Monday Poster Session
Category: Esophagus
P2857 - Ectopic Pancreas at the Crossroads: A Rare Case at the Gastroesophageal Junction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Khadija Khan, MD
LSU Health Shreveport
Shreveport, LA
Presenting Author(s)
Khadija Khan, MD1, Omar Khan, MD1, Qiang Cai, MD, PhD, MACG2
1LSU Health Shreveport, Shreveport, LA; 2LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: Pancreatic heterotopia, also known as pancreatic rest, is a rare congenital anomaly characterized by the presence of ectopic pancreatic tissue that lacks anatomical or vascular continuity with the main pancreas. This ectopic tissue possesses its own distinct ductal and vascular supply and can contain acinar, ductal, and occasionally islet cells. Autopsy studies estimate its prevalence to range from 0.55% to 13.7%, though it is typically asymptomatic and often discovered incidentally. The most common sites of pancreatic heterotopia include the gastric antrum, duodenum, and proximal jejunum. In contrast, heterotopic pancreas occurring in the esophagus, particularly at the gastroesophageal (GE) junction, is exceedingly rare, with only six cases reported in the literature to date. Here, we present a unique case of pancreatic heterotopia at the GE junction, contributing to the limited body of literature on this unusual presentation.
Case Description/
Methods: A 53-year-old South Asian male presented with progressively worsening intermittent dyspepsia and reflux symptoms, despite ongoing proton pump inhibitor (PPI) therapy. Esophagogastroduodenoscopy (EGD) revealed an irregular Z line and a small mucosal nodule extending above the GE junction. Barrett’s esophagus was initially suspected. However, histopathological examination of the biopsy demonstrated squamous mucosa with a well-defined nest of pancreatic tissue, consistent with pancreatic heterotopia at the GE junction. The remainder of the esophagus, stomach, and duodenum appeared normal. The patient was continued on PPI therapy, with a plan for close endoscopic surveillance given the rare location of the heterotopic tissue and ongoing symptoms.
Discussion: Ectopic pancreatic tissue is usually an incidental finding on EGD, typically presenting as a submucosal nodule with a characteristic central umbilication. Although the majority of cases are asymptomatic, some patients may experience symptoms like epigastric pain, heartburn, dysphagia, or in rare cases, luminal obstruction. Complications arising from ectopic pancreatic tissue such as acute or chronic pancreatitis, pseudocyst formation, abscess, or even malignant transformation are uncommon but have been reported. There are no established guidelines for the management of pancreatic rest. Treatment is generally guided by lesion size, location, and symptoms. Treatment can range from observation with medical therapy to more invasive approaches like resection, and in select cases, esophagectomy.
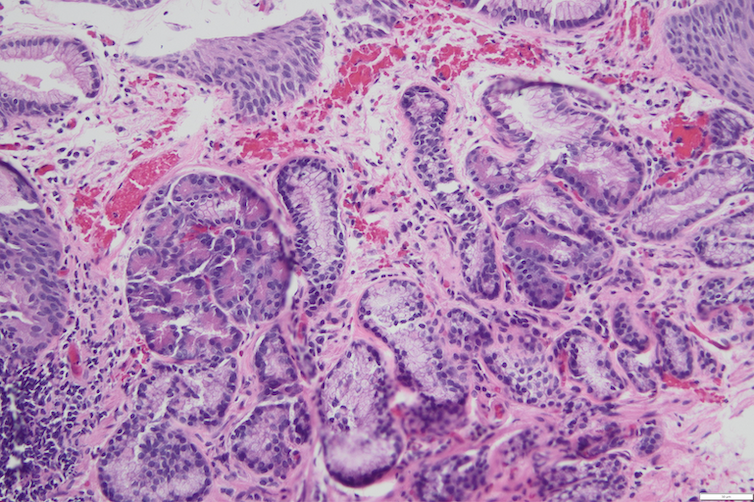
Figure: Squamous mucosa with nests of pancreatic tissue in the lamina propria ( H&E stain, 200X magnification)
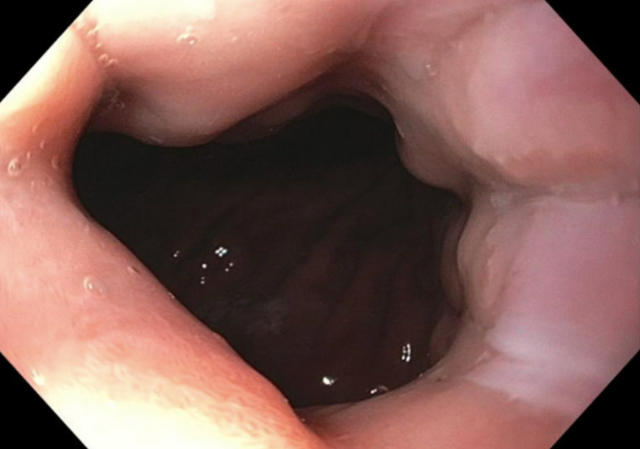
Figure: Upper gastrointestinal endoscopy revealed a slightly raised area of abnormal mucosa at the gastroesophageal juction that was biopsied to rule out Barrett's
Disclosures:
Khadija Khan indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Khadija Khan, MD1, Omar Khan, MD1, Qiang Cai, MD, PhD, MACG2. P2857 - Ectopic Pancreas at the Crossroads: A Rare Case at the Gastroesophageal Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1LSU Health Shreveport, Shreveport, LA; 2LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: Pancreatic heterotopia, also known as pancreatic rest, is a rare congenital anomaly characterized by the presence of ectopic pancreatic tissue that lacks anatomical or vascular continuity with the main pancreas. This ectopic tissue possesses its own distinct ductal and vascular supply and can contain acinar, ductal, and occasionally islet cells. Autopsy studies estimate its prevalence to range from 0.55% to 13.7%, though it is typically asymptomatic and often discovered incidentally. The most common sites of pancreatic heterotopia include the gastric antrum, duodenum, and proximal jejunum. In contrast, heterotopic pancreas occurring in the esophagus, particularly at the gastroesophageal (GE) junction, is exceedingly rare, with only six cases reported in the literature to date. Here, we present a unique case of pancreatic heterotopia at the GE junction, contributing to the limited body of literature on this unusual presentation.
