Monday Poster Session
Category: Esophagus
P2868 - A Cryptic Esophageal Lesion: Benign or Malignant?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Carlos G. Diola, MD (he/him/his)
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Carlos G. Diola, MD1, Mantej Sehmbhi, MBBS2, Edward Lung, MD3, Ian Cohen, MD3, Alexandra Rozalen, MD3, Abdelsalam Sharabi, MD3
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY
Introduction: Granular cell tumors, previously known as Abrikossoff’s tumor or granular cell myoblasts, are rare tumors that can involve the gastrointestinal tract. Initially described in 1926 by Russian pathologist Abrikossoff, the tumor can affect anatomical regions around the head, neck, and oral cavity but rarely arises in the esophagus. These tumors are generally benign, neurogenic in origin, and esophageal involvement only has an incidence of approximately 33 per 100,000. The mean age of diagnosis is 45 years, with lesions more commonly found in men, but should be considered in women presenting with an intramural mass at the proximal or distal third of the esophagus. Dysphagia is a common symptom seen in 33% of patients with these tumors, while the rest are asymptomatic. Esophageal granular cell tumors do have malignant potential and must be monitored closely.
Case Description/
Methods: In this case, a 57-year-old Caucasian female with a past medical history of gastroesophageal reflux disease (GERD) presented to the gastroenterology clinic for evaluation of intermittent worsening dysphagia with acid reflux. Subsequently, an upper endoscopy showed a nodule in the lower third of the esophagus, and diffuse mild inflammation with erythema in the gastric body and antrum. The esophageal biopsies were positive for S-100 on immunohistochemistry, a protein marker of neural crest origin and gastric biopsies were positive for Helicobacter pylori (H. pylori). An upper endoscopic ultrasound (EUS) demonstrated an eight mm in thickness hypoechoic and submucosal lesion with well-defined borders in the lower third of the esophagus. Endoscopic mucosal resection (EMR) was then performed with complete removal. Pathology from the resected lesion demonstrated an underlying population of neoplastic cells, with strong S100 and CD68 positivity confirming the diagnosis of a granular cell tumor. The patient was also treated with bismuth-based quadruple therapy for coincidental H. pylori infection and omeprazole.
