Monday Poster Session
Category: Esophagus
P2875 - Lymphocytic Esophagitis With Concomitant Esophagitis Dissecans Superficialis: A Rare Overlap in an Elderly Woman With Dysphagia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Olivia Foy, MD
Advocate Lutheran General
Park Ridge, IL
Presenting Author(s)
Olivia Foy, MD1, Thomas Mientus, MD2, Meghana Doniparthi, MD1
1Advocate Lutheran General, Park Ridge, IL; 2GI Alliance, Midwest, Waukegan, IL
Introduction: Lymphocytic esophagitis (LyE) is a rare, chronic inflammatory condition characterized histologically by intraepithelial lymphocytosis with minimal granulocytosis. The estimated incidence is 0.1% and is more commonly seen in women in later decades of life. Esophagitis dissecans superficialis (EDS) is an uncommon desquamative disorder defined by mucosal sloughing with minimal inflammation. Both conditions may present with chest discomfort, dysphagia, or dyspepsia. These two conditions are rarely seen concurrently and may present with overlapping clinical and endoscopic features, complicating diagnosis.
Case Description/
Methods: We report the case of an elderly female with a medical history significant for psoriasis on risankizumab, hyperlipidemia on atorvastatin, and GERD who presented with dysphagia refractory to pantoprazole 40 mg twice daily. Esophagogastroduodenoscopy (EGD) at this presentation revealed extensive mucosal sloughing in the distal esophagus with normal appearance of underlying mucosa and erythematous changes of the gastric antrum and prepyloric region (Fig 1). Random biopsies taken from the distal esophagus demonstrated extensive intraepithelial lymphocytes with necrosis and up to 20 eosinophils per high-power field (Fig 2A) admixed with superficial necrotic eosinophilic squamous epithelium between viable reactive squamous epithelium (Fig 2B). She was given a clinical diagnosis of lymphocytic esophagitis with EDS. The patient was initiated on budesonide 1 mg once daily oral solution with pantoprazole.
