Monday Poster Session
Category: Esophagus
P2913 - Cardiac Dysphagia: When the Heart Disrupts Swallowing – A Case Series
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sajid Ali, MD (he/him/his)
Aiken Regional Medical Centers
Aiken, SC
Presenting Author(s)
Sajid Ali, MD1, Caitlyn L. Margol, 2, Navkiran Randhawa, DO2, Subbaramiah Sridhar, MD3, Humberto Sifuentes, MD3
1Aiken Regional Medical Centers, Aiken, SC; 2Medical College of Georgia at Augusta University, Augusta, GA; 3Augusta University, Augusta, GA
Introduction: Dysphagia is a common complaint with diverse etiologies, including GERD, eosinophilic esophagitis, motility disorders, and structural abnormalities. Extrinsic esophageal compression remains underappreciated. Cardiac dysphagia occurs when an enlarged cardiovascular structure, typically the left atrium, compresses the esophagus. This may result in progressive dysphagia, hoarseness due to recurrent laryngeal nerve compression (known as Ortner’s syndrome), or even lung collapse.
Case Description/
Methods: Patient 1: A 70-year-old male with atrial fibrillation, heart failure, and metastatic lung adenocarcinoma presented with two months of dysphagia, regurgitation, and 6-pound weight loss. Endoscopy was limited at 30 cm due to bulging likely from a severely dilated left atrium (LAVI 66 mL/m²). A pediatric scope passed easily. No intrinsic structural abnormalities were found.
Patient 2: A 71-year-old female with CHF, coronary artery disease, and severe valvular regurgitation presented with throat secretions, choking, and weight loss. Manometry showed a 4-cm high-pressure zone with pulsatile low-pressure areas at 32 cm, possibly from cardiac indentation. Endoscopy showed a prominent beating heart at 32 cm but no obstruction or mucosal abnormality. Chest imaging consistently showed cardiomegaly and pulmonary vascular congestion.
Patient 3: A 31-year-old male with dilated cardiomyopathy, heart failure, and GERD reported dysphagia to solids, intractable nausea, and weight loss. Barium swallow showed esophageal narrowing due to cardiac silhouette. Echocardiography showed a severely dilated left atrium (LAVI 58.4 mL/m²). His symptoms improved with IV PPI and antiemetics.
Discussion: Cardiac dysphagia, particularly dysphagia megalatriensis, is a rare but significant condition. The left atrium’s posterior location makes it prone to compress the esophagus. Indexed left atrial volumes above 55–60 mL/m², as seen in Patients 1 and 3, can lead to symptomatic compression. Patient 2 demonstrated a more atypical presentation with excessive secretions and high-pressure manometric findings. Diagnosis requires integration of barium swallow, manometry, endoscopy, and cardiac imaging. Management ranges from medical therapy to PEG placement.