Discussion: As previously discussed, there is a potential for granular cell tumors to become malignant. Monitoring with EUS is critical in determining the choice of treatment. Small (< 1cm) lesions are managed conservatively, and larger lesions ( >1cm) are resected endoscopically. In this case, the patient still underwent EMR since the lesion was causing dysphagia. Diagnosis, work-up, and long-term management have not been well described due to the tumor’s rarity.
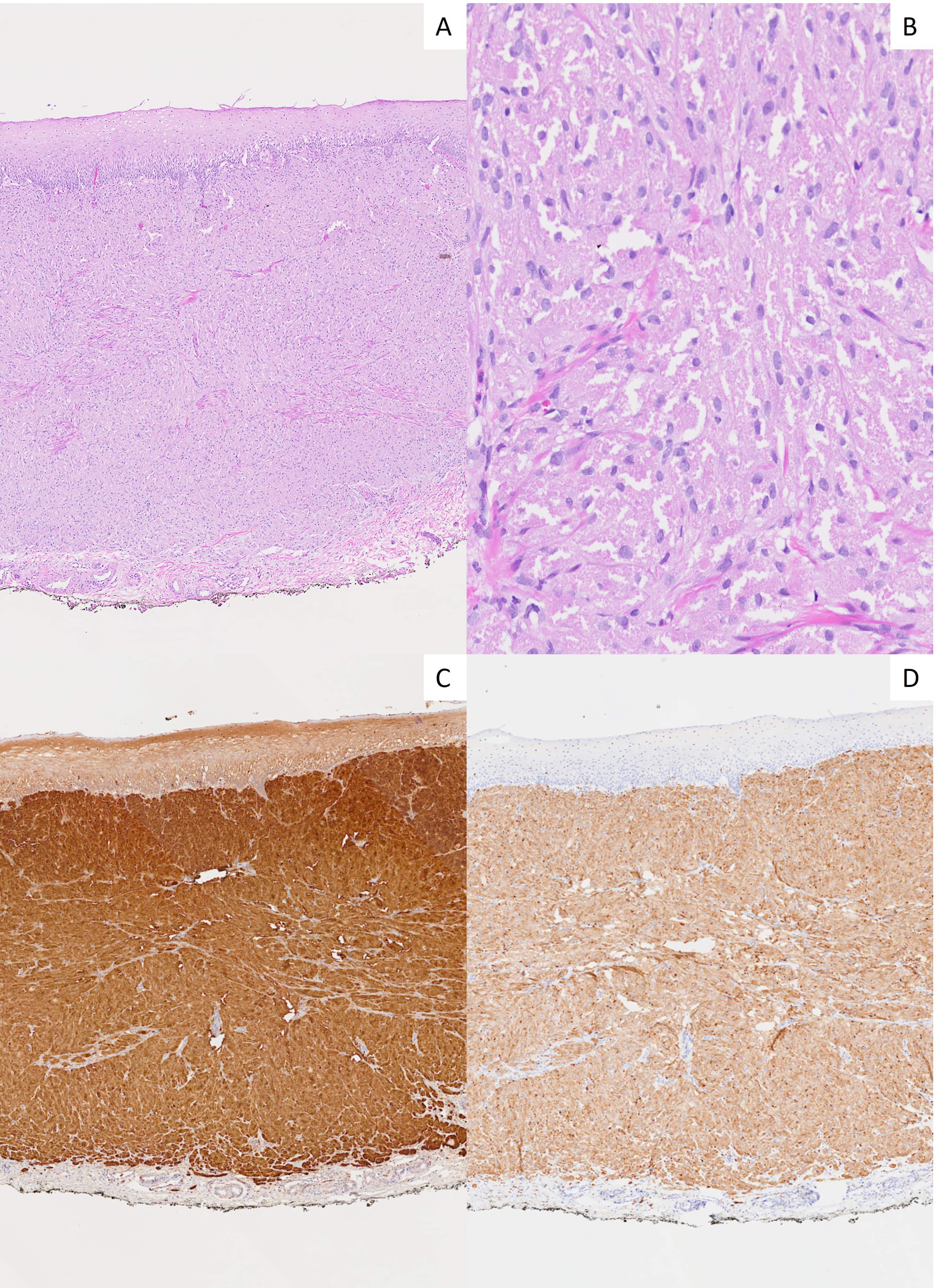
Figure: Image 1: Endoscopic views of a single eight mm (subepithelial) nodule in the lower third of the esophagus.
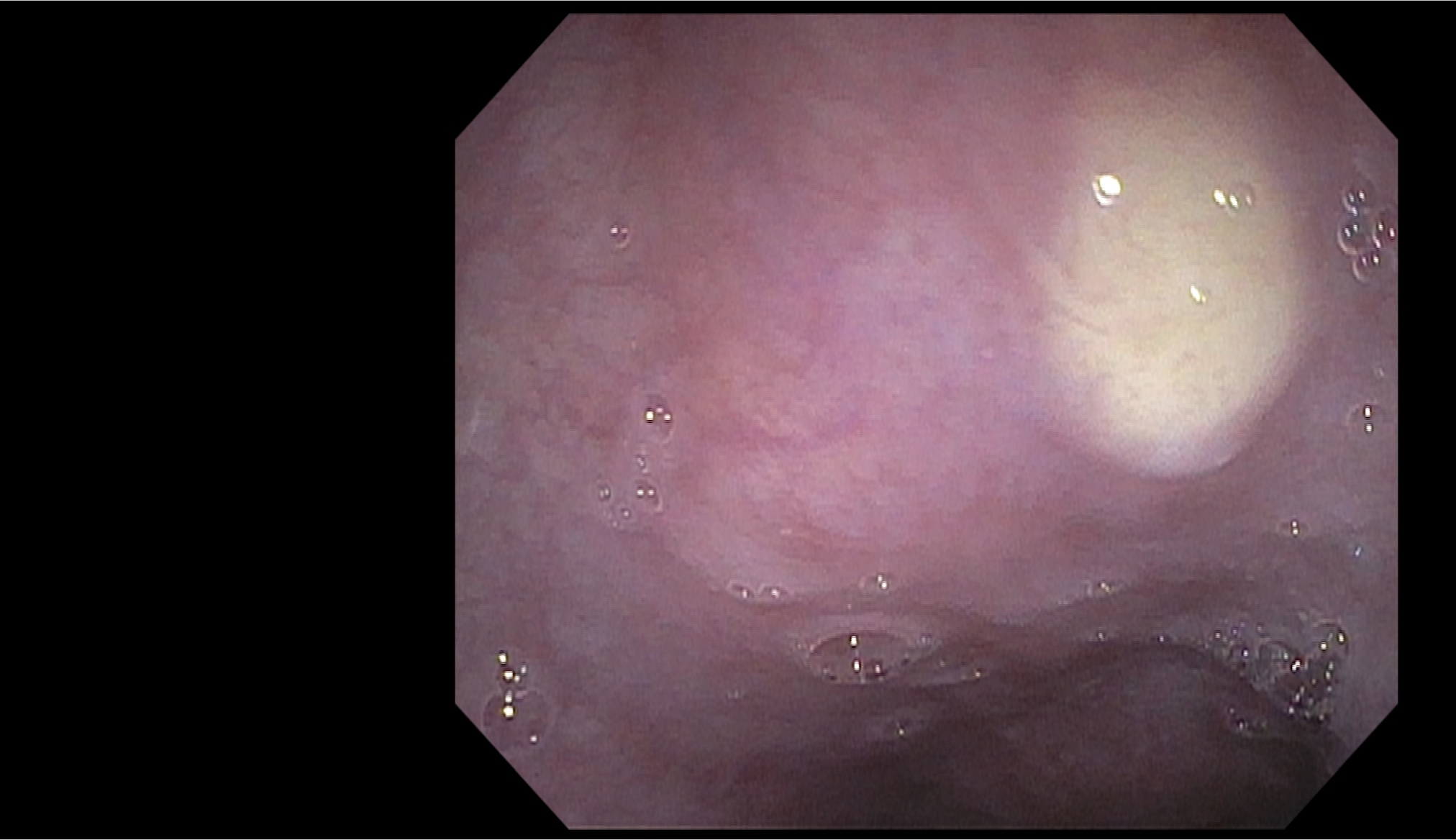
Figure: Image 2: Histopathologic digital images of an esophageal nodule: (A) H&E stain at 2x magnification reveals esophageal mucosa with an underlying population of neoplastic cells. (B) H&E stain at 20x magnification displays characteristic sheets or packets of uniform epithelioid cells with abundant eosinophilic granular cytoplasm and small nuclei. Immunohistochemical staining of the neoplastic cells demonstrates diffuse, strong S100 positivity (C) and CD68 positivity (D), both shown at 2x.
Disclosures:
Carlos Diola indicated no relevant financial relationships.
Mantej Sehmbhi indicated no relevant financial relationships.
Edward Lung indicated no relevant financial relationships.
Ian Cohen indicated no relevant financial relationships.
Alexandra Rozalen indicated no relevant financial relationships.
Abdelsalam Sharabi indicated no relevant financial relationships.
Carlos G. Diola, MD1, Mantej Sehmbhi, MBBS2, Edward Lung, MD3, Ian Cohen, MD3, Alexandra Rozalen, MD3, Abdelsalam Sharabi, MD3. P2868 - A Cryptic Esophageal Lesion: Benign or Malignant?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai, New York, NY; 3Mount Sinai West, New York, NY