Case Description/
Methods: A 53-year-old South Asian male presented with progressively worsening intermittent dyspepsia and reflux symptoms, despite ongoing proton pump inhibitor (PPI) therapy. Esophagogastroduodenoscopy (EGD) revealed an irregular Z line and a small mucosal nodule extending above the GE junction. Barrett’s esophagus was initially suspected. However, histopathological examination of the biopsy demonstrated squamous mucosa with a well-defined nest of pancreatic tissue, consistent with pancreatic heterotopia at the GE junction. The remainder of the esophagus, stomach, and duodenum appeared normal. The patient was continued on PPI therapy, with a plan for close endoscopic surveillance given the rare location of the heterotopic tissue and ongoing symptoms.
Discussion: Ectopic pancreatic tissue is usually an incidental finding on EGD, typically presenting as a submucosal nodule with a characteristic central umbilication. Although the majority of cases are asymptomatic, some patients may experience symptoms like epigastric pain, heartburn, dysphagia, or in rare cases, luminal obstruction. Complications arising from ectopic pancreatic tissue such as acute or chronic pancreatitis, pseudocyst formation, abscess, or even malignant transformation are uncommon but have been reported. There are no established guidelines for the management of pancreatic rest. Treatment is generally guided by lesion size, location, and symptoms. Treatment can range from observation with medical therapy to more invasive approaches like resection, and in select cases, esophagectomy.
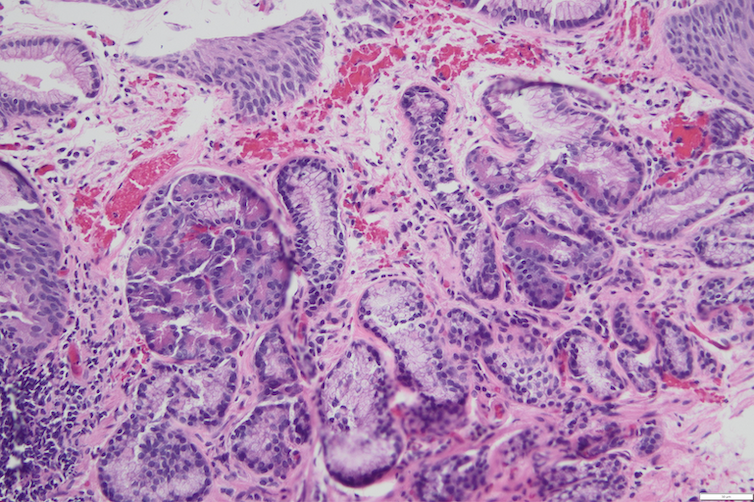
Figure: Squamous mucosa with nests of pancreatic tissue in the lamina propria ( H&E stain, 200X magnification)
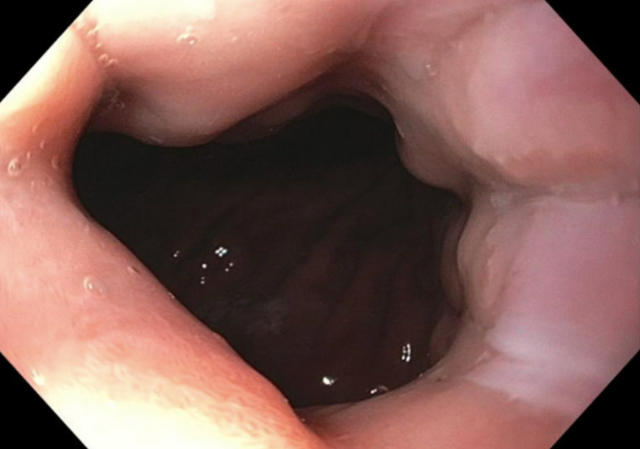
Figure: Upper gastrointestinal endoscopy revealed a slightly raised area of abnormal mucosa at the gastroesophageal juction that was biopsied to rule out Barrett's
Disclosures:
Khadija Khan indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Khadija Khan, MD1, Omar Khan, MD1, Qiang Cai, MD, PhD, MACG2. P2857 - Ectopic Pancreas at the Crossroads: A Rare Case at the Gastroesophageal Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