Discussion: This case illustrates a rare overlap between LyE and EDS. LyE is associated with autoimmune conditions (including IBD), GERD, esophageal motility disorders, tobacco use, and medications such as aspirin and statins. Risk factors for EDS include autoimmune conditions, NSAID/bisphosphonates, and chemical irritants including tobacco. Our patient has several risk factors and falls within the typical demographic range. The endoscopic findings of LyE can mimic eosinophilic esophagitis (EoE) with mucosal edema, linear furrows, and rings. Although at a diagnostic level for EoE, in this case the eosinophils were suspected to be secondary given the dense lymphocytic infiltration. This case underscores the importance of thorough histopathologic evaluation of dysphagia with nonspecific or overlapping endoscopic findings. Recognizing mixed histologic patterns is critical for accurate diagnosis and tailored therapy.
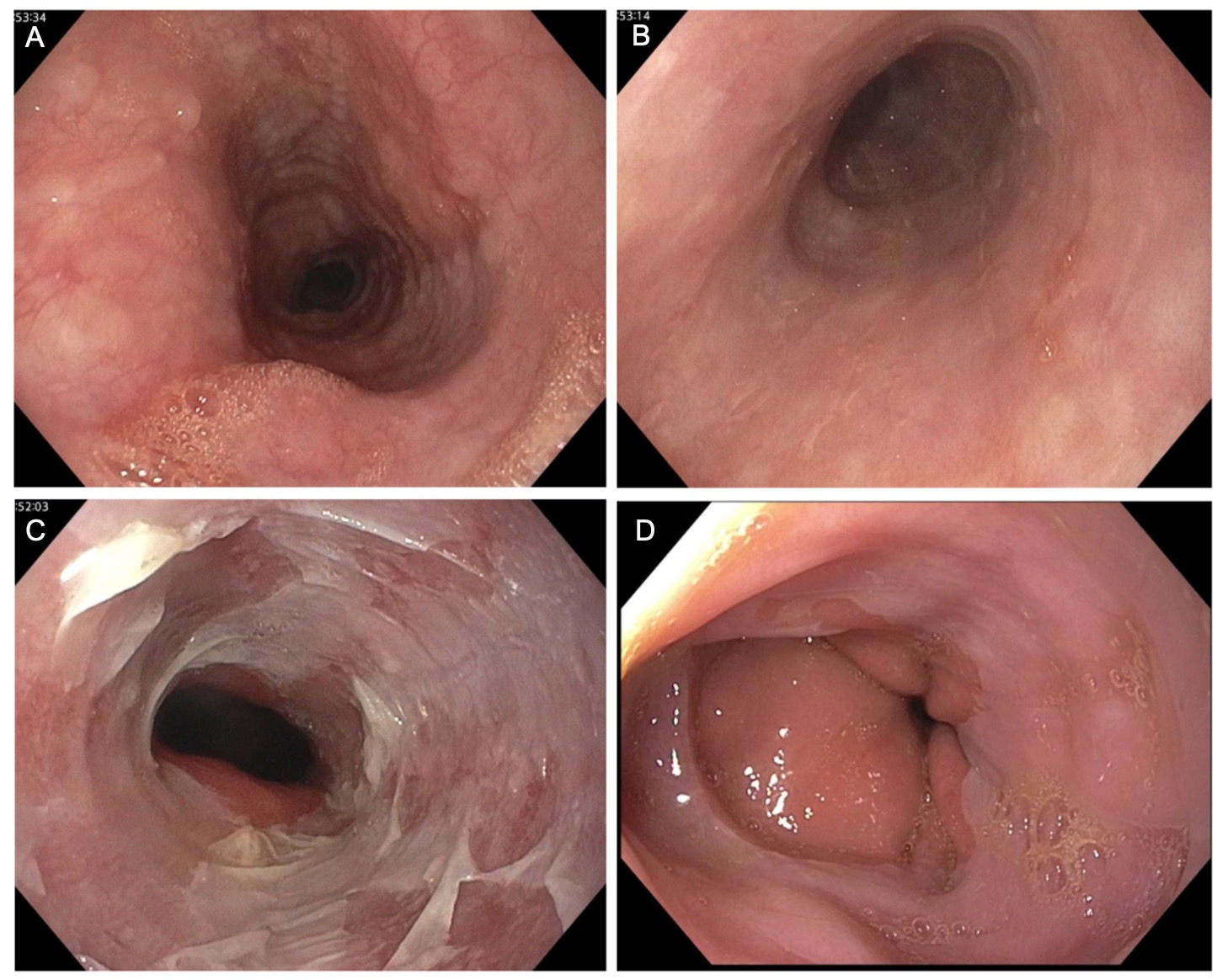
Figure: Figure 1. Endoscopic findings of A. Normal proximal esophagus mucosa B. Normal mid esophagus mucosa C. Mucosal sloughing in the distal esophagus D. Normal distal esophagus from EGD in 2021 for comparison.
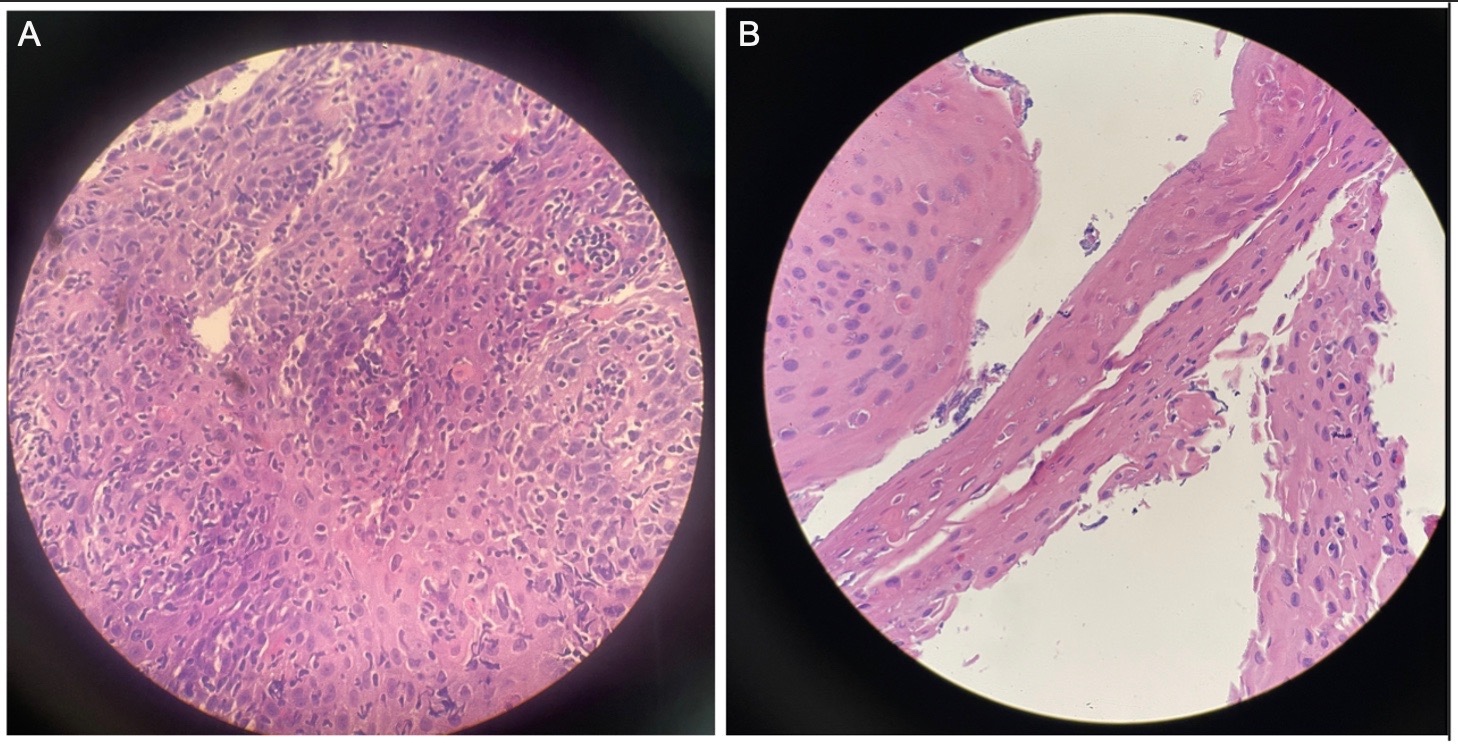
Figure: Figure 2. Histological sections from distal esophageal mucosal biopsy demonstrating A. prominent intraepithelial lymphocytosis, foci of epithelial necrosis, and up to 20 eosinophils per high-power field admixed with B. superficial necrotic eosinophilic squamous epithelial fragments between viable reactive squamous epithelium.
Disclosures:
Olivia Foy indicated no relevant financial relationships.
Thomas Mientus indicated no relevant financial relationships.
Meghana Doniparthi indicated no relevant financial relationships.
Olivia Foy, MD1, Thomas Mientus, MD2, Meghana Doniparthi, MD1. P2875 - Lymphocytic Esophagitis With Concomitant Esophagitis Dissecans Superficialis: A Rare Overlap in an Elderly Woman With Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Advocate Lutheran General, Park Ridge, IL; 2GI Alliance, Midwest, Waukegan, IL
