Monday Poster Session
Category: Esophagus
P2869 - Multisystem Sarcoidosis Presenting as Oropharyngeal Dysphagia: A Diagnostic Challenge
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cinthia Reyes Cruz, MD
University of Miami Miller School of Medicine at Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Cinthia Reyes Cruz, MD1, Mathew Farbman, DO2, Natasha Mederos Rocha, MD3, Luis Penaranda-Bolano, MD1, Nemer Dabage-Forzoli, MD1
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2Holy Cross Medical Group, Fort Lauderdale, FL; 3University of Miami, Fort Lauderdale, FL
Introduction: Sarcoidosis is a multisystem granulomatous disease with a higher prevalence among females and African Americans. It involves the lungs and mediastinal lymph nodes in over 90% of cases. Extrapulmonary manifestations can involve the skin, eyes, liver, and heart. However, gastrointestinal (GI) involvement is rare (< 1%). Even more uncommon is laryngeal sarcoidosis, seen in only 0.5–5% of cases, often presenting with hoarseness and/or dysphagia due to mass effect or vocal cord dysfunction.
Case Description/
Methods: A 68-year-old African American female with a history of hypertension presented with progressive dysphagia, dry cough, and unintentional weight loss of fourteen pounds over the past three months. Initial evaluation included a modified barium swallow, which showed oropharyngeal dysphagia. Computed Tomography (CT) of the neck revealed soft tissue prominence in the oropharynx. Further workup included an upper endoscopy, that was unrevealing, and a laryngoscopy, which revealed left oropharyngeal fullness and right vocal cord paralysis, suggestive of neuromuscular dysfunction.
Due to significant weight loss and dysphagia, which was initially concerning for malignancy, a CT abdomen and pelvis was ordered. It showed multiple enhancing splenic lesions, the largest measuring 5.7 cm (Figure1). Positron Emission Tomography PET/CT showed intense fluorodeoxyglucose (FDG) uptake in the spleen, gastric wall, mediastinal and hilar lymph nodes, and multiple bones, raising concern for disseminated malignancy (Figure 2). Laboratory studies revealed mildly elevated ACE 56 U/L and CRP 13 mg/L, elevated lysozyme at 20.9 mcg/mL and elevated 1,25 dihydroxy Vitamin D. She had a negative flow cytometry, ANA, Quantiferon Gold, and negative CEA, CA 125, CA 19-9, CA 27-29, CA 15-3. Iliac bone biopsy revealed non-caseating granulomas. Endobronchial ultrasound-guided biopsies of the mediastinal lymph nodes revealed granulomatous inflammation without malignant cells, confirming a diagnosis of sarcoidosis.
Discussion: Laryngeal sarcoidosis presenting as oropharyngeal dysphagia due to laryngeal nerve compression is an extremely rare and often missed diagnosis, with only a few cases reported in the literature. This case highlights the need for a high index of suspicion for sarcoidosis in atypical presentations, especially when imaging points toward malignancy and no overt lung involvement.
