Monday Poster Session
Category: Esophagus
P2865 - Moving the Needle: A Rare Case of an Esophageal Perforation by a Retained Needle After Cardiothoracic Surgery
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vincent J. Maffei, MD, PhD (he/him/his)
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Vincent J. Maffei, MD, PhD, Steven B. Clayton, MD
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Surgical device retention after cardiothoracic surgery is a rare complication that can injure vital structures within the mediastinum, including the esophagus. We present a case of an iatrogenic thoracic foreign body responsible for simultaneous aortic and esophageal perforations.
Case Description/
Methods: The patient is an 84 year old male veteran with a history of coronary artery bypass grafting decades prior who presented to the Emergency Department for subacute, left-sided chest pain with onset the week prior. His evaluation for acute coronary syndrome was unrevealing, and his vitals were clinically stable. His chest x-ray noted a thin, linear, 5 cm, retrocardiac foreign body. Cross-sectional imaging by computed tomography revealed a needle spanning the anterior wall of the descending aorta and the posterior wall of the esophagus. An esophagogastroduodenoscopy (EGD) and endoscopic ultrasound showed no injury to the esophageal lumen or wall of the aorta, respectively. The patient’s symptoms improved with conservative management, and he requested early discharge with follow up. He presented again 2 weeks later with progressed chest pain, and updated cross-sectional imaging revealed anterosuperior migration of the