Monday Poster Session
Category: Esophagus
P2914 - Cocaine-Induced Esophagobronchial Fistula, an Underrecognized Phenomena
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Grace E. Kim, DO
Baylor Scott & White Medical Center
Waxahachie, TX
Presenting Author(s)
Grace Kim, DO, Amer Alhreish, DO, Sneha Kalluri, DO, Jack Ni, DO
Baylor Scott & White Medical Center, Fort Worth, TX
Introduction: Esophagobronchial fistula (EBF) is a rare but serious condition involving an abnormal connection between the esophagus and bronchial tree. In adults, it is typically acquired and associated with malignancy, prolonged intubation, trauma, or infections such as tuberculosis. Patients often present with chronic cough after eating or drinking, recurrent aspiration, and lower respiratory tract infections. Cocaine is a well-known vasoconstrictor that can cause ischemic injury to multiple organs. While esophageal necrosis and pneumomediastinum have been reported with cocaine use, its role in EBF formation is not well established. The proposed mechanism involves recurrent vasospasm from prolonged norepinephrine activity, leading to localized ischemia and mucosal breakdown. This case highlights a potential link between chronic cocaine use and EBF development in the absence of other common etiologies, emphasizing the need for early recognition and multidisciplinary care to prevent life-threatening complications.
Case Description/
Methods: A 31-year-old female with asthma and polysubstance use (cocaine, MDMA, alcohol, tobacco) presented with hemoptysis, fever, sore throat, chest and back pain, and worsening cough. One month prior, she had similar symptoms and was treated for presumed pneumonia. On return, she was febrile to 102.9°F with leukocytosis, hyponatremia, and hypokalemia. CT chest showed a 9-cm cavitary pneumonia with mediastinal adenopathy. Bronchoscopy revealed purulent secretions and obstruction of the right lower lobe. Bronchoalveolar lavage and FNA were negative for malignancy or infection; elevated Aspergillus IgE suggested colonization. Thoracentesis confirmed empyema. Initial barium swallow was unrevealing, but follow-up imaging showed aspirated contrast. Esophagogram and EGD confirmed a 4-mm EBF, treated with argon plasma coagulation and esophageal stenting. The patient improved and was discharged on IV antibiotics. The stent was later removed due to discomfort, and she is pending surgical evaluation.
Discussion: This case illustrates EBF in a young adult without common risk factors. Chronic cocaine use likely caused ischemic mucosal injury, supporting the proposed vasospasm mechanism. Her symptoms—hemoptysis, cough with intake, infections—are classic for EBF. Diagnosis was confirmed with imaging and endoscopy, and she responded to endoscopic therapy, though surgical evaluation is ongoing. This case highlights cocaine as a potential but underrecognized cause of EBF in polysubstance users.
