Monday Poster Session
Category: Esophagus
P2881 - Invasive Fistulizing Esophageal Candidiasis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Parekh, DO
University of Florida College of Medicine
Jacksonville, FL
Presenting Author(s)
Sneh Parekh, DO, Laura Suzanne K.. Suarez, MD, Antoine Boustany, MD, Yusuke Hashimoto, MD
University of Florida College of Medicine, Jacksonville, FL
Introduction: Esophageal candidiasis is the infection of the esophagus caused by the fungus Candida, often seen in immunocompromised individuals. While odynophagia is the hallmark of esophageal candidiasis, other common symptoms include dysphagia, diarrhea, nausea, and vomiting. Numerous complications of esophageal candidiasis have been reported, however, serious complications such as fistulation, perforation, and pseudodiverticulosis formation are exceptionally rare. Here, we present the case of candidiasis resulting in esophageal fistula formation along with pseudodiverticulosis in an immunocompetent individual.
Case Description/
Methods: A 52-year-old male with a one-year history of solid food dysphagia, weight loss, and percutaneous endoscopic gastrostomy (PEG) tube placement was referred for further evaluation of undiagnosed esophagitis. Esophagogastroduodenoscopy (EGD) showed diffuse mucosal ulceration in the middle and lower esophagus with three chronic fistulas identified (Figure 1). Subsequent repeat EGD about 1.5 months later revealed the persistent severe esophagitis along with extensive white plaques dispersed throughout (Figure 2). Additionally, progression of diverticula and pseudodiverticula, along with multiple fistulous tracts, were found in the middle and lower esophagus at the site of prior ulceration (Figure 2). The biopsies showed squamous mucosa with severe inflammation, reactive changes, and multiple fungal elements. Fungal cultures were obtained, returning positive for Candida albicans, for which he was prescribed fluconazole with close outpatient follow-up planned.
Discussion: Generally, esophageal candidiasis occurs in the form of superficial candidiasis, and fistula formation along with pseudodiverticula formation within the deeper layers of the esophageal wall are rare complications. Candida infection causes inflammation and fibrosis within the esophageal wall and gland ducts, leading to the formation of fistulas and esophageal intramural pseudodiverticula (EIPD), as seen in our patient. Early recognition with a high index of suspicion, through serial EGDs, along with initiation of infection treatment with antifungals, is crucial for symptomatic control and to prevent further complications that may ultimately lead to death, including esophageal stenosis and perforation.
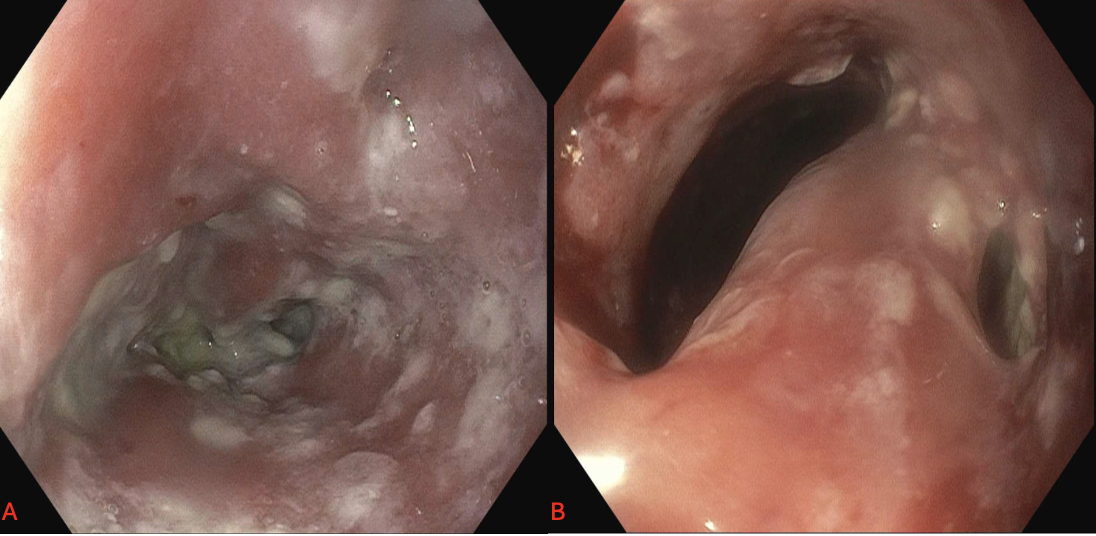
Figure: Figure 1: Image A representing fistula formation with diffuse white plaques and ulceration seen on initial EGD; Image B representing the presence of pseudodiverticulosis seen on initial EGD