needle resulting in violation of the anterior wall of the descending aorta and through-and-through penetration of the esophagus (Figure 1) with termination of the needle at the left mainstem bronchus. A repeat EGD confirmed a thin, metallic foreign body traversing the anterior and posterior esophageal walls (Figure 2). The patient underwent urgent repeat sternotomy with cardiopulmonary bypass for needle removal and repair of the associated aortic wall defect. The esophageal perforation, free of the foreign body, was re-inspected on intraoperative EGD, and no further complication was noted. A nasogastric tube was placed to suction, and the patient was brought back to the post-surgical floor in stable condition. His post-operative course was complicated by oropharyngeal dysphagia and deconditioning necessitating rehabilitation.
Discussion: Historical cases of retained surgical materials have motivated the advancement of operating room safety protocols to curb this avoidable complication. This case highlights that symptoms of iatrogenic foreign bodies may not manifest until many years after the index surgery. The decision to remove a foreign body must carefully balance the perceived harm reduction by removal against the risks imposed by a second major surgery.
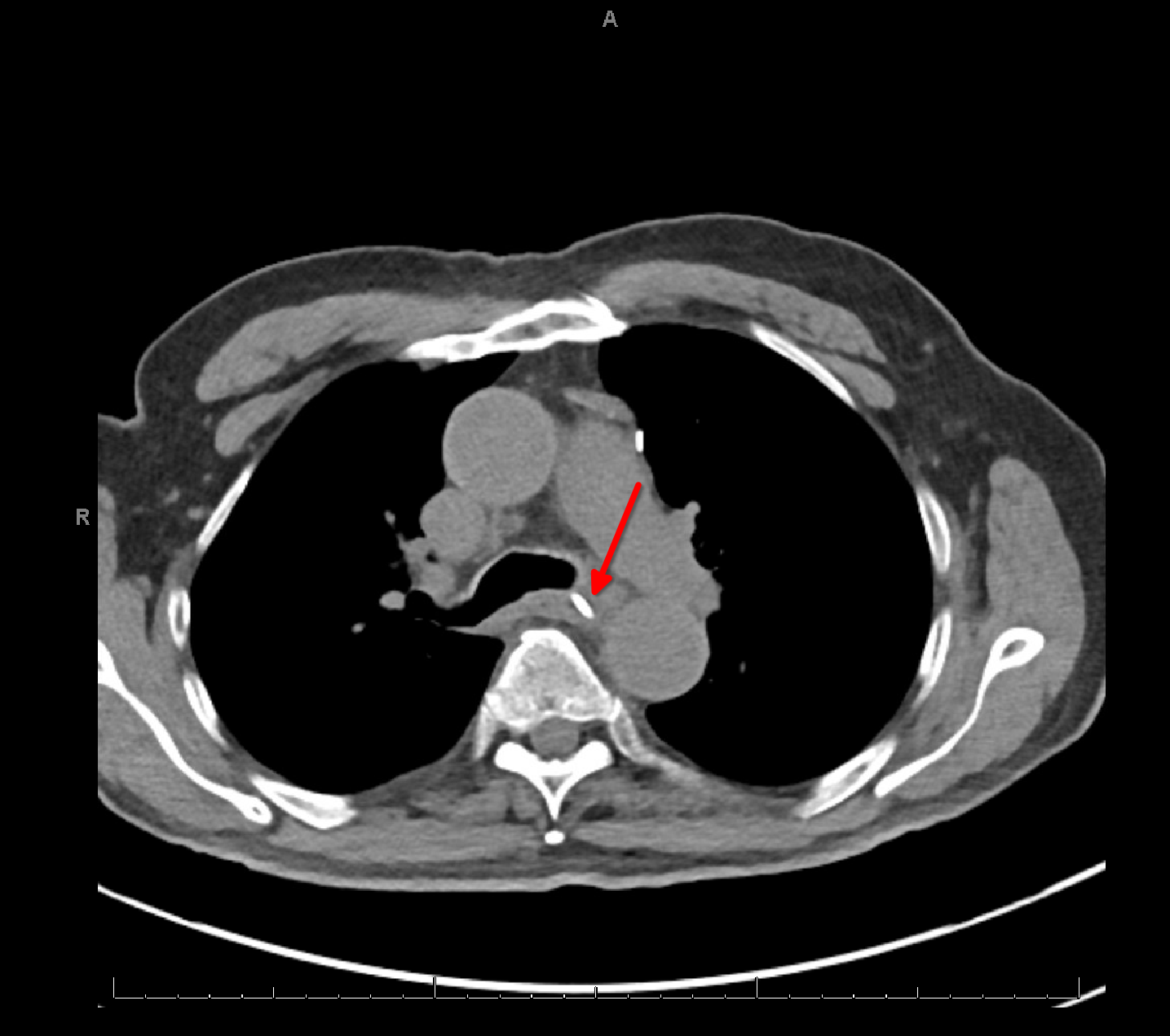
Figure: A computed tomography cross-section at the level of the carina shows a linear foreign body (red arrow) traversing the esophagus.
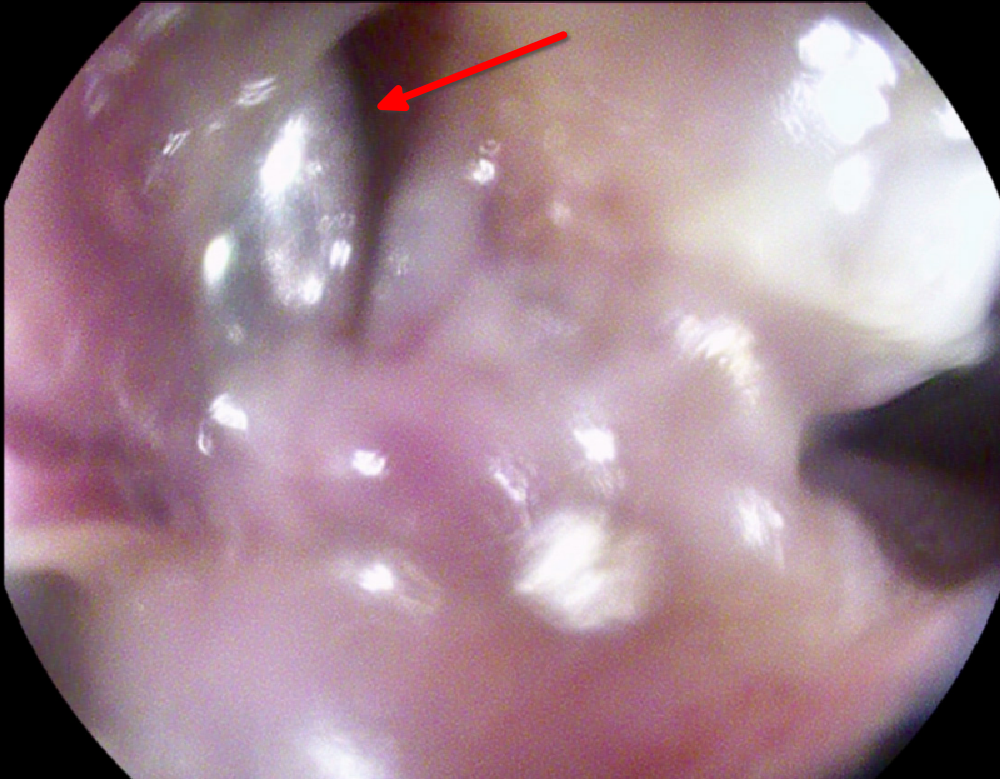
Figure: An esophagogastroduodenoscopy intraprocedural photo confirms a thin metallic foreign body (red arrow) penetrating the esophageal luminal walls.
