Monday Poster Session
Category: Esophagus
P2873 - Coexisting Eosinophilic Esophagitis and Diffuse Glycogenic Acanthosis in Cowden Syndrome: The Importance of Biopsy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Dimitri Melki, MD (he/him/his)
University of Massachusetts Chan Medical School - Baystate Health
Windsor, CT
Presenting Author(s)
Dimitri Melki, MD1, Kevin Groudan, MD2, David Desilets, MD, PhD3
1University of Massachusetts Chan Medical School - Baystate Health, Windsor, CT; 2University of Massachusetts Chan Medical School - Baystate Health, East Windsor, CT; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA
Introduction: Cowden syndrome (CS), a rare autosomal dominant disorder caused by pathogenic PTEN mutations, is part of the PTEN hamartoma tumor syndrome spectrum. Diffuse esophageal glycogenic acanthosis is a benign condition characterized by white, glycogen-containing plaques of the esophagus. Diffuse esophageal glycogenic acanthosis is seen in over 80% of CS patients, and its association with colon polyposis is pathognomonic for CS. We present a patient whose biopsies for suspected diffuse esophageal glycogenic acanthosis were consistent with eosinophilic esophagitis.
Case Description/
Methods: A 50-year-old woman with history of Cowden syndrome (confirmed by PTEN gene mutation), breast cancer, thyroidectomy for thyroid nodules, and hysterectomy with bilateral salpingo-oophorectomy, presented for her routine, biennial esophagogastroduodenoscopy (EGD) and colonoscopy to screen for stomach, small bowel and colon cancer. Of note, patient did not endorse a history of dysphagia. Prior endoscopies were significant for diffuse esophageal glycogenic acanthosis, hyperplastic gastric polyps, and numerous hamartomatous colon polyps. Repeat EGD was significant for diffuse congestion and cobblestoning of the mucosa throughout the whole esophagus, suspicious for diffuse esophageal glycogenic acanthosis. Four-quadrant cold forceps biopsies were obtained throughout the whole esophagus. Histology demonstrated intraepithelial eosinophilia, with a maximum of 45 eosinophils/HPF, consistent with a diagnosis of eosinophilic esophagitis.
Discussion: Eosinophilic esophagitis (EoE), is an immune mediated disorder often triggered by allergens. It is often associated with dysphagia and food impaction, and diagnosis requires histologic confirmation of ≥15 eosinophils per high-power field. Classic endoscopic features include rings, furrows, and edema.
Our case highlights the importance of biopsies in Cowden syndrome patients in which diffuse esophageal glycogenic acanthosis is observed. While glycogenic acanthosis is common in Cowden syndrome, it could be masking other pathologies. EoE is a treatable condition that cause significant morbidities if it is left undiagnosed. Routine biopsy should be considered to rule out EoE in Cowden patients who present with esophageal mucosal changes, given the overlapping appearance on endoscopy and clinical implications of missing the diagnosis.
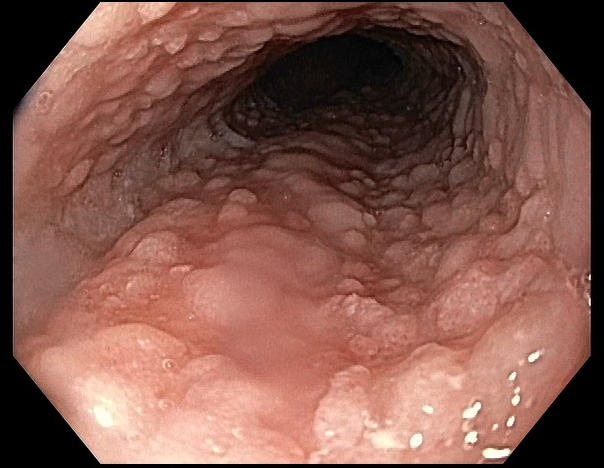
Figure: Cobblestoning of the esophageal mucosa seen on endoscopy
Disclosures:
Dimitri Melki indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
David Desilets indicated no relevant financial relationships.