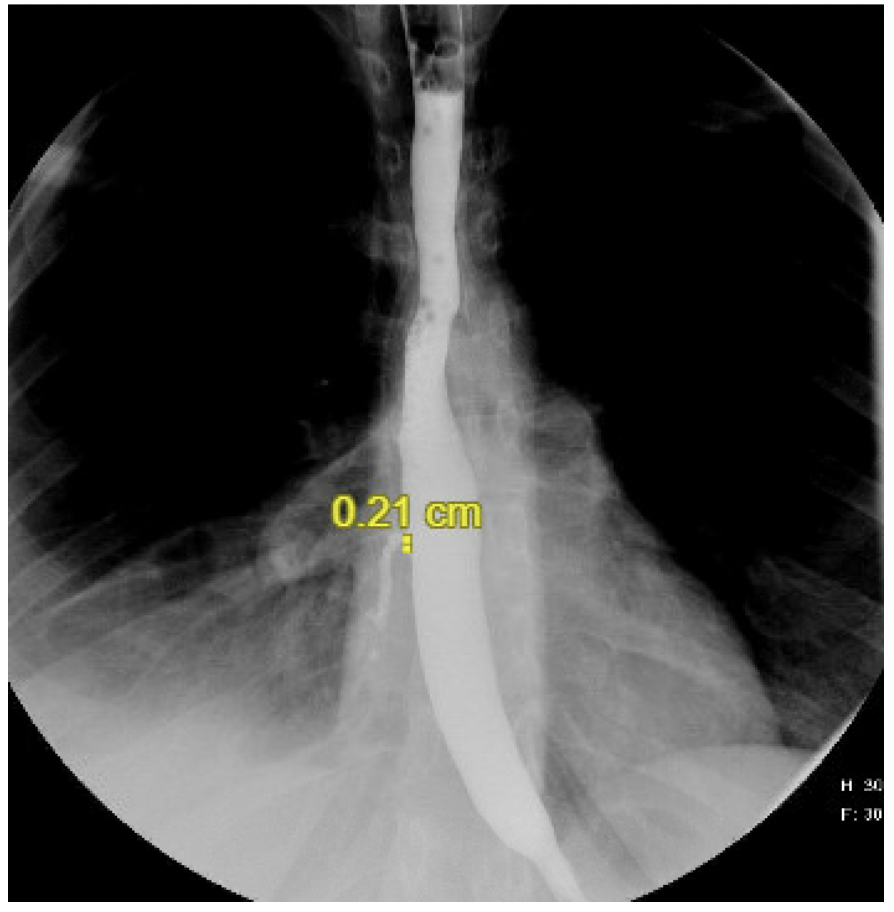
Figure: An esophagogram revealing an extraluminal extension of contrast or fistula from the right posterior lateral mid-to-distal third esophagus to the right lower lung bronchial, measuring 0.2 cm in diameter

Figure: A 4mm esophagobronchial fistula in the upper third of the esophagus was confirmed through an esophagogastroduodenoscopy (EGD)
Disclosures:
Grace Kim indicated no relevant financial relationships.
Amer Alhreish indicated no relevant financial relationships.
Sneha Kalluri indicated no relevant financial relationships.
Jack Ni indicated no relevant financial relationships.
Grace Kim, DO, Amer Alhreish, DO, Sneha Kalluri, DO, Jack Ni, DO. P2914 - Cocaine-Induced Esophagobronchial Fistula, an Underrecognized Phenomena, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Baylor Scott & White Medical Center, Fort Worth, TX
Introduction: Esophagobronchial fistula (EBF) is a rare but serious condition involving an abnormal connection between the esophagus and bronchial tree. In adults, it is typically acquired and associated with malignancy, prolonged intubation, trauma, or infections such as tuberculosis. Patients often present with chronic cough after eating or drinking, recurrent aspiration, and lower respiratory tract infections. Cocaine is a well-known vasoconstrictor that can cause ischemic injury to multiple organs. While esophageal necrosis and pneumomediastinum have been reported with cocaine use, its role in EBF formation is not well established. The proposed mechanism involves recurrent vasospasm from prolonged norepinephrine activity, leading to localized ischemia and mucosal breakdown. This case highlights a potential link between chronic cocaine use and EBF development in the absence of other common etiologies, emphasizing the need for early recognition and multidisciplinary care to prevent life-threatening complications.
Case Description/
Methods: A 31-year-old female with asthma and polysubstance use (cocaine, MDMA, alcohol, tobacco) presented with hemoptysis, fever, sore throat, chest and back pain, and worsening cough. One month prior, she had similar symptoms and was treated for presumed pneumonia. On return, she was febrile to 102.9°F with leukocytosis, hyponatremia, and hypokalemia. CT chest showed a 9-cm cavitary pneumonia with mediastinal adenopathy. Bronchoscopy revealed purulent secretions and obstruction of the right lower lobe. Bronchoalveolar lavage and FNA were negative for malignancy or infection; elevated Aspergillus IgE suggested colonization. Thoracentesis confirmed empyema. Initial barium swallow was unrevealing, but follow-up imaging showed aspirated contrast. Esophagogram and EGD confirmed a 4-mm EBF, treated with argon plasma coagulation and esophageal stenting. The patient improved and was discharged on IV antibiotics. The stent was later removed due to discomfort, and she is pending surgical evaluation.