Introduction: Granular cell tumors, previously known as Abrikossoff’s tumor or granular cell myoblasts, are rare tumors that can involve the gastrointestinal tract. Initially described in 1926 by Russian pathologist Abrikossoff, the tumor can affect anatomical regions around the head, neck, and oral cavity but rarely arises in the esophagus. These tumors are generally benign, neurogenic in origin, and esophageal involvement only has an incidence of approximately 33 per 100,000. The mean age of diagnosis is 45 years, with lesions more commonly found in men, but should be considered in women presenting with an intramural mass at the proximal or distal third of the esophagus. Dysphagia is a common symptom seen in 33% of patients with these tumors, while the rest are asymptomatic. Esophageal granular cell tumors do have malignant potential and must be monitored closely.
Case Description/
Methods: In this case, a 57-year-old Caucasian female with a past medical history of gastroesophageal reflux disease (GERD) presented to the gastroenterology clinic for evaluation of intermittent worsening dysphagia with acid reflux. Subsequently, an upper endoscopy showed a nodule in the lower third of the esophagus, and diffuse mild inflammation with erythema in the gastric body and antrum. The esophageal biopsies were positive for S-100 on immunohistochemistry, a protein marker of neural crest origin and gastric biopsies were positive for Helicobacter pylori (H. pylori). An upper endoscopic ultrasound (EUS) demonstrated an eight mm in thickness hypoechoic and submucosal lesion with well-defined borders in the lower third of the esophagus. Endoscopic mucosal resection (EMR) was then performed with complete removal. Pathology from the resected lesion demonstrated an underlying population of neoplastic cells, with strong S100 and CD68 positivity confirming the diagnosis of a granular cell tumor. The patient was also treated with bismuth-based quadruple therapy for coincidental H. pylori infection and omeprazole.
Discussion: As previously discussed, there is a potential for granular cell tumors to become malignant. Monitoring with EUS is critical in determining the choice of treatment. Small (< 1cm) lesions are managed conservatively, and larger lesions ( >1cm) are resected endoscopically. In this case, the patient still underwent EMR since the lesion was causing dysphagia. Diagnosis, work-up, and long-term management have not been well described due to the tumor’s rarity.