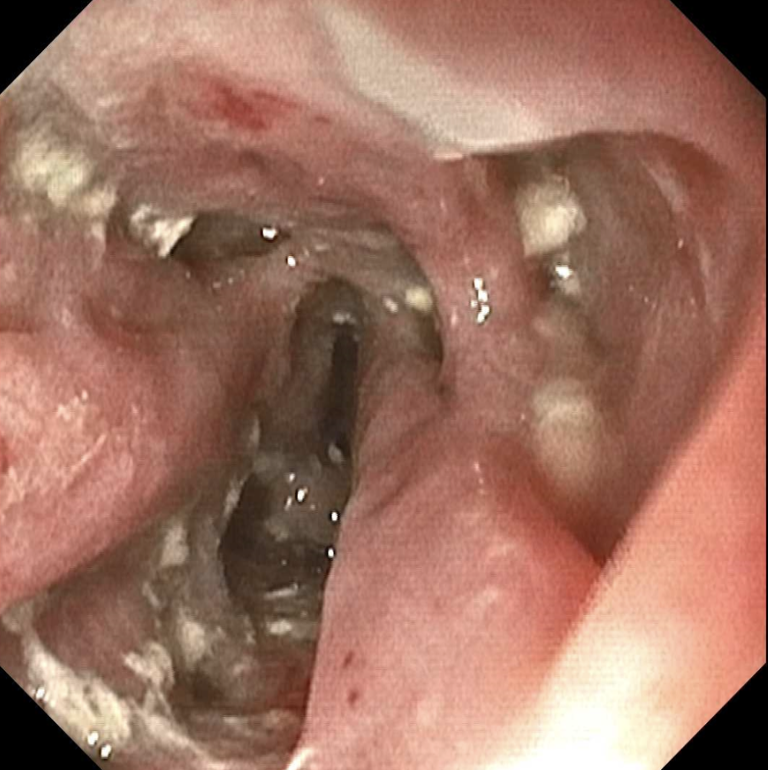
Figure: Figure 2: Repeat EGD on follow up showing worsening erythema, ulceration, plaque growth, and again the presence of pseudodiverticula
Disclosures:
Sneh Parekh indicated no relevant financial relationships.
Laura Suzanne Suarez indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Yusuke Hashimoto indicated no relevant financial relationships.
Sneh Parekh, DO, Laura Suzanne K.. Suarez, MD, Antoine Boustany, MD, Yusuke Hashimoto, MD. P2881 - Invasive Fistulizing Esophageal Candidiasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Florida College of Medicine, Jacksonville, FL
Introduction: Esophageal candidiasis is the infection of the esophagus caused by the fungus Candida, often seen in immunocompromised individuals. While odynophagia is the hallmark of esophageal candidiasis, other common symptoms include dysphagia, diarrhea, nausea, and vomiting. Numerous complications of esophageal candidiasis have been reported, however, serious complications such as fistulation, perforation, and pseudodiverticulosis formation are exceptionally rare. Here, we present the case of candidiasis resulting in esophageal fistula formation along with pseudodiverticulosis in an immunocompetent individual.
Case Description/
Methods: A 52-year-old male with a one-year history of solid food dysphagia, weight loss, and percutaneous endoscopic gastrostomy (PEG) tube placement was referred for further evaluation of undiagnosed esophagitis. Esophagogastroduodenoscopy (EGD) showed diffuse mucosal ulceration in the middle and lower esophagus with three chronic fistulas identified (Figure 1). Subsequent repeat EGD about 1.5 months later revealed the persistent severe esophagitis along with extensive white plaques dispersed throughout (Figure 2). Additionally, progression of diverticula and pseudodiverticula, along with multiple fistulous tracts, were found in the middle and lower esophagus at the site of prior ulceration (Figure 2). The biopsies showed squamous mucosa with severe inflammation, reactive changes, and multiple fungal elements. Fungal cultures were obtained, returning positive for Candida albicans, for which he was prescribed fluconazole with close outpatient follow-up planned.
Discussion: Generally, esophageal candidiasis occurs in the form of superficial candidiasis, and fistula formation along with pseudodiverticula formation within the deeper layers of the esophageal wall are rare complications. Candida infection causes inflammation and fibrosis within the esophageal wall and gland ducts, leading to the formation of fistulas and esophageal intramural pseudodiverticula (EIPD), as seen in our patient. Early recognition with a high index of suspicion, through serial EGDs, along with initiation of infection treatment with antifungals, is crucial for symptomatic control and to prevent further complications that may ultimately lead to death, including esophageal stenosis and perforation.
