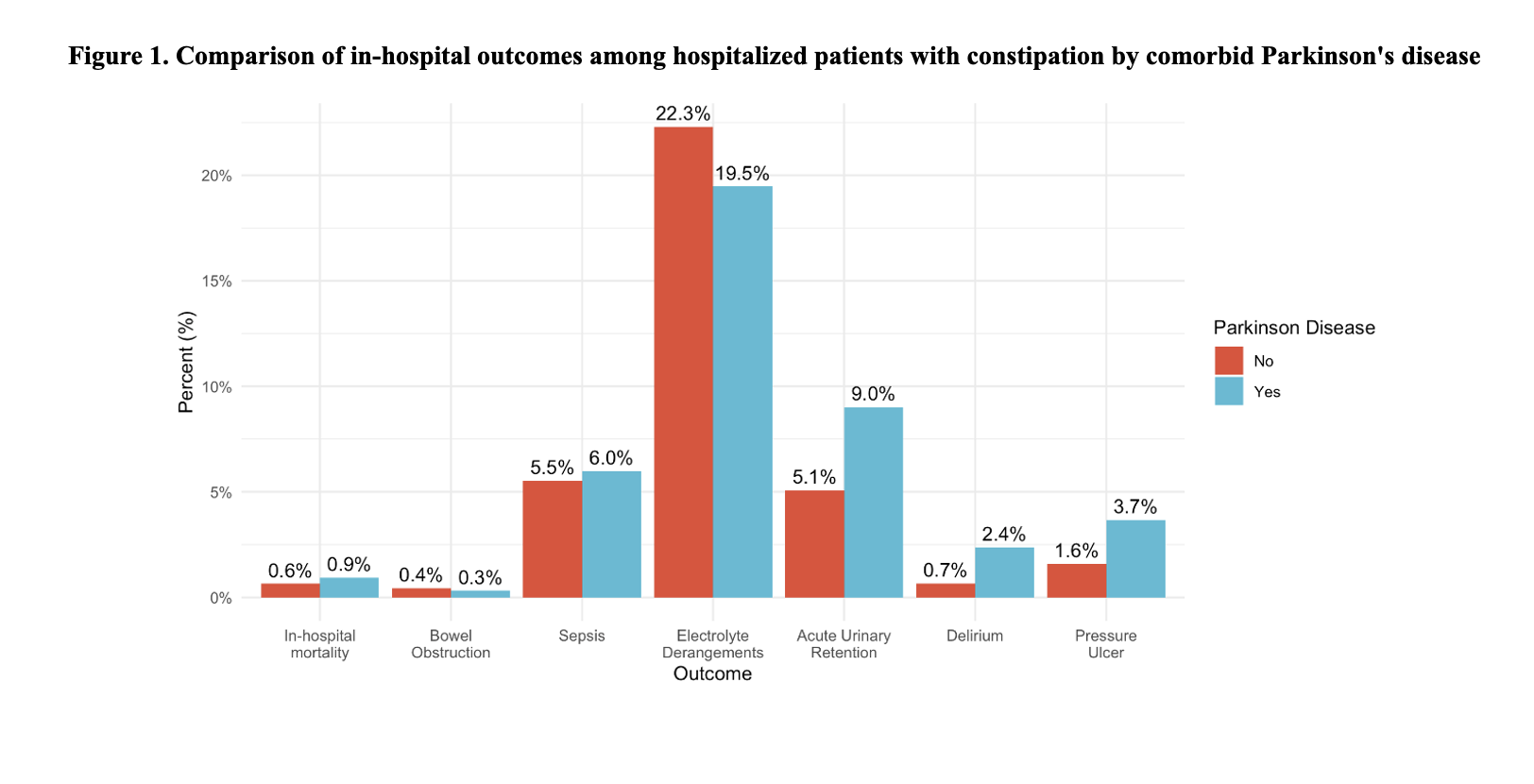
Figure: Figure 1: Bar Chart of in-hospital outcomes among hospitalized patients with constipation by comorbid Parkinson's disease
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Aisha Elamin indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Peter Lymberopoulos, MD, Aisha Elamin, MD, Savanna Thor, DO, MPH. P2941 - Parkinson’s Disease and Inpatient Outcomes Among Adults Hospitalized With Constipation: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