Disclosures:
Vincent Maffei indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Vincent J. Maffei, MD, PhD, Steven B. Clayton, MD. P2865 - Moving the Needle: A Rare Case of an Esophageal Perforation by a Retained Needle After Cardiothoracic Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Surgical device retention after cardiothoracic surgery is a rare complication that can injure vital structures within the mediastinum, including the esophagus. We present a case of an iatrogenic thoracic foreign body responsible for simultaneous aortic and esophageal perforations.
Case Description/
Methods: The patient is an 84 year old male veteran with a history of coronary artery bypass grafting decades prior who presented to the Emergency Department for subacute, left-sided chest pain with onset the week prior. His evaluation for acute coronary syndrome was unrevealing, and his vitals were clinically stable. His chest x-ray noted a thin, linear, 5 cm, retrocardiac foreign body. Cross-sectional imaging by computed tomography revealed a needle spanning the anterior wall of the descending aorta and the posterior wall of the esophagus. An esophagogastroduodenoscopy (EGD) and endoscopic ultrasound showed no injury to the esophageal lumen or wall of the aorta, respectively. The patient’s symptoms improved with conservative management, and he requested early discharge with follow up. He presented again 2 weeks later with progressed chest pain, and updated cross-sectional imaging revealed anterosuperior migration of the needle resulting in violation of the anterior wall of the descending aorta and through-and-through penetration of the esophagus (Figure 1) with termination of the needle at the left mainstem bronchus. A repeat