Introduction: Lymphocytic esophagitis (LyE) is a rare, chronic inflammatory condition characterized histologically by intraepithelial lymphocytosis with minimal granulocytosis. The estimated incidence is 0.1% and is more commonly seen in women in later decades of life. Esophagitis dissecans superficialis (EDS) is an uncommon desquamative disorder defined by mucosal sloughing with minimal inflammation. Both conditions may present with chest discomfort, dysphagia, or dyspepsia. These two conditions are rarely seen concurrently and may present with overlapping clinical and endoscopic features, complicating diagnosis.
Case Description/
Methods: We report the case of an elderly female with a medical history significant for psoriasis on risankizumab, hyperlipidemia on atorvastatin, and GERD who presented with dysphagia refractory to pantoprazole 40 mg twice daily. Esophagogastroduodenoscopy (EGD) at this presentation revealed extensive mucosal sloughing in the distal esophagus with normal appearance of underlying mucosa and erythematous changes of the gastric antrum and prepyloric region (Fig 1). Random biopsies taken from the distal esophagus demonstrated extensive intraepithelial lymphocytes with necrosis and up to 20 eosinophils per high-power field (Fig 2A) admixed with superficial necrotic eosinophilic squamous epithelium between viable reactive squamous epithelium (Fig 2B). She was given a clinical diagnosis of lymphocytic esophagitis with EDS. The patient was initiated on budesonide 1 mg once daily oral solution with pantoprazole.
Discussion: This case illustrates a rare overlap between LyE and EDS. LyE is associated with autoimmune conditions (including IBD), GERD, esophageal motility disorders, tobacco use, and medications such as aspirin and statins. Risk factors for EDS include autoimmune conditions, NSAID/bisphosphonates, and chemical irritants including tobacco. Our patient has several risk factors and falls within the typical demographic range. The endoscopic findings of LyE can mimic eosinophilic esophagitis (EoE) with mucosal edema, linear furrows, and rings. Although at a diagnostic level for EoE, in this case the eosinophils were suspected to be secondary given the dense lymphocytic infiltration. This case underscores the importance of thorough histopathologic evaluation of dysphagia with nonspecific or overlapping endoscopic findings. Recognizing mixed histologic patterns is critical for accurate diagnosis and tailored therapy.