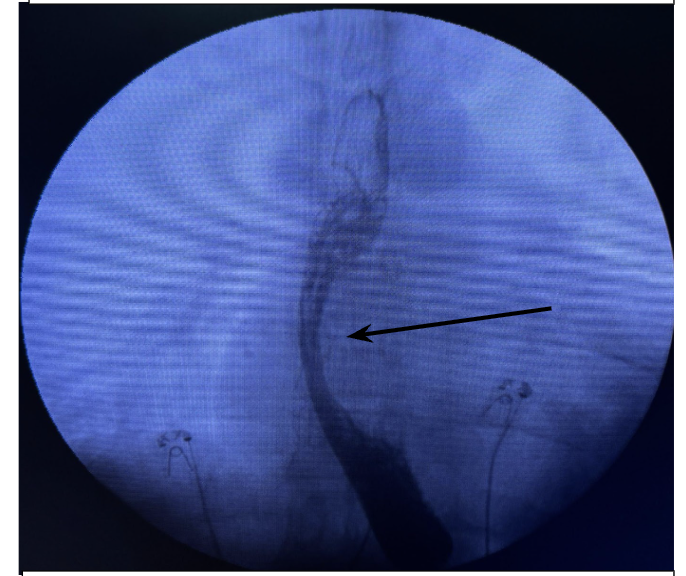
Figure: Figure 1: Endoscopic view of extrinsic compression (arrow) at 30cm (Case 1)
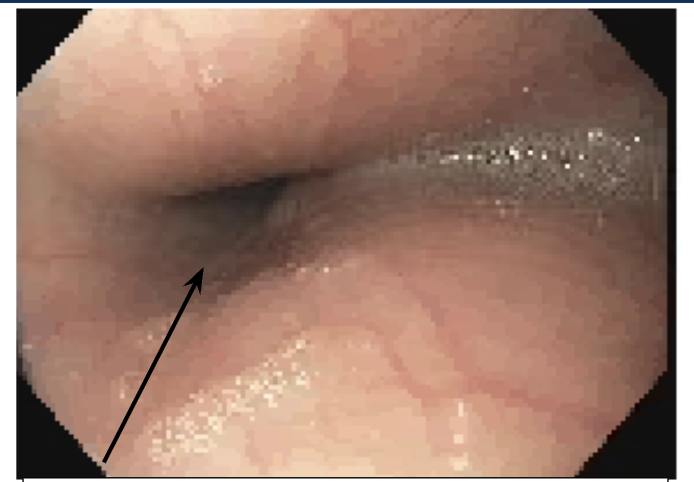
Figure: Figure 2: Barium swallow showing narrowing (arrow) from cardiac silhouette (Case 2)
Disclosures:
Sajid Ali indicated no relevant financial relationships.
Caitlyn Margol indicated no relevant financial relationships.
Navkiran Randhawa indicated no relevant financial relationships.
Subbaramiah Sridhar indicated no relevant financial relationships.
Humberto Sifuentes indicated no relevant financial relationships.
Sajid Ali, MD1, Caitlyn L. Margol, 2, Navkiran Randhawa, DO2, Subbaramiah Sridhar, MD3, Humberto Sifuentes, MD3. P2913 - Cardiac Dysphagia: When the Heart Disrupts Swallowing – A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Aiken Regional Medical Centers, Aiken, SC; 2Medical College of Georgia at Augusta University, Augusta, GA; 3Augusta University, Augusta, GA
Introduction: Dysphagia is a common complaint with diverse etiologies, including GERD, eosinophilic esophagitis, motility disorders, and structural abnormalities. Extrinsic esophageal compression remains underappreciated. Cardiac dysphagia occurs when an enlarged cardiovascular structure, typically the left atrium, compresses the esophagus. This may result in progressive dysphagia, hoarseness due to recurrent laryngeal nerve compression (known as Ortner’s syndrome), or even lung collapse.
Case Description/
Methods: Patient 1: A 70-year-old male with atrial fibrillation, heart failure, and metastatic lung adenocarcinoma presented with two months of dysphagia, regurgitation, and 6-pound weight loss. Endoscopy was limited at 30 cm due to bulging likely from a severely dilated left atrium (LAVI 66 mL/m²). A pediatric scope passed easily. No intrinsic structural abnormalities were found.
Patient 2: A 71-year-old female with CHF, coronary artery disease, and severe valvular regurgitation presented with throat secretions, choking, and weight loss. Manometry showed a 4-cm high-pressure zone with pulsatile low-pressure areas at 32 cm, possibly from cardiac indentation. Endoscopy showed a prominent beating heart at 32 cm but no obstruction or mucosal abnormality. Chest imaging consistently showed cardiomegaly and pulmonary vascular congestion.
Patient 3: A 31-year-old male with dilated cardiomyopathy, heart failure, and GERD reported dysphagia to solids, intractable nausea, and weight loss. Barium swallow showed esophageal narrowing due to cardiac silhouette. Echocardiography showed a severely dilated left atrium (LAVI 58.4 mL/m²). His symptoms improved with IV PPI and antiemetics.