Discussion: This case illustrates EBF in a young adult without common risk factors. Chronic cocaine use likely caused ischemic mucosal injury, supporting the proposed vasospasm mechanism. Her symptoms—hemoptysis, cough with intake, infections—are classic for EBF. Diagnosis was confirmed with imaging and endoscopy, and she responded to endoscopic therapy, though surgical evaluation is ongoing. This case highlights cocaine as a potential but underrecognized cause of EBF in polysubstance users.
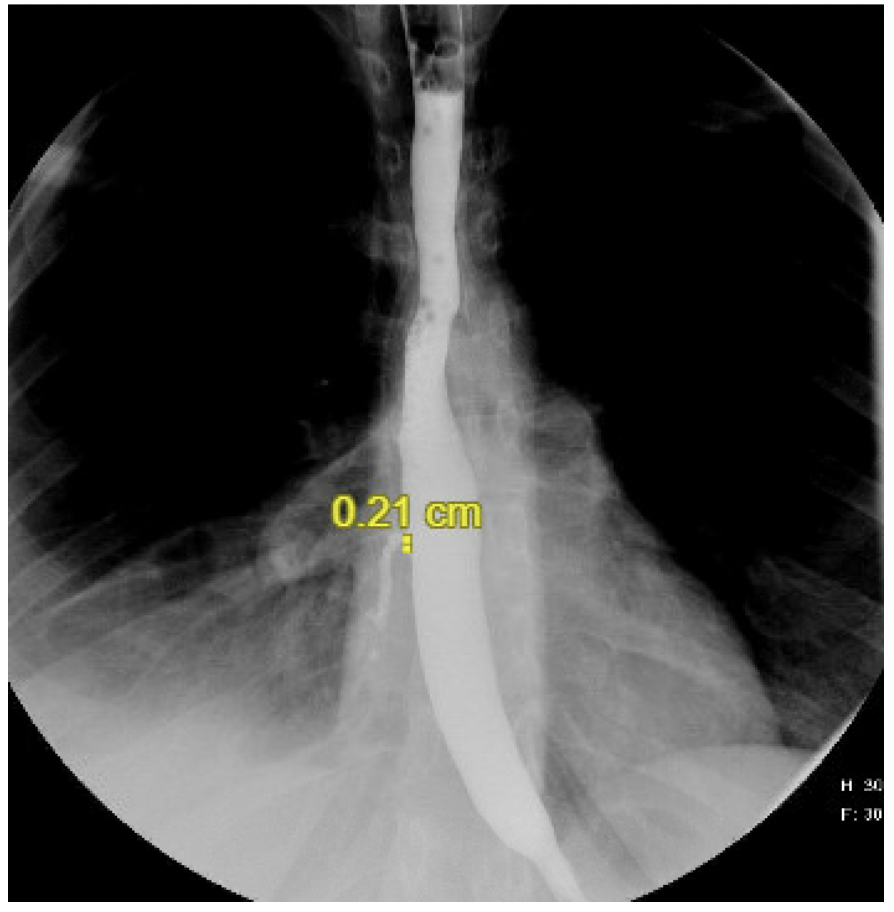
Figure: An esophagogram revealing an extraluminal extension of contrast or fistula from the right posterior lateral mid-to-distal third esophagus to the right lower lung bronchial, measuring 0.2 cm in diameter

Figure: A 4mm esophagobronchial fistula in the upper third of the esophagus was confirmed through an esophagogastroduodenoscopy (EGD)
Disclosures:
Grace Kim indicated no relevant financial relationships.
Amer Alhreish indicated no relevant financial relationships.
Sneha Kalluri indicated no relevant financial relationships.
Jack Ni indicated no relevant financial relationships.
Grace Kim, DO, Amer Alhreish, DO, Sneha Kalluri, DO, Jack Ni, DO. P2914 - Cocaine-Induced Esophagobronchial Fistula, an Underrecognized Phenomena, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