Dimitri Melki, MD1, Kevin Groudan, MD2, David Desilets, MD, PhD3. P2873 - Coexisting Eosinophilic Esophagitis and Diffuse Glycogenic Acanthosis in Cowden Syndrome: The Importance of Biopsy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School - Baystate Health, Windsor, CT; 2University of Massachusetts Chan Medical School - Baystate Health, East Windsor, CT; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA
Introduction: Cowden syndrome (CS), a rare autosomal dominant disorder caused by pathogenic PTEN mutations, is part of the PTEN hamartoma tumor syndrome spectrum. Diffuse esophageal glycogenic acanthosis is a benign condition characterized by white, glycogen-containing plaques of the esophagus. Diffuse esophageal glycogenic acanthosis is seen in over 80% of CS patients, and its association with colon polyposis is pathognomonic for CS. We present a patient whose biopsies for suspected diffuse esophageal glycogenic acanthosis were consistent with eosinophilic esophagitis.
Case Description/
Methods: A 50-year-old woman with history of Cowden syndrome (confirmed by PTEN gene mutation), breast cancer, thyroidectomy for thyroid nodules, and hysterectomy with bilateral salpingo-oophorectomy, presented for her routine, biennial esophagogastroduodenoscopy (EGD) and colonoscopy to screen for stomach, small bowel and colon cancer. Of note, patient did not endorse a history of dysphagia. Prior endoscopies were significant for diffuse esophageal glycogenic acanthosis, hyperplastic gastric polyps, and numerous hamartomatous colon polyps. Repeat EGD was significant for diffuse congestion and cobblestoning of the mucosa throughout the whole esophagus, suspicious for diffuse esophageal glycogenic acanthosis. Four-quadrant cold forceps biopsies were obtained throughout the whole esophagus. Histology demonstrated intraepithelial eosinophilia, with a maximum of 45 eosinophils/HPF, consistent with a diagnosis of eosinophilic esophagitis.
Discussion: Eosinophilic esophagitis (EoE), is an immune mediated disorder often triggered by allergens. It is often associated with dysphagia and food impaction, and diagnosis requires histologic confirmation of ≥15 eosinophils per high-power field. Classic endoscopic features include rings, furrows, and edema.
Our case highlights the importance of biopsies in Cowden syndrome patients in which diffuse esophageal glycogenic acanthosis is observed. While glycogenic acanthosis is common in Cowden syndrome, it could be masking other pathologies. EoE is a treatable condition that cause significant morbidities if it is left undiagnosed. Routine biopsy should be considered to rule out EoE in Cowden patients who present with esophageal mucosal changes, given the overlapping appearance on endoscopy and clinical implications of missing the diagnosis.
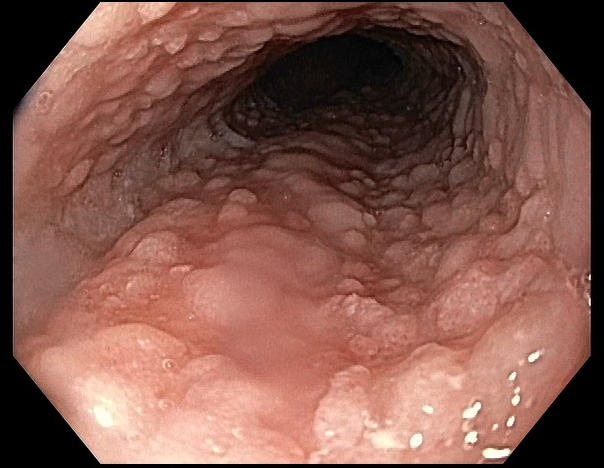
Figure: Cobblestoning of the esophageal mucosa seen on endoscopy
Disclosures:
Dimitri Melki indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
David Desilets indicated no relevant financial relationships.
Dimitri Melki, MD1, Kevin Groudan, MD2, David Desilets, MD, PhD3. P2873 - Coexisting Eosinophilic Esophagitis and Diffuse Glycogenic Acanthosis in Cowden Syndrome: The Importance of Biopsy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
