Monday Poster Session
Category: Functional Bowel Disease
P2930 - Outcomes of Patients Hospitalized for Spontaneous Bacterial Peritonitis with Comorbid Irritable Bowel Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexander J. Kaye, MD (he/him/his)
SUNY Downstate Health Sciences University, NY
Presenting Author(s)
Alexander J. Kaye, MD, MBA1, Kariana Martinez, MD2, Narinderjeet Kaur, MD, MS2, Anwar Uddin, MD2, Andrew Draheim, BS2, Bani Chander-Roland, MD3, Daniel DiLeo, MD3
1SUNY Downstate Health Sciences University, Staten Island, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Brooklyn VA Medical Center, Brooklyn, NY
Introduction: Spontaneous bacterial peritonitis (SBP) is a common reason for hospitalization in cirrhotic patients with an associated 30-day mortality rate of 10.8%. The bacterial source for SBP is from the gastrointestinal tract. IBS is a highly prevalent disorder impacting about 11% of patients globally. Studies have demonstrated that IBS may be associated with a higher prevalence of pro-inflammatory bacteria within the gut microbiome. While IBS has been associated with alterations in the gut microflora, its subsequent impact on cirrhotic patients is not well explored. Our study aim is to understand the impact of comorbid IBS on the outcomes of hospitalized patients with SBP.
Methods: Hospitalized adults diagnosed with SBP were selected from the 2020 National Inpatient Sample database. ICD-10 codes were used to select diagnoses. Demographic data and outcomes of SBP were compared between a subgroup with IBS, and without IBS. The outcomes of interest were sepsis, acute renal failure (AKI), acute respiratory failure, hypotension/shock, and inpatient mortality. Chi-squared tests and independent t-tests were used to compare proportions and means respectively. A multivariate logistic regression analysis was used to establish if IBS is an independent predictor for the outcomes after adjusting for age, sex, race, and Charlson Comorbidity Index (CCI).
Results: For the year 2020, 811,930 hospitalized adults were diagnosed with SBP. Patients with SBP and comorbid IBS were more likely to be female (74% vs 47%, p< 0.001), more likely to be white (83% vs 67%, p< 0.001), have a shorter length of stay (9.7 days vs. 11.5 days, p< 0.001), lower hospitalization cost ($29,817 vs. $38,195, p< 0.001), and a lower CCI (2.0 vs 2.6, p< 0.001). There was no significant difference in age (58.7 vs. 59.3, p=0.138). IBS was noted to be an independent protective factor for inpatient mortality (adjusted odds ratio (aOR) 0.60, 95% confidence interval (CI): 0.49-0.75, p< 0.001), sepsis (aOR 0.72, 95% CI: 0.65-0.81, p< 0.001), hypotension/shock (aOR 0.80, 95% CI: 0.66-0.97, p=0.022), acute respiratory failure (aOR 0.67, 95% CI: 0.57-0.77, p< 0.001) and AKI (aOR 0.74, 95% CI: 0.65-0.83), p< 0.001).
Discussion: In hospitalized adults with SBP, our study demonstrates that IBS is a protective a risk factor for sepsis, hypotension/shock, AKI, acute respiratory failure and inpatient mortality. Further randomized studies are needed to evaluate whether this association is due to differences in gut microbiome or other factors.
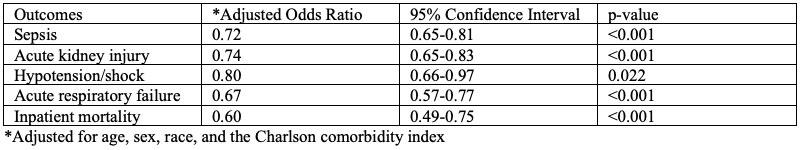
Figure: Multivariate logistic regression analysis of clinical outcomes among Spontaneous Bacterial Peritonitis With Comorbid Irritable Bowel Syndrome
Disclosures:
Alexander Kaye indicated no relevant financial relationships.
Kariana Martinez indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Anwar Uddin indicated no relevant financial relationships.
