Monday Poster Session
Category: Esophagus
P2856 - Chronic Tracheoesophageal Fistula to Native Esophagus After Colonic Interposition
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Roma Ahuja, MD
Baylor University Medical Center
Dallas, TX
Presenting Author(s)
Roma Ahuja, MD1, Kenneth Ford, MD1, Ashton Ellison, MBChB2, Eitan Podgaetz, MD1, Anh Nguyen, MD2
1Baylor University Medical Center, Dallas, TX; 2Center for Esophageal Diseases, Baylor University Medical Center, Dallas, TX
Introduction: A tracheoesophageal fistula (TEF) is an aberrant connection between the trachea and esophagus that can result in aspiration events and recurrent pneumonias. TEF can be congenital in nature (i.e., esophageal atresia) or acquired as a complication of surgery or trauma. It is treated with surgical resection of the fistula and airway repair. Esophageal repair is preferred while esophagectomy with diversion is sometimes necessary. Reconstruction techniques include colonic interposition whereby a portion of the colon is anastomosed to the proximal esophagus and stomach. We present a case where the native esophagus was ligated and left in-situ and a right sided colonic interposition was done. The native esophagus led to formation of a TEF.
Case Description/
Methods: A 45-year-old female had a traumatic injury at age 6 resulting in tracheal and esophageal rupture. She underwent right colonic interposition to her proximal esophagus. Her native esophagus was ligated proximally just distal to the esophago-colic anastomosis and distally at the gastro-esophageal junction. Since her colonic interposition, she had chronic bronchitis and bacterial pneumonia. A CT Chest showed a large fistula of the blind distal esophagus to the carina (Figure 1) with confirmation via bronchoscopy (Figure 2). After multidisciplinary discussion, endoscopic intervention was attempted with argon plasma coagulation (APC) ablation of the blind native esophagus mucosa with suture closure of the TEF opening and bronchial stents placed to close the two esophago-tracheal fistulas. However, repeat CT Chest showed that the TEF remained open. The risks and benefits of surgical repair was discussed with patient who decided not to pursue surgery. She is currently being managed with pulmonary hygiene measures and long-term antibiotic therapy with no recent hospitalizations.
Discussion: Though unconventional, endoscopic intervention with suture closure of the TEF was pursued due to the high-risk nature of surgery intervention, which would require a right thoracotomy with complete esophagectomy of the native esophagus and complex tracheal repair with mesh under ECMO support. Other endoscopic options for TEF closure include the use of sealants, clip closure or stent placement. This case underscores the rare occurrence of TEF development from a retained blind native esophagus located adjacent to the trachea and demonstrates potential endoscopic approaches that may be considered prior to high-risk surgical repair in challenging clinical scenarios.
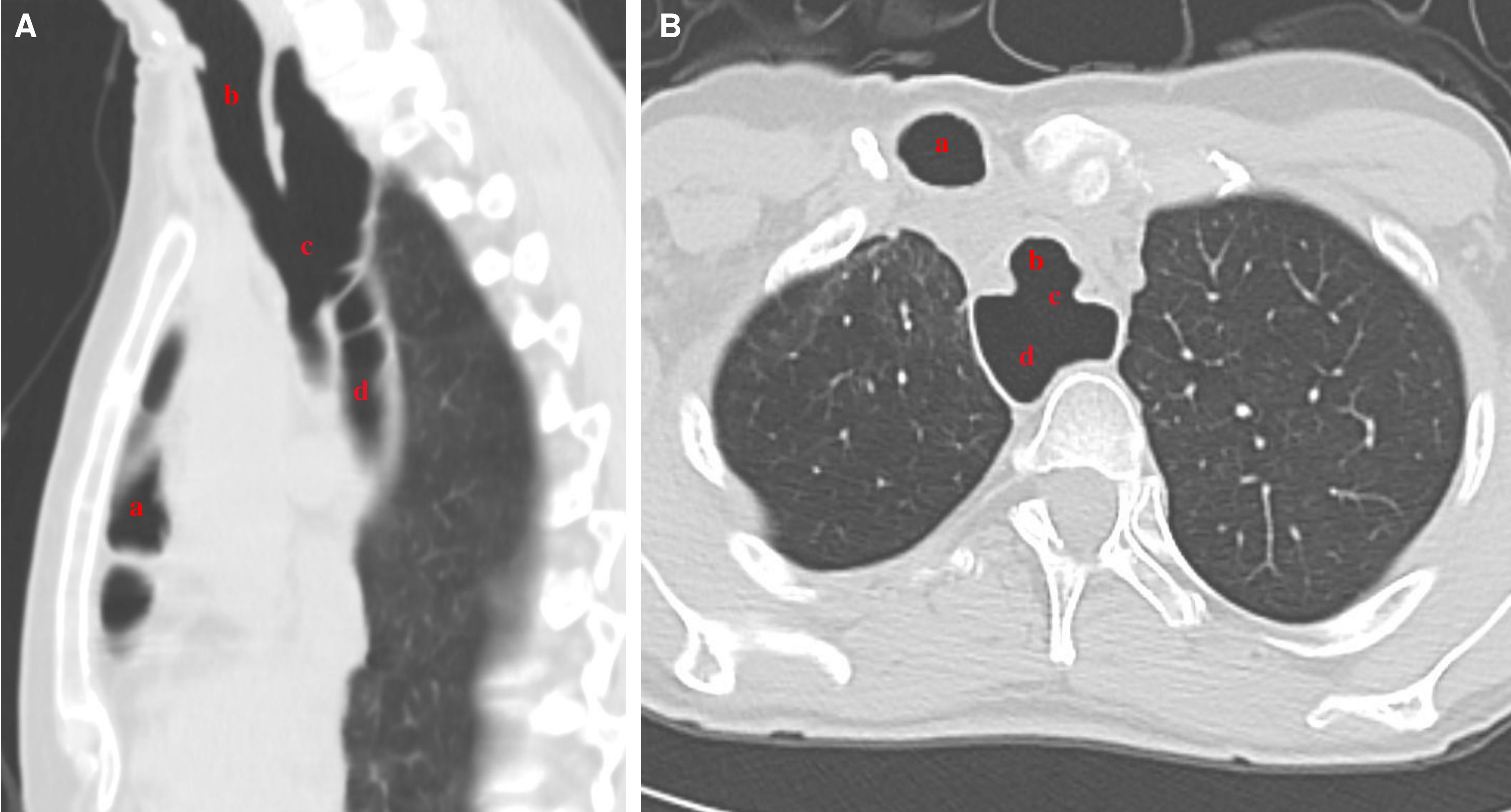
Figure: Figure 1. Pre-operative imaging of the tracheaoesophageal fistula in the sagittal (Figure 1A) and axial view (Figure 1B).
a) Colonic interposition
b) Trachea
c) TEF
d) Native distal esophagus