Discussion: Cardiac dysphagia, particularly dysphagia megalatriensis, is a rare but significant condition. The left atrium’s posterior location makes it prone to compress the esophagus. Indexed left atrial volumes above 55–60 mL/m², as seen in Patients 1 and 3, can lead to symptomatic compression. Patient 2 demonstrated a more atypical presentation with excessive secretions and high-pressure manometric findings. Diagnosis requires integration of barium swallow, manometry, endoscopy, and cardiac imaging. Management ranges from medical therapy to PEG placement.
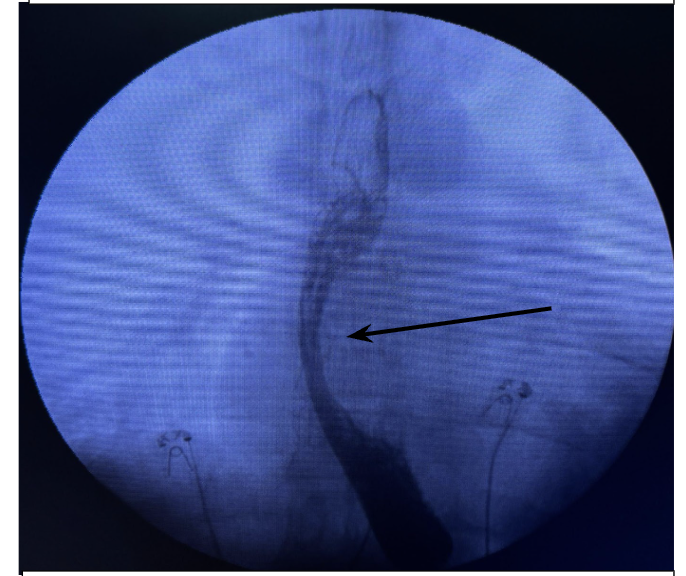
Figure: Figure 1: Endoscopic view of extrinsic compression (arrow) at 30cm (Case 1)
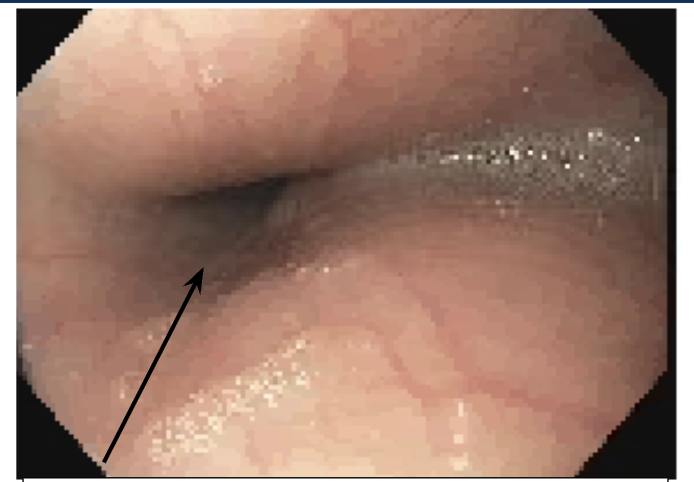
Figure: Figure 2: Barium swallow showing narrowing (arrow) from cardiac silhouette (Case 2)
Disclosures:
Sajid Ali indicated no relevant financial relationships.
Caitlyn Margol indicated no relevant financial relationships.
Navkiran Randhawa indicated no relevant financial relationships.
Subbaramiah Sridhar indicated no relevant financial relationships.
Humberto Sifuentes indicated no relevant financial relationships.
Sajid Ali, MD1, Caitlyn L. Margol, 2, Navkiran Randhawa, DO2, Subbaramiah Sridhar, MD3, Humberto Sifuentes, MD3. P2913 - Cardiac Dysphagia: When the Heart Disrupts Swallowing – A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