EGD confirmed a thin, metallic foreign body traversing the anterior and posterior esophageal walls (Figure 2). The patient underwent urgent repeat sternotomy with cardiopulmonary bypass for needle removal and repair of the associated aortic wall defect. The esophageal perforation, free of the foreign body, was re-inspected on intraoperative EGD, and no further complication was noted. A nasogastric tube was placed to suction, and the patient was brought back to the post-surgical floor in stable condition. His post-operative course was complicated by oropharyngeal dysphagia and deconditioning necessitating rehabilitation.
Discussion: Historical cases of retained surgical materials have motivated the advancement of operating room safety protocols to curb this avoidable complication. This case highlights that symptoms of iatrogenic foreign bodies may not manifest until many years after the index surgery. The decision to remove a foreign body must carefully balance the perceived harm reduction by removal against the risks imposed by a second major surgery.
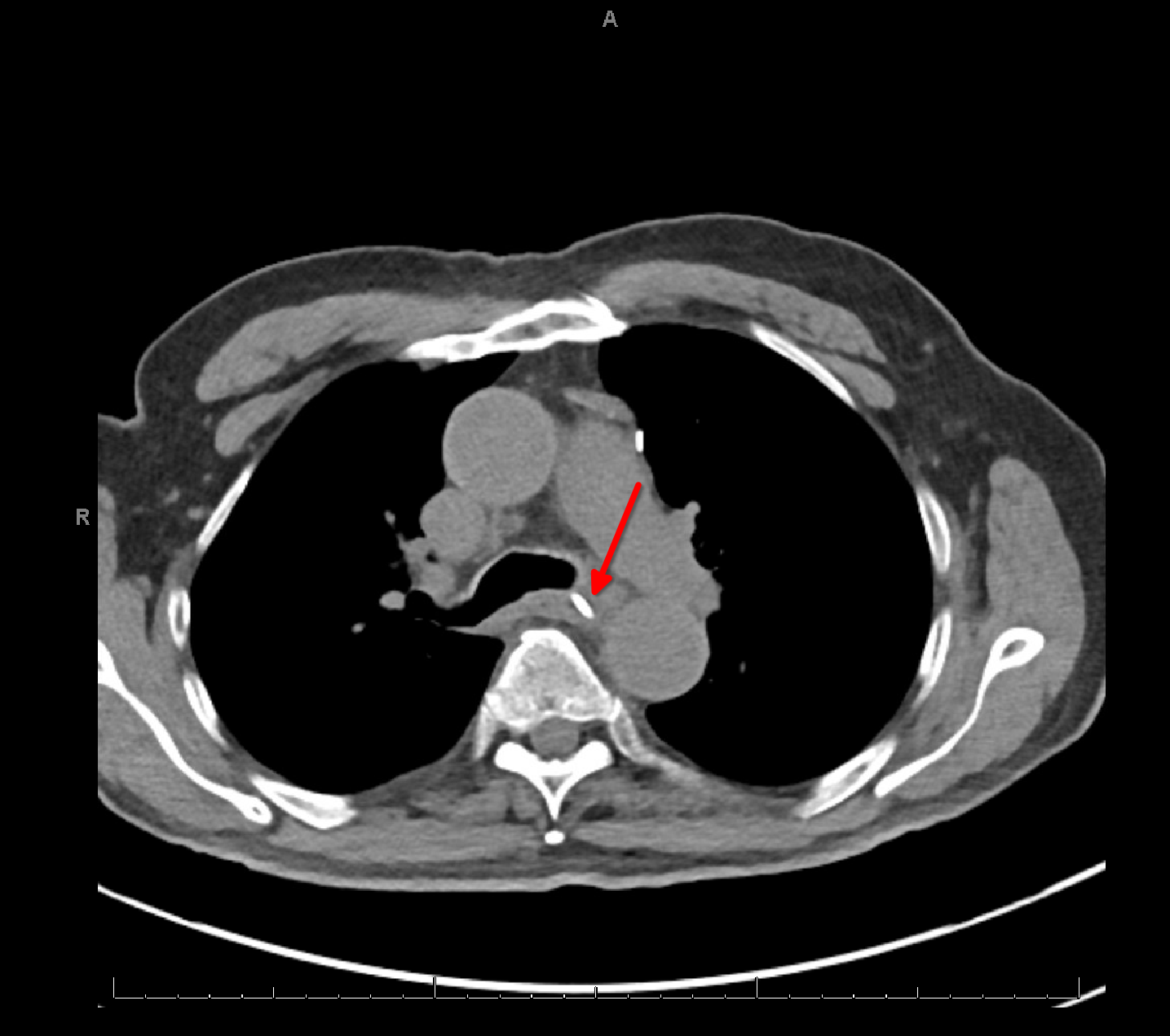
Figure: A computed tomography cross-section at the level of the carina shows a linear foreign body (red arrow) traversing the esophagus.
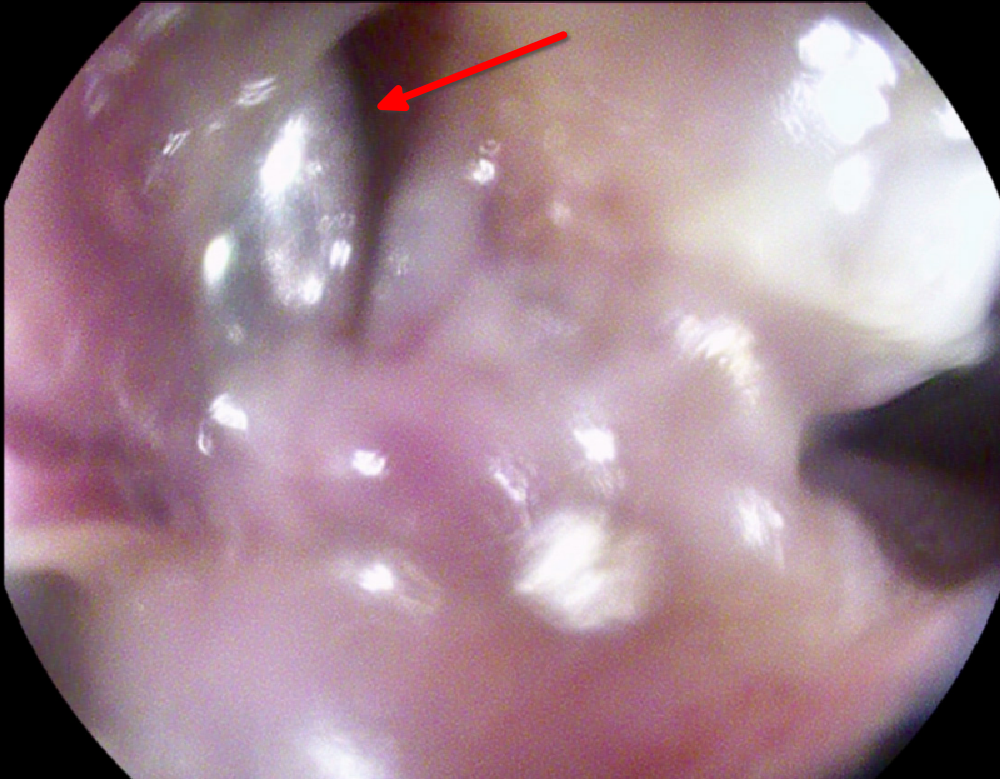
Figure: An esophagogastroduodenoscopy intraprocedural photo confirms a thin metallic foreign body (red arrow) penetrating the esophageal luminal walls.
Disclosures:
Vincent Maffei indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Vincent J. Maffei, MD, PhD, Steven B. Clayton, MD. P2865 - Moving the Needle: A Rare Case of an Esophageal Perforation by a Retained Needle After Cardiothoracic Surgery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