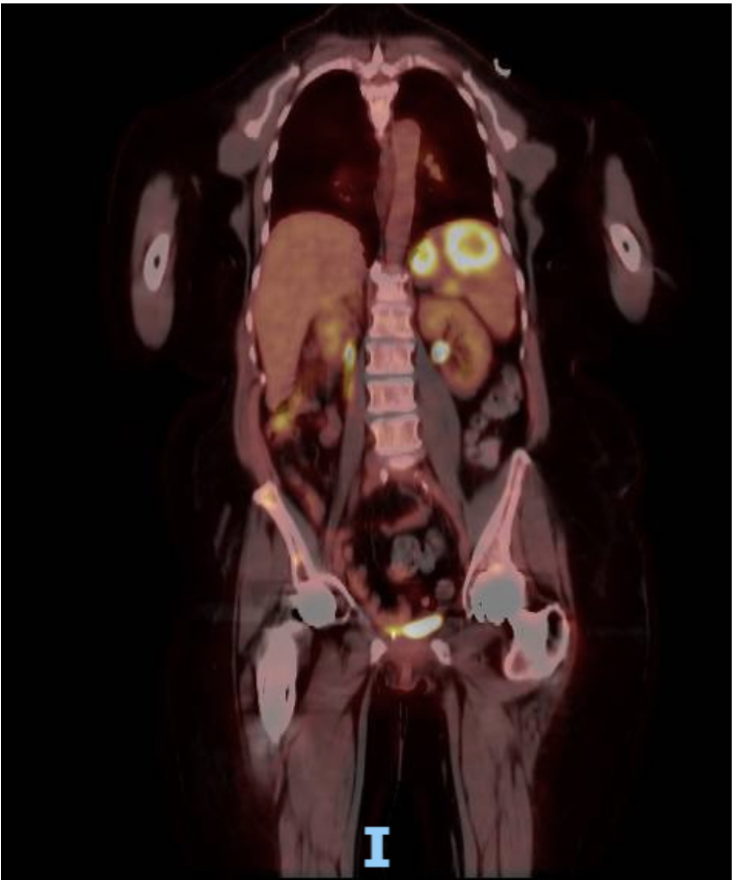
Figure: Figure 1. CT Abdomen and Pelvis showing multiple heterogeneous hypodense lesions/masses in the liver and spleen
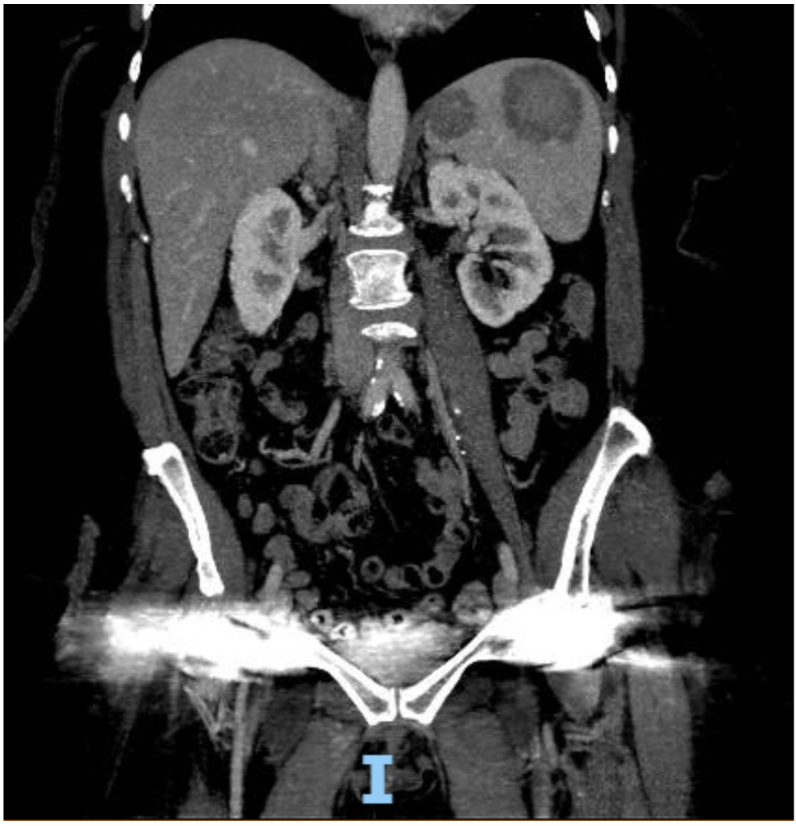
Figure: Figure 2. PET CT Scan showing multiple reuptake sites
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Mathew Farbman indicated no relevant financial relationships.
Natasha Mederos Rocha indicated no relevant financial relationships.
Luis Penaranda-Bolano indicated no relevant financial relationships.