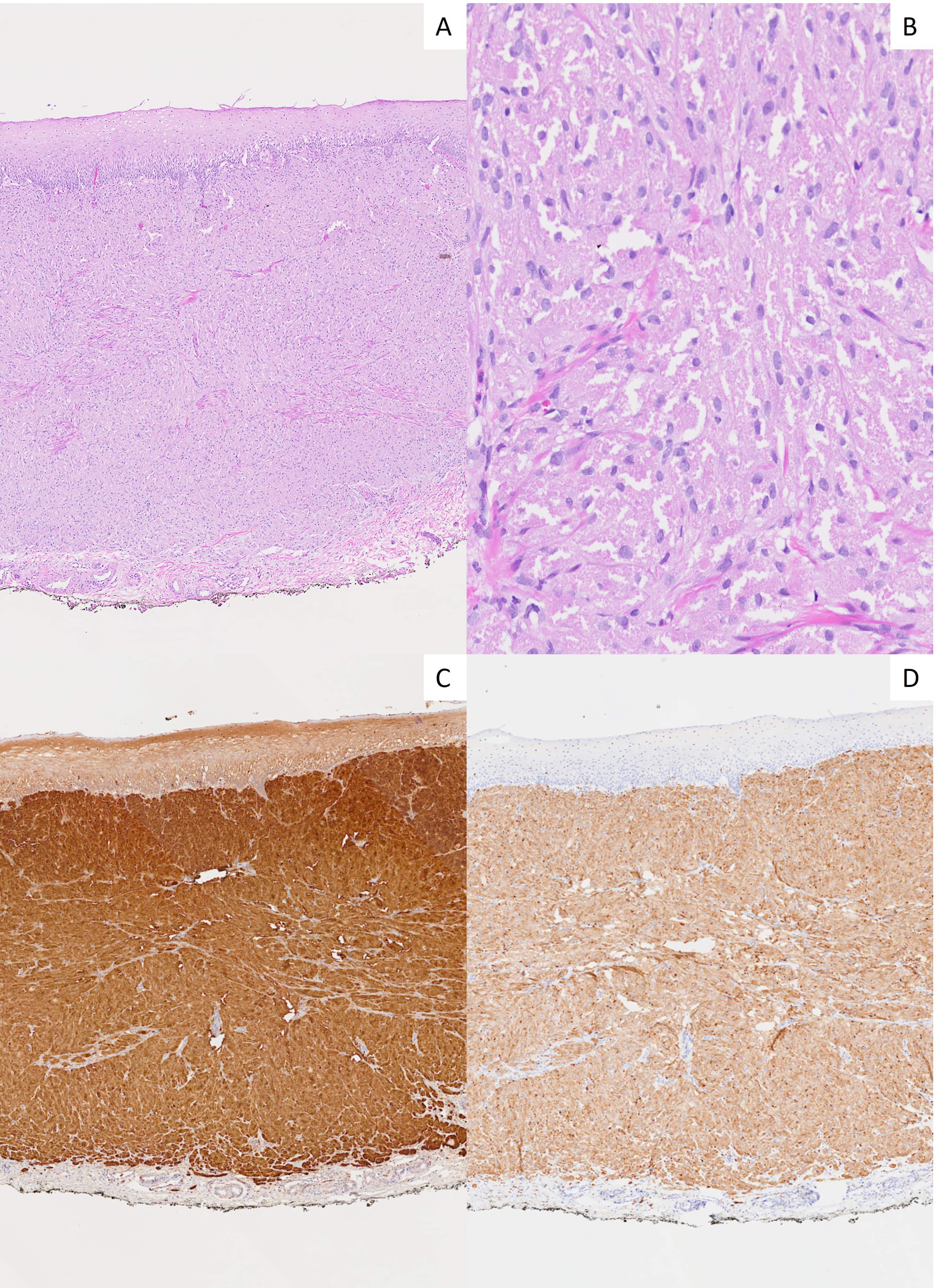
Figure: Image 1: Endoscopic views of a single eight mm (subepithelial) nodule in the lower third of the esophagus.
