Monday Poster Session
Category: Functional Bowel Disease
P2923 - Rectal Hyposensitivity on Anorectal Manometry Does Not Distinguish Clinically Significant Structural Disorders Seen on MR Defecography
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Abigail Bacharach, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Abigail Bacharach, MD1, Ahmun Zafar, DO2, Yuying Luo, MD3
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West & Morningside, New York, NY
Introduction: Diagnosis of defecatory disorders is based on two of three concordant tests, anorectal manometry (ARM) with balloon expulsion testing (BET) and defecography, with ARM and BET often being performed first. However, ARM provides limited insight into structural defects that can contribute to defecatory dysfunction compared with MR defecography (MRD). We aimed to evaluate if rectal sensory abnormalities on ARM were associated with structural disorders on MRD.
Methods: We performed a retrospective chart review on consecutive patients who underwent both MRD and ARM for chronic constipation or defecatory complaints in a 5-year period. MRD reports were reviewed for significant findings (compartment prolapse, rectocele, intussusception, peritoneocele, enterocele, sigmoidocele, and paradoxical puborectalis contraction during defecation). ARM data was collected, including resting tone, squeeze, intrarectal pressure, rectoanal pressure differential, percent relaxation, and rectal sensation. Rectal hyposensitivity was defined by age and sex normals and by the London Classification (i.e. two of three thresholds > upper limit of normal is diagnostic of rectal hyposensitivity; one of three thresholds > upper limit of normal is borderline). Findings between both tests were then analyzed for correlation.
Results: 55 patients were reviewed and ultimately 34 patients were included in our cohort (54.3% female, average 55.2 years +/- 17.1 at time of ARM). There was a total of 23 (67.6%) patients with rectoceles (21.7% with grade 1, 73.9% with grade 2, 4.35% with grade 3). There was no correlation between increasing size of rectocele and likelihood of rectal hyposensitivity. Maximum tolerated volume was not detected in 4 patients with rectoceles with all three grades of rectocele represented. Additionally, 8 of the 23 (34.8%) patients with rectoceles had inadequate propulsive force on ARM. For patients with rectal prolapse or intussusception on MRD (n=5), 60% (n=3) had normal sensation and 80% (n=4) had normal rectoanal pressure differential for their age/gender. 57.1% of patients with grade 3 pelvic floor descent (n=4) also had hyposensitivity on ARM.
Discussion: Rectal hyposensitivity on ARM does not predict clinically significant structural disorders on MRD. More research is needed to determine nuanced positioning of ARM versus MR defecography in patients with defecatory symptoms.
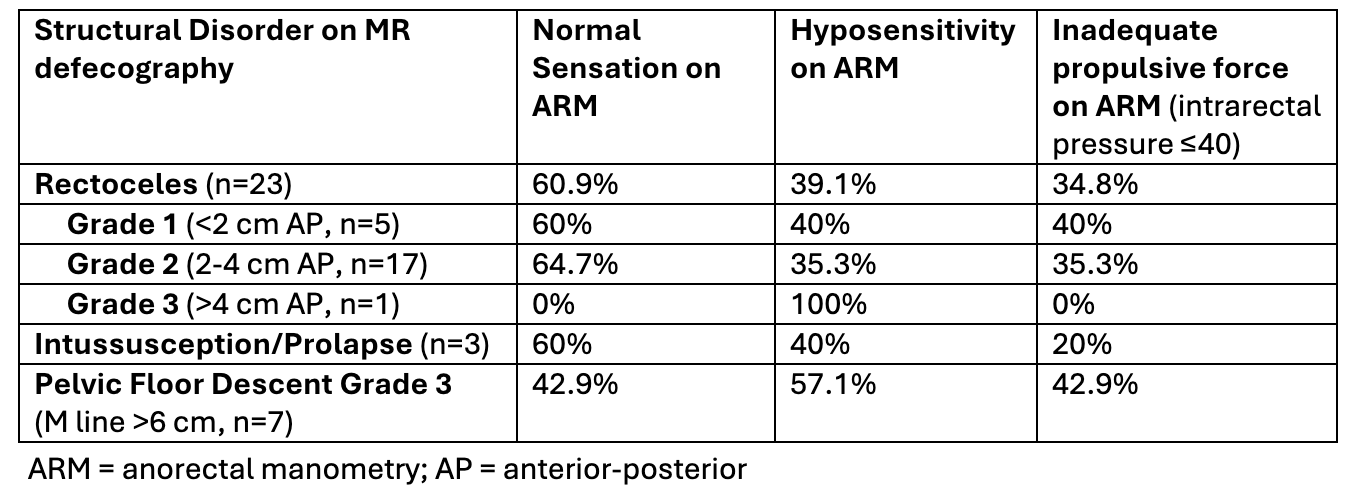
Figure: The correlation between structural disorders identified with MR defecography and certain findings on ARM
Disclosures:
Abigail Bacharach indicated no relevant financial relationships.