Nemer Dabage-Forzoli indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD1, Mathew Farbman, DO2, Natasha Mederos Rocha, MD3, Luis Penaranda-Bolano, MD1, Nemer Dabage-Forzoli, MD1. P2869 - Multisystem Sarcoidosis Presenting as Oropharyngeal Dysphagia: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL; 2Holy Cross Medical Group, Fort Lauderdale, FL; 3University of Miami, Fort Lauderdale, FL
Introduction: Sarcoidosis is a multisystem granulomatous disease with a higher prevalence among females and African Americans. It involves the lungs and mediastinal lymph nodes in over 90% of cases. Extrapulmonary manifestations can involve the skin, eyes, liver, and heart. However, gastrointestinal (GI) involvement is rare (< 1%). Even more uncommon is laryngeal sarcoidosis, seen in only 0.5–5% of cases, often presenting with hoarseness and/or dysphagia due to mass effect or vocal cord dysfunction.
Case Description/
Methods: A 68-year-old African American female with a history of hypertension presented with progressive dysphagia, dry cough, and unintentional weight loss of fourteen pounds over the past three months. Initial evaluation included a modified barium swallow, which showed oropharyngeal dysphagia. Computed Tomography (CT) of the neck revealed soft tissue prominence in the oropharynx. Further workup included an upper endoscopy, that was unrevealing, and a laryngoscopy, which revealed left oropharyngeal fullness and right vocal cord paralysis, suggestive of neuromuscular dysfunction.
Due to significant weight loss and dysphagia, which was initially concerning for malignancy, a CT abdomen and pelvis was ordered. It showed multiple enhancing splenic lesions, the largest measuring 5.7 cm (Figure1). Positron Emission Tomography PET/CT showed intense fluorodeoxyglucose (FDG) uptake in the