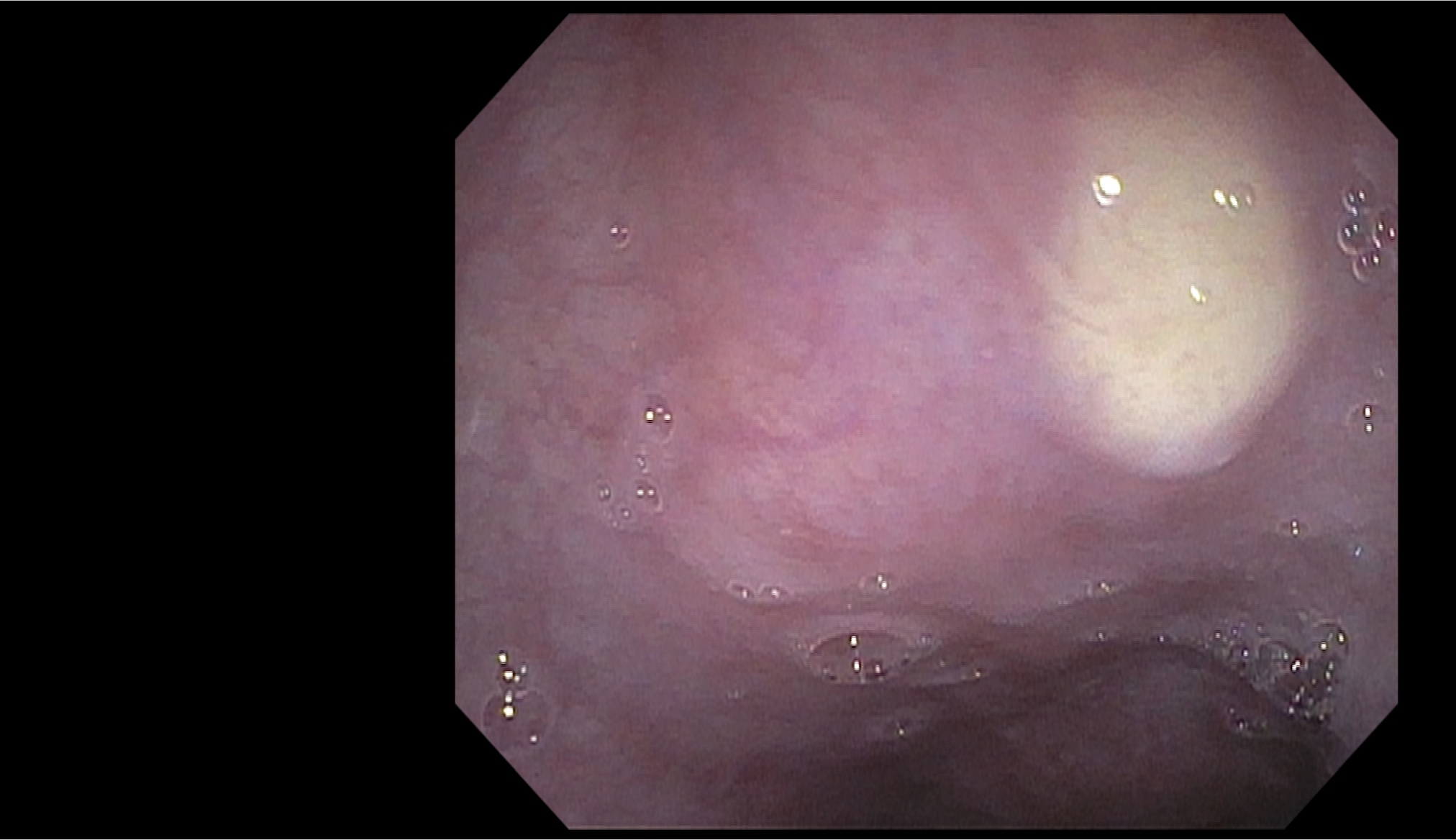
Figure: Image 2: Histopathologic digital images of an esophageal nodule: (A) H&E stain at 2x magnification reveals esophageal mucosa with an underlying population of neoplastic cells. (B) H&E stain at 20x magnification displays characteristic sheets or packets of uniform epithelioid cells with abundant eosinophilic granular cytoplasm and small nuclei. Immunohistochemical staining of the neoplastic cells demonstrates diffuse, strong S100 positivity (C) and CD68 positivity (D), both shown at 2x.
Disclosures:
Carlos Diola indicated no relevant financial relationships.
Mantej Sehmbhi indicated no relevant financial relationships.
Edward Lung indicated no relevant financial relationships.
Ian Cohen indicated no relevant financial relationships.
Alexandra Rozalen indicated no relevant financial relationships.
Abdelsalam Sharabi indicated no relevant financial relationships.
Carlos G. Diola, MD1, Mantej Sehmbhi, MBBS2, Edward Lung, MD3, Ian Cohen, MD3, Alexandra Rozalen, MD3, Abdelsalam Sharabi, MD3. P2868 - A Cryptic Esophageal Lesion: Benign or Malignant?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