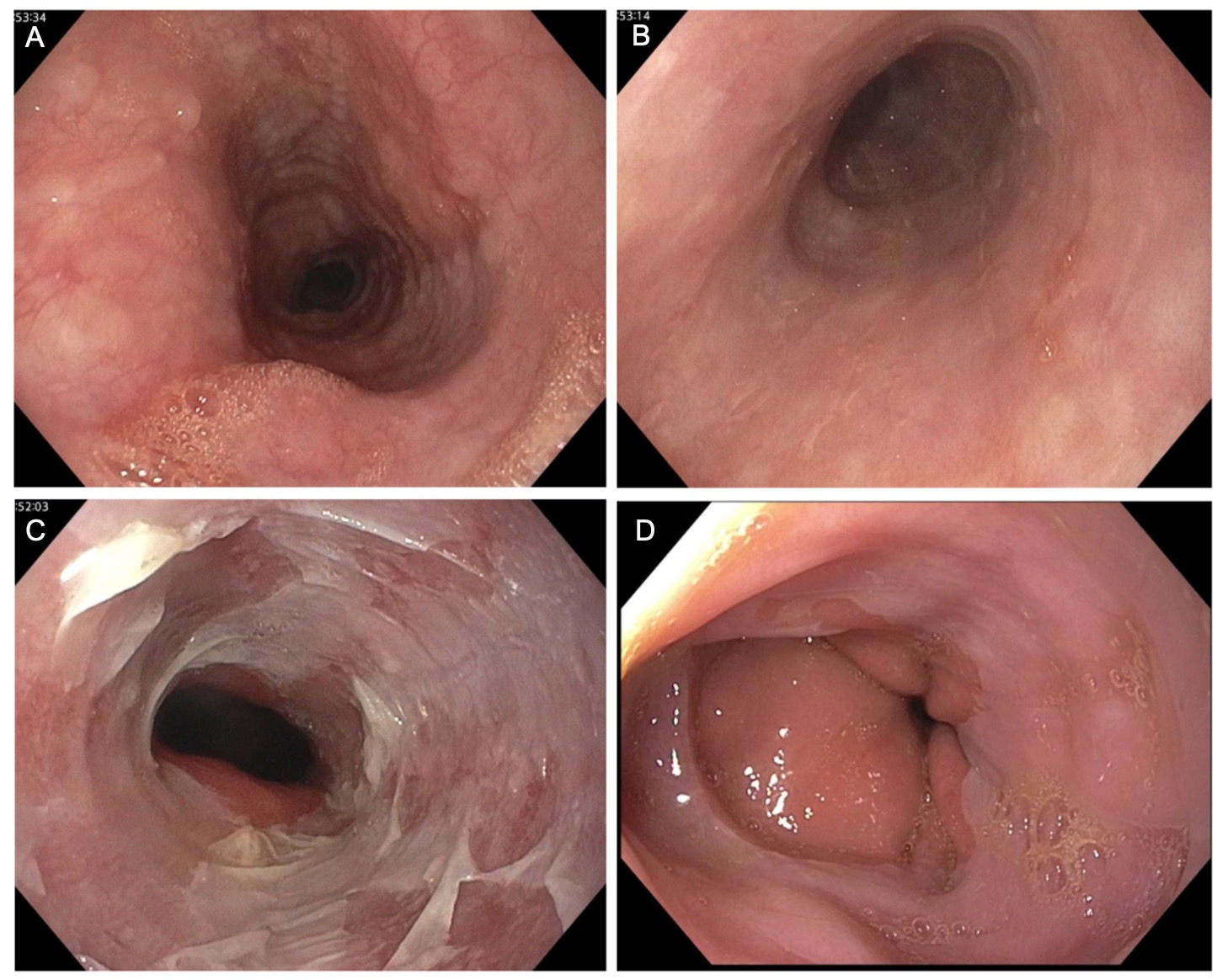
Figure: Figure 1. Endoscopic findings of A. Normal proximal esophagus mucosa B. Normal mid esophagus mucosa C. Mucosal sloughing in the distal esophagus D. Normal distal esophagus from EGD in 2021 for comparison.