Andrew Draheim indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Alexander J. Kaye, MD, MBA1, Kariana Martinez, MD2, Narinderjeet Kaur, MD, MS2, Anwar Uddin, MD2, Andrew Draheim, BS2, Bani Chander-Roland, MD3, Daniel DiLeo, MD3. P2930 - Outcomes of Patients Hospitalized for Spontaneous Bacterial Peritonitis with Comorbid Irritable Bowel Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Staten Island, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Brooklyn VA Medical Center, Brooklyn, NY
Introduction: Spontaneous bacterial peritonitis (SBP) is a common reason for hospitalization in cirrhotic patients with an associated 30-day mortality rate of 10.8%. The bacterial source for SBP is from the gastrointestinal tract. IBS is a highly prevalent disorder impacting about 11% of patients globally. Studies have demonstrated that IBS may be associated with a higher prevalence of pro-inflammatory bacteria within the gut microbiome. While IBS has been associated with alterations in the gut microflora, its subsequent impact on cirrhotic patients is not well explored. Our study aim is to understand the impact of comorbid IBS on the outcomes of hospitalized patients with SBP.
Methods: Hospitalized adults diagnosed with SBP were selected from the 2020 National Inpatient Sample database. ICD-10 codes were used to select diagnoses. Demographic data and outcomes of SBP were compared between a subgroup with IBS, and without IBS. The outcomes of interest were sepsis, acute renal failure (AKI), acute respiratory failure, hypotension/shock, and inpatient mortality. Chi-squared tests and independent t-tests were used to compare proportions and means respectively. A multivariate logistic regression analysis was used to establish if IBS is an independent predictor for the outcomes after adjusting for age, sex, race, and Charlson Comorbidity Index (CCI).
Results: For the year 2020, 811,930 hospitalized adults were diagnosed with SBP. Patients with SBP and comorbid IBS were more likely to be female (74% vs 47%, p< 0.001), more likely to be white (83% vs 67%, p< 0.001), have a shorter length of stay (9.7 days vs. 11.5 days, p< 0.001), lower hospitalization cost ($29,817 vs. $38,195, p< 0.001), and a lower CCI (2.0 vs 2.6, p< 0.001). There was no significant difference in age (58.7 vs. 59.3, p=0.138). IBS was noted to be an independent protective factor for inpatient mortality (adjusted odds ratio (aOR) 0.60, 95% confidence interval (CI): 0.49-0.75, p< 0.001), sepsis (aOR 0.72, 95% CI: 0.65-0.81, p< 0.001), hypotension/shock (aOR 0.80, 95% CI: 0.66-0.97, p=0.022), acute respiratory failure (aOR 0.67, 95% CI: 0.57-0.77, p< 0.001) and AKI (aOR 0.74, 95% CI: 0.65-0.83), p< 0.001).
Discussion: In hospitalized adults with SBP, our study demonstrates that IBS is a protective a risk factor for sepsis, hypotension/shock, AKI, acute respiratory failure and inpatient mortality. Further randomized studies are needed to evaluate whether this association is due to differences in gut microbiome or other factors.
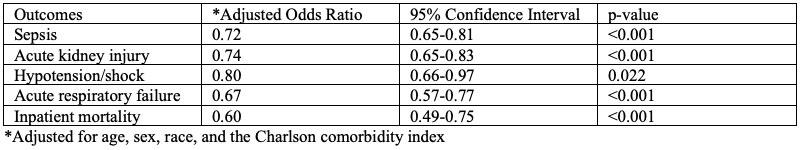
Figure: Multivariate logistic regression analysis of clinical outcomes among Spontaneous Bacterial Peritonitis With Comorbid Irritable Bowel Syndrome
Disclosures:
Alexander Kaye indicated no relevant financial relationships.
Kariana Martinez indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Anwar Uddin indicated no relevant financial relationships.
Andrew Draheim indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Alexander J. Kaye, MD, MBA1, Kariana Martinez, MD2, Narinderjeet Kaur, MD, MS2, Anwar Uddin, MD2, Andrew Draheim, BS2, Bani Chander-Roland, MD3, Daniel DiLeo, MD3. P2930 - Outcomes of Patients Hospitalized for Spontaneous Bacterial Peritonitis with Comorbid Irritable Bowel Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