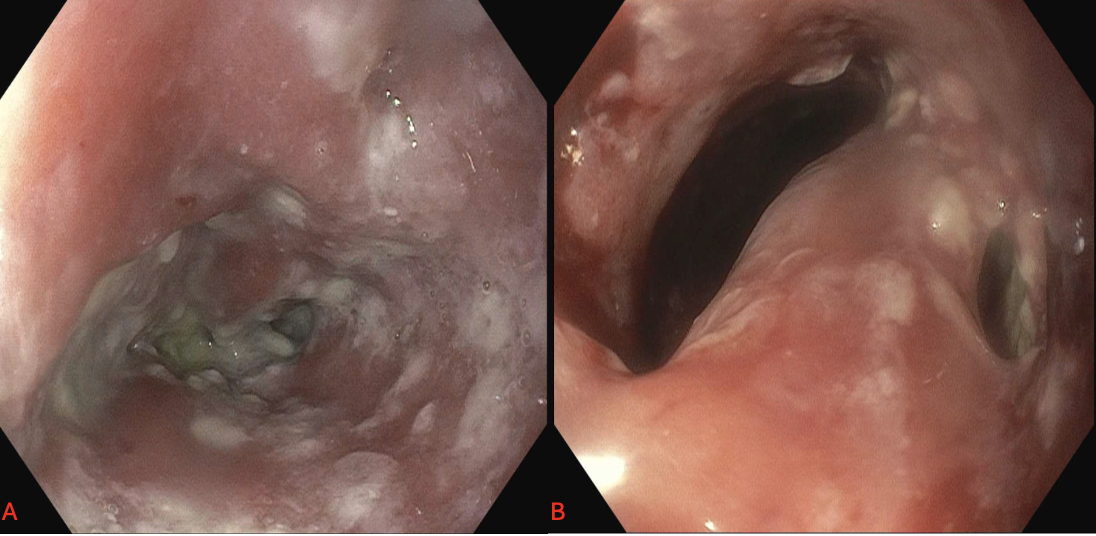
Figure: Figure 1: Image A representing fistula formation with diffuse white plaques and ulceration seen on initial EGD; Image B representing the presence of pseudodiverticulosis seen on initial EGD
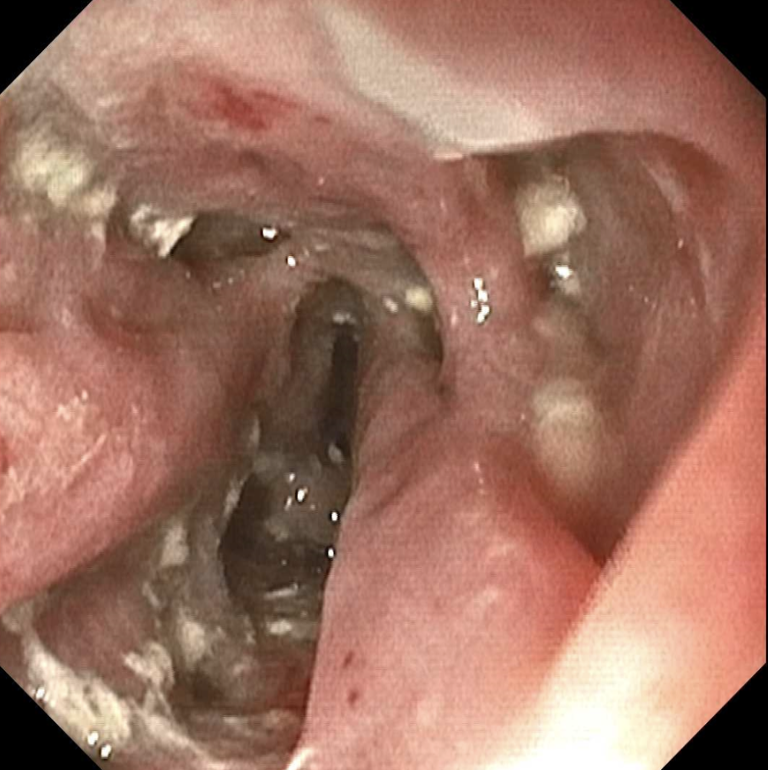
Figure: Figure 2: Repeat EGD on follow up showing worsening erythema, ulceration, plaque growth, and again the presence of pseudodiverticula
Disclosures:
Sneh Parekh indicated no relevant financial relationships.
Laura Suzanne Suarez indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Yusuke Hashimoto indicated no relevant financial relationships.
Sneh Parekh, DO, Laura Suzanne K.. Suarez, MD, Antoine Boustany, MD, Yusuke Hashimoto, MD. P2881 - Invasive Fistulizing Esophageal Candidiasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
