Monday Poster Session
Category: Esophagus
P2863 - Rare Tumor, Rare Route: Diagnosing a Mediastinal Yolk Sac Tumor via Endoscopy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hootan Vakili, MD (he/him/his)
Broward Health North
Boca Raton, FL
Presenting Author(s)
Hootan Vakili, MD1, Mina Ayad, MD2, Gautam Anand, MD2, Keshavi Mahesh, MD2, Satya Singh, MD3
1Broward Health North, Boca Raton, FL; 2Broward Health North, Pompano Beach, FL; 3Broward Health Medical Center, Fort Lauderdale, FL
Introduction: Primary mediastinal germ cell tumors (PMGCTs) are rare, accounting for only 1%–4% of all mediastinal masses. Yolk sac tumors, a subtype of non-seminomatous germ cell tumors, most commonly arise in the gonads, with extragonadal occurrences primarily seen in the mediastinum or retroperitoneum. Direct esophageal invasion by such tumors is extremely uncommon, and diagnosis via EGD is exceedingly rare. We present a unique case of a primary mediastinal yolk sac tumor with direct esophageal involvement diagnosed by upper endoscopy in a young adult male presenting with progressive dysphagia.
Case Description/
Methods: A 34-year-old male warehouse worker with a history of obesity and prior tobacco use presented with a four-month history of progressively worsening dysphagia, initially to solids and eventually to liquids.
CTA of the chest demonstrated a large heterogeneous mass in the subcarinal and middle mediastinum with internal air, concerning for communication with the esophagus or superimposed infection.
EGD was performed and revealed a single, fungating, ulcerated, and invasive mass measuring approximately 9 mm in the middle third of the esophagus. Biopsies of the lesion were obtained.
Histologic examination revealed malignant neoplastic cells consistent with a germ cell tumor showing yolk sac (endodermal sinus tumor) differentiation.
Serum AFP level was markedly elevated at 797.86 ng/mL, further supporting the diagnosis. Testicular ultrasound showed no evidence of a gonadal primary, confirming the mediastinum as the primary site of disease.
Discussion: Primary mediastinal yolk sac tumors are rare and typically affect young adult males. They most often present with nonspecific symptoms such as chest pain, cough, dyspnea, or superior vena cava syndrome. Gastrointestinal symptoms, particularly dysphagia, are highly atypical and usually occur only in cases with direct tumor invasion into the esophagus—a rare phenomenon.
In this case, progressive dysphagia was the key symptom leading to diagnostic evaluation. While CT imaging raised suspicion for malignancy, the diagnosis was confiremd via endoscopic biopsy—an uncommon route for identifying PMGCTs, as they typically do not involve the esophageal mucosa.
This case highlights the importance of considering mediastinal tumors in the differential diagnosis of unexplained dysphagia, especially in young male patients. It also underscores the diagnostic value of EGD in atypical cases and expands the clinical spectrum of PMGCTs with esophageal involvement.

Figure: Chest CT revealing a large soft tissue lesion in the subcarinal and middle mediastinal region
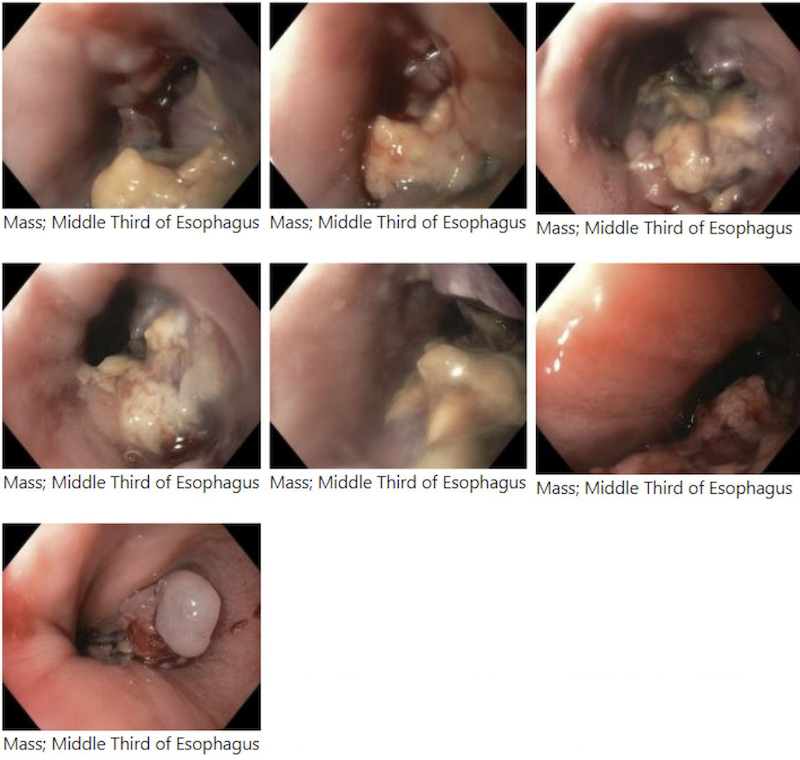
Figure: EGD images revealing a 9 mm fungating, ulcerated, and invasive mass in the middle third of the esophagus.
Disclosures:
Hootan Vakili indicated no relevant financial relationships.
Mina Ayad indicated no relevant financial relationships.
Gautam Anand indicated no relevant financial relationships.
Keshavi Mahesh indicated no relevant financial relationships.
Satya Singh indicated no relevant financial relationships.