Figure: Figure 2: Pre-operative bronchoscopy with TEF visualized at the level of the carina.
a) Right main stem bronchus
b) TEF
Disclosures:
Roma Ahuja indicated no relevant financial relationships.
Kenneth Ford indicated no relevant financial relationships.
Ashton Ellison indicated no relevant financial relationships.
Eitan Podgaetz indicated no relevant financial relationships.
Anh Nguyen indicated no relevant financial relationships.
Roma Ahuja, MD1, Kenneth Ford, MD1, Ashton Ellison, MBChB2, Eitan Podgaetz, MD1, Anh Nguyen, MD2. P2856 - Chronic Tracheoesophageal Fistula to Native Esophagus After Colonic Interposition, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor University Medical Center, Dallas, TX; 2Center for Esophageal Diseases, Baylor University Medical Center, Dallas, TX
Introduction: A tracheoesophageal fistula (TEF) is an aberrant connection between the trachea and esophagus that can result in aspiration events and recurrent pneumonias. TEF can be congenital in nature (i.e., esophageal atresia) or acquired as a complication of surgery or trauma. It is treated with surgical resection of the fistula and airway repair. Esophageal repair is preferred while esophagectomy with diversion is sometimes necessary. Reconstruction techniques include colonic interposition whereby a portion of the colon is anastomosed to the proximal esophagus and stomach. We present a case where the native esophagus was ligated and left in-situ and a right sided colonic interposition was done. The native esophagus led to formation of a TEF.
Case Description/
Methods: A 45-year-old female had a traumatic injury at age 6 resulting in tracheal and esophageal rupture. She underwent right colonic interposition to her proximal esophagus. Her native esophagus was ligated proximally just distal to the esophago-colic anastomosis and distally at the gastro-esophageal junction. Since her colonic interposition, she had chronic bronchitis and bacterial pneumonia. A CT Chest showed a large fistula of the blind distal esophagus to the carina (Figure 1) with confirmation via bronchoscopy (Figure 2). After multidisciplinary discussion, endoscopic intervention was attempted with argon plasma coagulation (APC) ablation of the blind native esophagus mucosa with suture closure of the TEF opening and bronchial stents placed to close the two esophago-tracheal fistulas. However, repeat CT Chest showed that the TEF remained open. The risks and benefits of surgical repair was discussed with patient who decided not to pursue surgery. She is currently being managed with pulmonary hygiene measures and long-term antibiotic therapy with no recent hospitalizations.
Discussion: Though unconventional, endoscopic intervention with suture closure of the TEF was pursued due to the high-risk nature of surgery intervention, which would require a right thoracotomy with complete esophagectomy of the native esophagus and complex tracheal repair with mesh under ECMO support. Other endoscopic options for TEF closure include the use of sealants, clip closure or stent placement. This case underscores the rare occurrence of TEF development from a retained blind native esophagus located adjacent to the trachea and demonstrates potential endoscopic approaches that may be considered prior to high-risk surgical repair in challenging clinical scenarios.