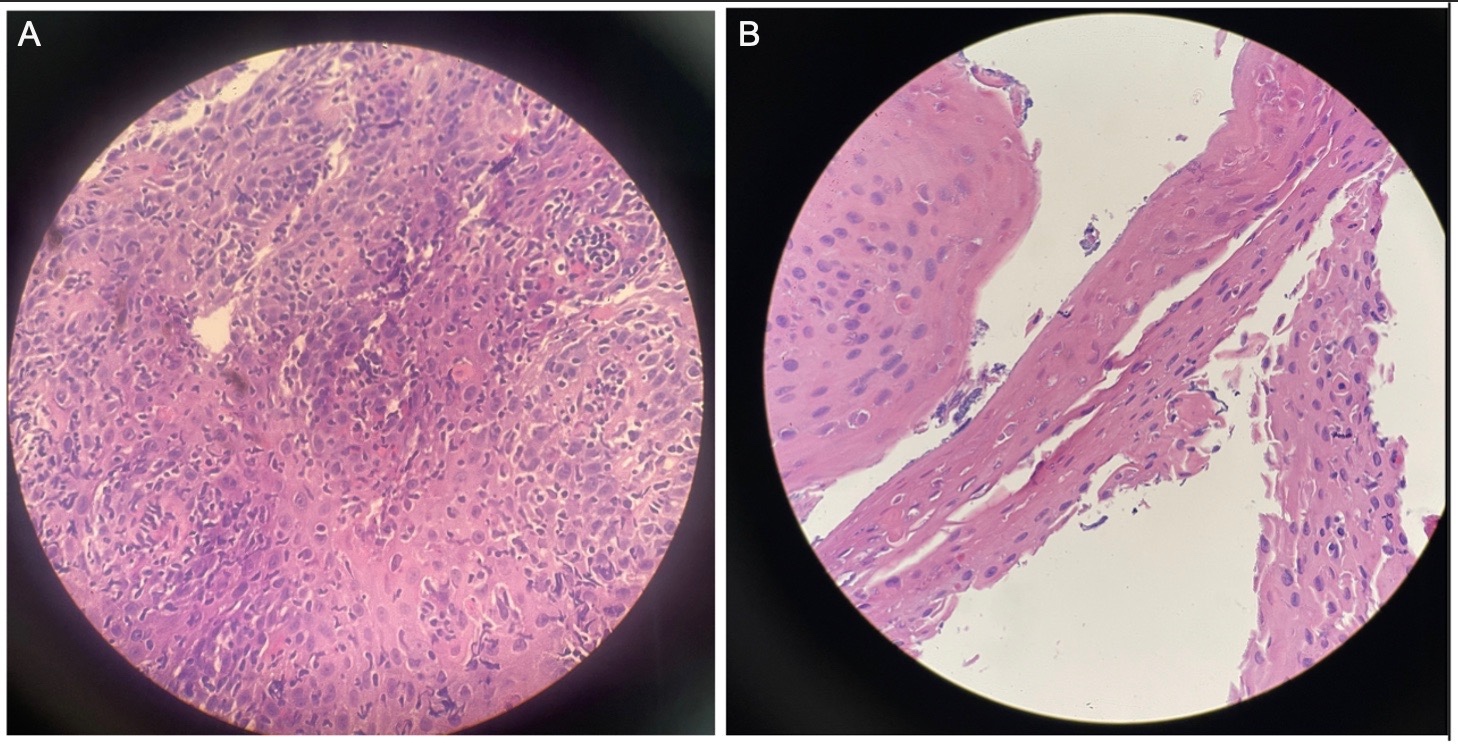
Figure: Figure 2. Histological sections from distal esophageal mucosal biopsy demonstrating A. prominent intraepithelial lymphocytosis, foci of epithelial necrosis, and up to 20 eosinophils per high-power field admixed with B. superficial necrotic eosinophilic squamous epithelial fragments between viable reactive squamous epithelium.
Disclosures:
Olivia Foy indicated no relevant financial relationships.
Thomas Mientus indicated no relevant financial relationships.
Meghana Doniparthi indicated no relevant financial relationships.
Olivia Foy, MD1, Thomas Mientus, MD2, Meghana Doniparthi, MD1. P2875 - Lymphocytic Esophagitis With Concomitant Esophagitis Dissecans Superficialis: A Rare Overlap in an Elderly Woman With Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