Hootan Vakili, MD1, Mina Ayad, MD2, Gautam Anand, MD2, Keshavi Mahesh, MD2, Satya Singh, MD3. P2863 - Rare Tumor, Rare Route: Diagnosing a Mediastinal Yolk Sac Tumor via Endoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Broward Health North, Boca Raton, FL; 2Broward Health North, Pompano Beach, FL; 3Broward Health Medical Center, Fort Lauderdale, FL
Introduction: Primary mediastinal germ cell tumors (PMGCTs) are rare, accounting for only 1%–4% of all mediastinal masses. Yolk sac tumors, a subtype of non-seminomatous germ cell tumors, most commonly arise in the gonads, with extragonadal occurrences primarily seen in the mediastinum or retroperitoneum. Direct esophageal invasion by such tumors is extremely uncommon, and diagnosis via EGD is exceedingly rare. We present a unique case of a primary mediastinal yolk sac tumor with direct esophageal involvement diagnosed by upper endoscopy in a young adult male presenting with progressive dysphagia.
Case Description/
Methods: A 34-year-old male warehouse worker with a history of obesity and prior tobacco use presented with a four-month history of progressively worsening dysphagia, initially to solids and eventually to liquids.
CTA of the chest demonstrated a large heterogeneous mass in the subcarinal and middle mediastinum with internal air, concerning for communication with the esophagus or superimposed infection.
EGD was performed and revealed a single, fungating, ulcerated, and invasive mass measuring approximately 9 mm in the middle third of the esophagus. Biopsies of the lesion were obtained.
Histologic examination revealed malignant neoplastic cells consistent with a germ cell tumor showing yolk sac (endodermal sinus tumor) differentiation.
Serum AFP level was markedly elevated at 797.86 ng/mL, further supporting the diagnosis. Testicular ultrasound showed no evidence of a gonadal primary, confirming the mediastinum as the primary site of disease.
Discussion: Primary mediastinal yolk sac tumors are rare and typically affect young adult males. They most often present with nonspecific symptoms such as chest pain, cough, dyspnea, or superior vena cava syndrome. Gastrointestinal symptoms, particularly dysphagia, are highly atypical and usually occur only in cases with direct tumor invasion into the esophagus—a rare phenomenon.
In this case, progressive dysphagia was the key symptom leading to diagnostic evaluation. While CT imaging raised suspicion for malignancy, the diagnosis was confiremd via endoscopic biopsy—an uncommon route for identifying PMGCTs, as they typically do not involve the esophageal mucosa.
This case highlights the importance of considering mediastinal tumors in the differential diagnosis of unexplained dysphagia, especially in young male patients. It also underscores the diagnostic value of EGD in atypical cases and expands the clinical spectrum of PMGCTs with esophageal involvement.

Figure: Chest CT revealing a large soft tissue lesion in the subcarinal and middle mediastinal region
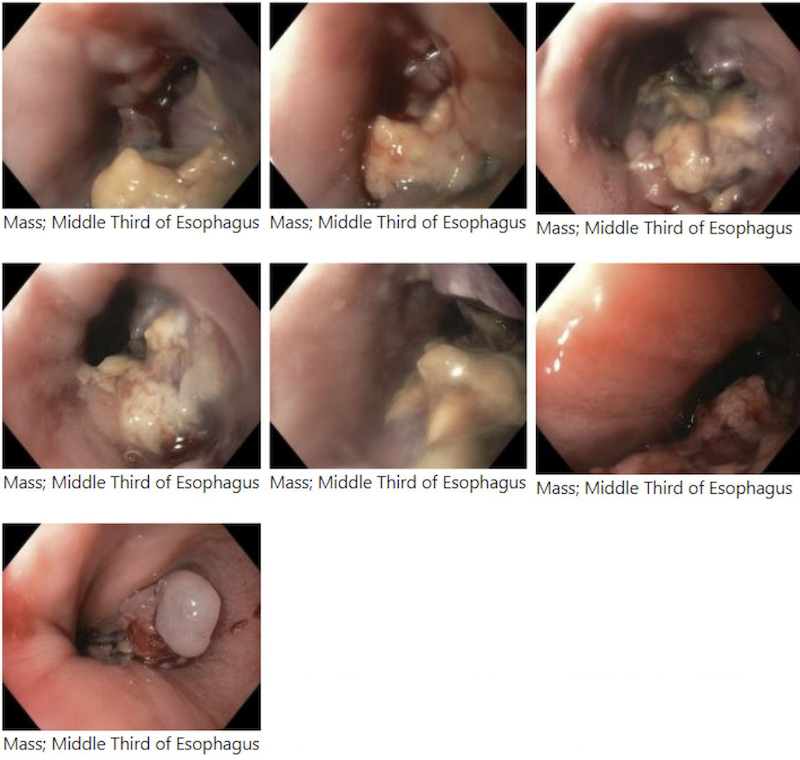
Figure: EGD images revealing a 9 mm fungating, ulcerated, and invasive mass in the middle third of the esophagus.
Disclosures:
Hootan Vakili indicated no relevant financial relationships.
Mina Ayad indicated no relevant financial relationships.
Gautam Anand indicated no relevant financial relationships.
Keshavi Mahesh indicated no relevant financial relationships.
Satya Singh indicated no relevant financial relationships.
Hootan Vakili, MD1, Mina Ayad, MD2, Gautam Anand, MD2, Keshavi Mahesh, MD2, Satya Singh, MD3. P2863 - Rare Tumor, Rare Route: Diagnosing a Mediastinal Yolk Sac Tumor via Endoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
