Monday Poster Session
Category: Functional Bowel Disease
P2929 - Outcomes of Patients Hospitalized for Hyperemesis Gravidarum with Comorbid Depression
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexander J. Kaye, MD (he/him/his)
SUNY Downstate Health Sciences University, NY
Presenting Author(s)
Alexander J. Kaye, MD, MBA1, Sarah R. Meyers, DO2, Selome Yewedalsew, MD3, Anwar Uddin, MD3, Elizabeth Kaye, AB4, Daniel DiLeo, MD5, Bani Chander-Roland, MD5
1SUNY Downstate Health Sciences University, Staten Island, NY; 2Robert Wood Johnson Medical School, Rutgers University, Piscataway, NJ; 3SUNY Downstate Health Sciences University, Brooklyn, NY; 4McLean Hospital, Boston, MA; 5Brooklyn VA Medical Center, Brooklyn, NY
Introduction: Hyperemesis gravidarum (HG) is a common reason for hospitalization for pregnant women. HG is associated with complications including suicidal ideation and elective termination of a desired pregnancy. Antenatal depression can impact 20% of pregnancies. Prior literature has identified an association between depression and adverse medical outcomes of inpatients including elevated risk of inpatient mortality and increased readmission risk. However, these studies were not specific to pregnant patients. Despite the prevalence of antenatal depression and HG, there is a paucity of literature exploring their relationship. Our study aims to understand the impact of comorbid depression on the outcomes of hospitalized HG patients.
Methods: Hospitalized adults diagnosed with HG were selected from the 2020 National Inpatient Sample database. ICD-10 codes were used to select diagnoses. Demographic data and outcomes for HG were compared between a subgroup with and without depression. The outcomes of interest were length of stay (LOS), hospitalization cost, sepsis, hypotension/shock, acute kidney injury (AKI), acute respiratory failure, and inpatient EGD. Chi-squared tests and independent t-tests were used to compare proportions and means, respectively. A multivariate logistic regression analysis was used to establish if depression is an independent predictor for the outcomes after adjusting for age, sex, race, and Charlson Comorbidity Index (CCI).
Results: For the year 2020, 135,005 hospitalized adults were diagnosed with HG. Patients with HG and comorbid depression were older (27.6 years old vs. 27.1 years old, p< 0.001), more likely to be white (54% vs. 38%, p< 0.001), and have a higher CCI (0.3 vs. 0.2, p< 0.001). All patients were female. Depression was an independent risk factor for inpatient EGD (adjusted odds ratio (aOR) 2.24, 95% confidence interval (CI): 1.41-3.55, p< 0.001), increased LOS (3.9 days vs. 3.0 days, aOR 1.28, 95% CI: 1.21-1.36, p< 0.001), and increased hospitalization cost ($6,982 vs. $5,463, aOR 1.25, CI 1.18-1.33, p< 0.001). Depression was not a risk factor for AKI (p=0.33), acute respiratory failure (p=0.40), sepsis (p=0.055) or hypotension/shock (p=0.62).
Discussion: In hospitalized women with HG, depression is a risk factor for inpatient EGD, increased LOS, and increased hospitalization cost. Further large scale randomized prospective studies are needed to further explore whether treatment for depression can help tailor therapies and mitigate these outcomes.
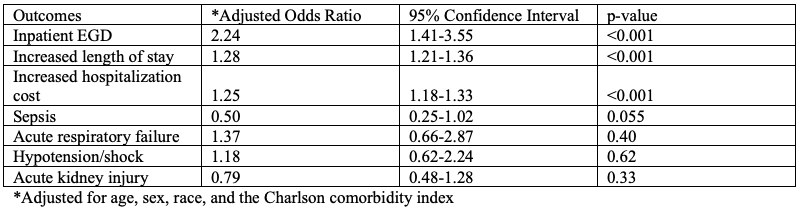
Figure: Multivariate logistic regression analysis of clinical outcomes among hyperemesis gravidarum with comorbid depression
Disclosures:
Alexander Kaye indicated no relevant financial relationships.
Sarah Meyers indicated no relevant financial relationships.
Selome Yewedalsew indicated no relevant financial relationships.
Anwar Uddin indicated no relevant financial relationships.