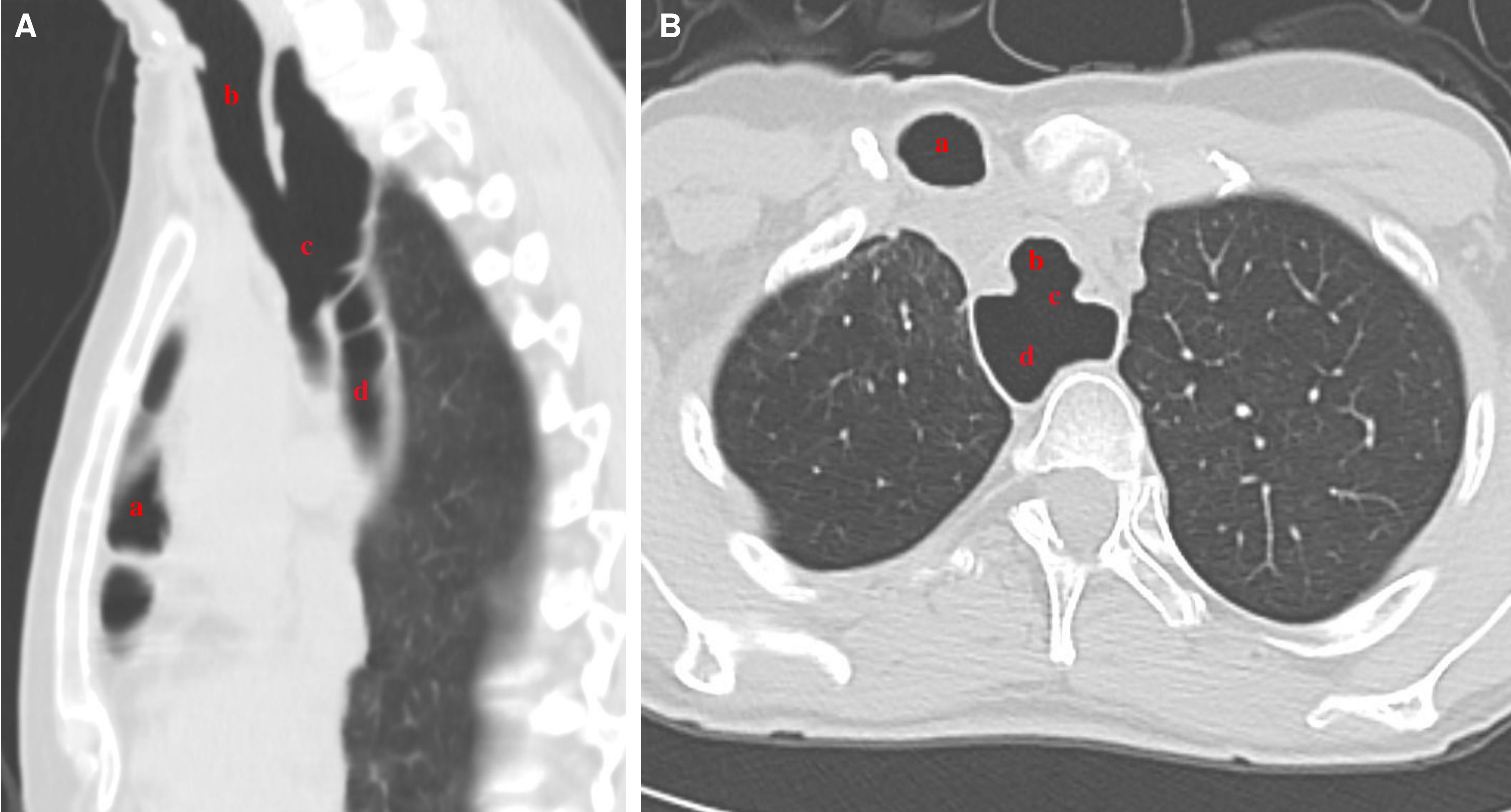
Figure: Figure 1. Pre-operative imaging of the tracheaoesophageal fistula in the sagittal (Figure 1A) and axial view (Figure 1B).
a) Colonic interposition
b) Trachea
c) TEF
d) Native distal esophagus

Figure: Figure 2: Pre-operative bronchoscopy with TEF visualized at the level of the carina.
a) Right main stem bronchus
b) TEF
Disclosures:
Roma Ahuja indicated no relevant financial relationships.
Kenneth Ford indicated no relevant financial relationships.
Ashton Ellison indicated no relevant financial relationships.
Eitan Podgaetz indicated no relevant financial relationships.
Anh Nguyen indicated no relevant financial relationships.
Roma Ahuja, MD1, Kenneth Ford, MD1, Ashton Ellison, MBChB2, Eitan Podgaetz, MD1, Anh Nguyen, MD2. P2856 - Chronic Tracheoesophageal Fistula to Native Esophagus After Colonic Interposition, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