Ahmun Zafar indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Abigail Bacharach, MD1, Ahmun Zafar, DO2, Yuying Luo, MD3. P2923 - Rectal Hyposensitivity on Anorectal Manometry Does Not Distinguish Clinically Significant Structural Disorders Seen on MR Defecography, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West & Morningside, New York, NY
Introduction: Diagnosis of defecatory disorders is based on two of three concordant tests, anorectal manometry (ARM) with balloon expulsion testing (BET) and defecography, with ARM and BET often being performed first. However, ARM provides limited insight into structural defects that can contribute to defecatory dysfunction compared with MR defecography (MRD). We aimed to evaluate if rectal sensory abnormalities on ARM were associated with structural disorders on MRD.
Methods: We performed a retrospective chart review on consecutive patients who underwent both MRD and ARM for chronic constipation or defecatory complaints in a 5-year period. MRD reports were reviewed for significant findings (compartment prolapse, rectocele, intussusception, peritoneocele, enterocele, sigmoidocele, and paradoxical puborectalis contraction during defecation). ARM data was collected, including resting tone, squeeze, intrarectal pressure, rectoanal pressure differential, percent relaxation, and rectal sensation. Rectal hyposensitivity was defined by age and sex normals and by the London Classification (i.e. two of three thresholds > upper limit of normal is diagnostic of rectal hyposensitivity; one of three thresholds > upper limit of normal is borderline). Findings between both tests were then analyzed for correlation.
Results: 55 patients were reviewed and ultimately 34 patients were included in our cohort (54.3% female, average 55.2 years +/- 17.1 at time of ARM). There was a total of 23 (67.6%) patients with rectoceles (21.7% with grade 1, 73.9% with grade 2, 4.35% with grade 3). There was no correlation between increasing size of rectocele and likelihood of rectal hyposensitivity. Maximum tolerated volume was not detected in 4 patients with rectoceles with all three grades of rectocele represented. Additionally, 8 of the 23 (34.8%) patients with rectoceles had inadequate propulsive force on ARM. For patients with rectal prolapse or intussusception on MRD (n=5), 60% (n=3) had normal sensation and 80% (n=4) had normal rectoanal pressure differential for their age/gender. 57.1% of patients with grade 3 pelvic floor descent (n=4) also had hyposensitivity on ARM.
Discussion: Rectal hyposensitivity on ARM does not predict clinically significant structural disorders on MRD. More research is needed to determine nuanced positioning of ARM versus MR defecography in patients with defecatory symptoms.
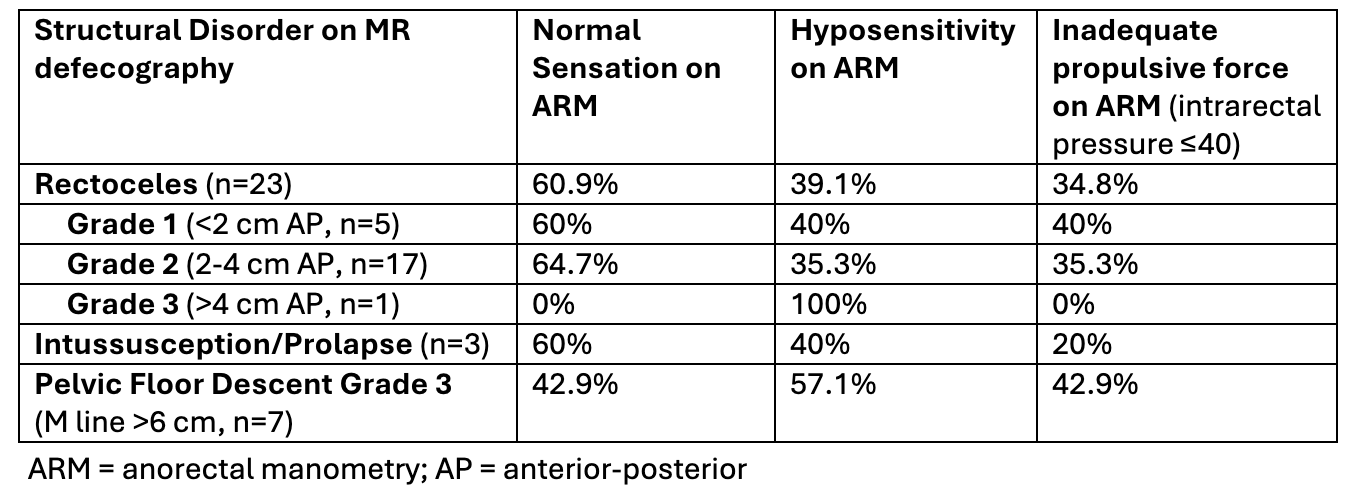
Figure: The correlation between structural disorders identified with MR defecography and certain findings on ARM
Disclosures:
Abigail Bacharach indicated no relevant financial relationships.
Ahmun Zafar indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Abigail Bacharach, MD1, Ahmun Zafar, DO2, Yuying Luo, MD3. P2923 - Rectal Hyposensitivity on Anorectal Manometry Does Not Distinguish Clinically Significant Structural Disorders Seen on MR Defecography, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