Elizabeth Kaye indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Alexander J. Kaye, MD, MBA1, Sarah R. Meyers, DO2, Selome Yewedalsew, MD3, Anwar Uddin, MD3, Elizabeth Kaye, AB4, Daniel DiLeo, MD5, Bani Chander-Roland, MD5. P2929 - Outcomes of Patients Hospitalized for Hyperemesis Gravidarum with Comorbid Depression, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Staten Island, NY; 2Robert Wood Johnson Medical School, Rutgers University, Piscataway, NJ; 3SUNY Downstate Health Sciences University, Brooklyn, NY; 4McLean Hospital, Boston, MA; 5Brooklyn VA Medical Center, Brooklyn, NY
Introduction: Hyperemesis gravidarum (HG) is a common reason for hospitalization for pregnant women. HG is associated with complications including suicidal ideation and elective termination of a desired pregnancy. Antenatal depression can impact 20% of pregnancies. Prior literature has identified an association between depression and adverse medical outcomes of inpatients including elevated risk of inpatient mortality and increased readmission risk. However, these studies were not specific to pregnant patients. Despite the prevalence of antenatal depression and HG, there is a paucity of literature exploring their relationship. Our study aims to understand the impact of comorbid depression on the outcomes of hospitalized HG patients.
Methods: Hospitalized adults diagnosed with HG were selected from the 2020 National Inpatient Sample database. ICD-10 codes were used to select diagnoses. Demographic data and outcomes for HG were compared between a subgroup with and without depression. The outcomes of interest were length of stay (LOS), hospitalization cost, sepsis, hypotension/shock, acute kidney injury (AKI), acute respiratory failure, and inpatient EGD. Chi-squared tests and independent t-tests were used to compare proportions and means, respectively. A multivariate logistic regression analysis was used to establish if depression is an independent predictor for the outcomes after adjusting for age, sex, race, and Charlson Comorbidity Index (CCI).
Results: For the year 2020, 135,005 hospitalized adults were diagnosed with HG. Patients with HG and comorbid depression were older (27.6 years old vs. 27.1 years old, p< 0.001), more likely to be white (54% vs. 38%, p< 0.001), and have a higher CCI (0.3 vs. 0.2, p< 0.001). All patients were female. Depression was an independent risk factor for inpatient EGD (adjusted odds ratio (aOR) 2.24, 95% confidence interval (CI): 1.41-3.55, p< 0.001), increased LOS (3.9 days vs. 3.0 days, aOR 1.28, 95% CI: 1.21-1.36, p< 0.001), and increased hospitalization cost ($6,982 vs. $5,463, aOR 1.25, CI 1.18-1.33, p< 0.001). Depression was not a risk factor for AKI (p=0.33), acute respiratory failure (p=0.40), sepsis (p=0.055) or hypotension/shock (p=0.62).
Discussion: In hospitalized women with HG, depression is a risk factor for inpatient EGD, increased LOS, and increased hospitalization cost. Further large scale randomized prospective studies are needed to further explore whether treatment for depression can help tailor therapies and mitigate these outcomes.
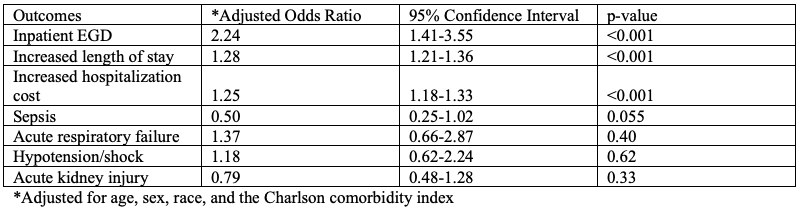
Figure: Multivariate logistic regression analysis of clinical outcomes among hyperemesis gravidarum with comorbid depression
Disclosures:
Alexander Kaye indicated no relevant financial relationships.
Sarah Meyers indicated no relevant financial relationships.
Selome Yewedalsew indicated no relevant financial relationships.
Anwar Uddin indicated no relevant financial relationships.
Elizabeth Kaye indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Alexander J. Kaye, MD, MBA1, Sarah R. Meyers, DO2, Selome Yewedalsew, MD3, Anwar Uddin, MD3, Elizabeth Kaye, AB4, Daniel DiLeo, MD5, Bani Chander-Roland, MD5. P2929 - Outcomes of Patients Hospitalized for Hyperemesis Gravidarum with Comorbid Depression, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