spleen, gastric wall, mediastinal and hilar lymph nodes, and multiple bones, raising concern for disseminated malignancy (Figure 2). Laboratory studies revealed mildly elevated ACE 56 U/L and CRP 13 mg/L, elevated lysozyme at 20.9 mcg/mL and elevated 1,25 dihydroxy Vitamin D. She had a negative flow cytometry, ANA, Quantiferon Gold, and negative CEA, CA 125, CA 19-9, CA 27-29, CA 15-3. Iliac bone biopsy revealed non-caseating granulomas. Endobronchial ultrasound-guided biopsies of the mediastinal lymph nodes revealed granulomatous inflammation without malignant cells, confirming a diagnosis of sarcoidosis.
Discussion: Laryngeal sarcoidosis presenting as oropharyngeal dysphagia due to laryngeal nerve compression is an extremely rare and often missed diagnosis, with only a few cases reported in the literature. This case highlights the need for a high index of suspicion for sarcoidosis in atypical presentations, especially when imaging points toward malignancy and no overt lung involvement.
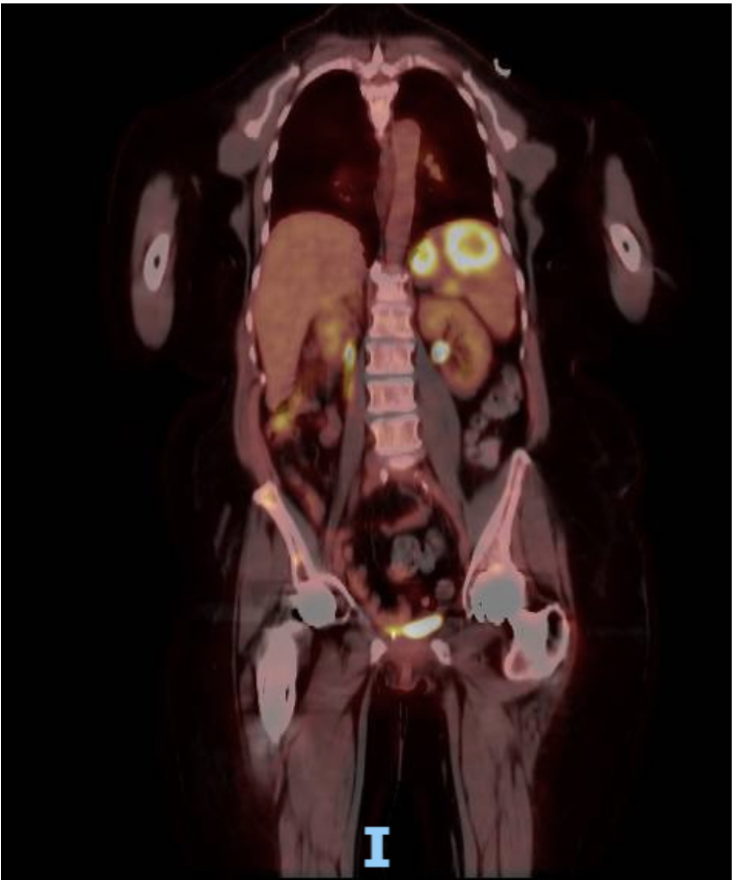
Figure: Figure 1. CT Abdomen and Pelvis showing multiple heterogeneous hypodense lesions/masses in the liver and spleen
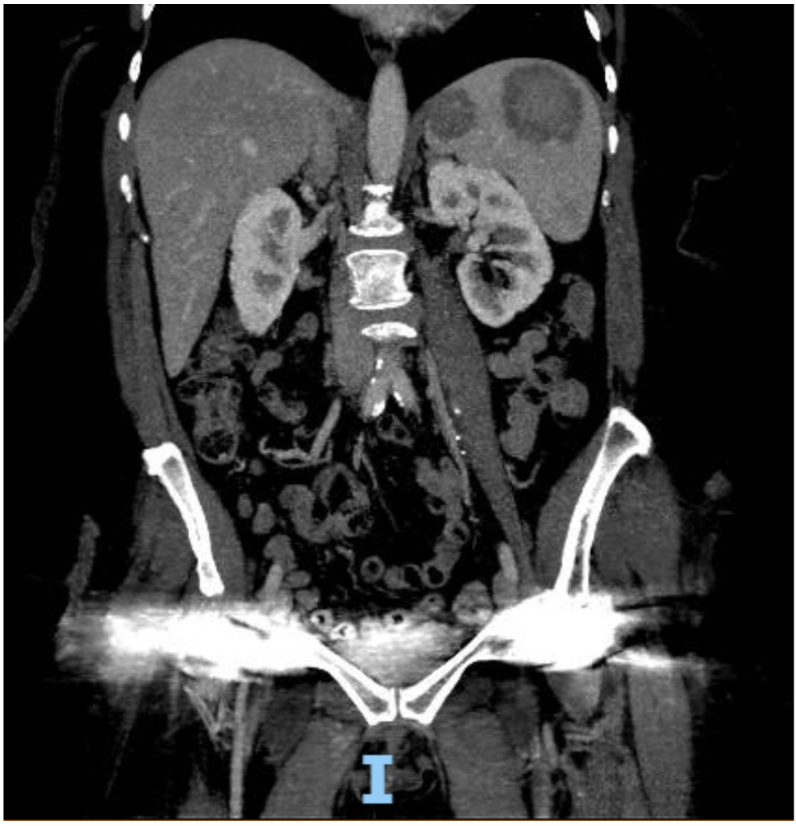
Figure: Figure 2. PET CT Scan showing multiple reuptake sites
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Mathew Farbman indicated no relevant financial relationships.
Natasha Mederos Rocha indicated no relevant financial relationships.
Luis Penaranda-Bolano indicated no relevant financial relationships.
Nemer Dabage-Forzoli indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD1, Mathew Farbman, DO2, Natasha Mederos Rocha, MD3, Luis Penaranda-Bolano, MD1, Nemer Dabage-Forzoli, MD1. P2869 - Multisystem Sarcoidosis Presenting as Oropharyngeal Dysphagia: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
